Supracondylar humeral fractures represent only about 0.5–1% of all fractures in adults. The objective of this study is to evaluate functional outcome and quality of life in patients treated with open reduction and internal fixation using double plates.
Material and methodsWe designed a retrospective descriptive study including 27 supracondylar humeral fractures treated with open reduction and internal fixation using two anatomic plates from January 2005 to September 2012. Mean age was 56±22.9 years including 14 female and 13 male. All fractures were classified using the AO classification. Average follow-up was of 41±23.9 months. Fracture union was evaluated with X-ray exams and functional outcome using the Mayo Elbow Performance Score (MEPS). Quality of life was evaluated using the Short Form-36 survey.
ResultsUnion at 6 months was achieved in 96% of all fractures. Average range of motion was 102° (70–140°) and average MEPS 86 points (60–100). Mean score on SF-36 was 54.87 (8.66–89.22) the older patients had lower scores. Sixty percent of patients (15 of 25) were able to return to previous activity. No infection was reported. Two patients required surgical treatment due to a stiff elbow.
ConclusionsOpen reduction and internal fixation using double plates in supracondylar humeral fractures obtains a high union rate allowing excellent functional and radiological outcomes.
Las fracturas supracondíleas de húmero representan el 0,5-1%. El objetivo de nuestro estudio es evaluar retrospectivamente el resultado funcional y la calidad de vida de los pacientes intervenidos quirúrgicamente por fractura supracondílea de húmero mediante osteosíntesis con doble placa.
Material y métodosPresentamos un estudio descriptivo retrospectivo de 27 fracturas supracondíleas de húmero tratadas quirúrgicamente mediante reducción abierta y osteosíntesis con 2 placas anatómicas, entre enero de 2005 y septiembre de 2012. La edad media de los pacientes fue de 56±22,9 años, 14 mujeres y 13 hombres. Todas las fracturas fueron tipificadas según la clasificación de la AO. El seguimiento medio fue de 41±23,9 meses. Se evaluó la consolidación de la fractura por medio de estudio radiológico y el resultado funcional mediante el Mayo Elbow Performance Score. La calidad de vida fue evaluada mediante el cuestionario SF 36.
ResultadosEl 96% de las fracturas consolidaron antes de 6 meses. El rango de movimiento medio fue de 102° (70-140°) y el Mayo Elbow Performance Score fue de 86 puntos (60-100). La puntuación media en el SF-36 fue de 54,87 (8,66-89,22), siendo las puntuaciones menores en pacientes de mayor edad. El 60% de los pacientes (15 de 25) se incorporaron a la misma actividad que realizaban antes del accidente. No hubo ningún caso de infección. Dos pacientes fueron reintervenidos por rigidez de codo.
ConclusionesLa reducción abierta y osteosíntesis con doble placa de las fracturas supracondíleas de húmero permite obtener la consolidación de la fractura en un porcentaje elevado, con buenos resultados funcionales y radiológicos.
Supracondylar humeral fractures represent 0.5–1% of all fractures in adults and 30% of elbow fractures.1 Distribution is bimodal with regards to age and mechanism of injury. In young people fractures are more commonly the consequence of high energy trauma and in the elderly low energy tauma.2
The main aim of surgical treatment is to reconstruct the articular surface of the joint. Stability and compression must also be sufficiently achieved on supracondylar level for union to occur and allow for early mobility so that the elbow may function correctly.3 The osteoporotic bone of elderly patients and conminuted articular segment are a challenge for osteosynthesis in this type of fractures. Preoperative planning, surgical approach and implant selection are factors which must be taken into account and which may affect outcome.4
Biomechanical studies have shown that osteosynthesis using double plates is more stable and more rigid than a single plate system.5,6 Regarding the positioning of the double plates, it has been observed that a parallel 2 plate structure is superior in rigidity and resistance to fatigue than the orthogonal 2 plate fixation.7–12
The most frequent complications in this type of fracture are: joint stiffness, pain and peripheral neuropathy from ulnar nerve involvement.4–13 Complications related to olecranon osteotomy have also been described.9–18,20
At present, delayed union and pseudoarthrosis are not frequent problems in this type of injury, thanks to the development of surgical technique and new osteosynthetic devices.
The aim our study was to assess the long-term radiologic and functional outcomes of open reduction and internal fixation with double plate humeral supracondylar fractures.
Material and methodsA retrospective study of 27 supracondylar humeral fracture patients who had undergone surgery between January 2005 and September 2012. Mean follow-up was 41±23.9 months. Open reduction and internal fixation was used in all cases with osteosynthesis with a parallel or orthogonal parallel double plate. Two patients (7%) died from causes unrelated to the fracture, prior to review and were therefore excluded from the study. The fractures were classified according to the AO classification system.
Mean patient age at the time of fracture was 56±22.9 years. There were 14 female patients (52%) and 13 male patients (48%). In 18 (72%) their upper left limb was affected whilst in 7 (28%) it was the right limb.
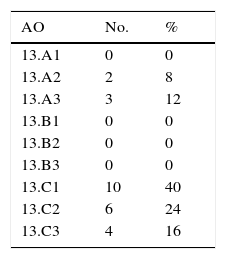
The types of fracture are listed in Table 1. The most common were type 13C (80%).
Distribution of fractures by age continues to be a bimodal distribution, with 2 peaks of age range frequencies. The mechanism of injury was a fall from the person's own height in 14 cases, and in 11 was produced as a consequence of high energy trauma (4 were traffic accidents and 7 were accident-precipitated). Two grade I open fractures were reported, according to the Gustilo classification.
All the patients underwent surgery with a peripheral nerve block and general anaesthesia, in supine lateral position with controlled ischaemia of the limb. The surgical approach was posterior in all cases. In 13 cases (52%) olecranon osteotomy was performed and in 12 (48%) there was no osteotomy (Newcastle approach).21 In our series the epitrochlear-olecranon canal was released, including the opening of the head of the flexor carpi ulnaris muscle in all cases, but the ulnar nerve was not transposed in any of them. In 22 patients the osteosynthesis plates were implanted in parallel whilst in the other 3 cases they were orthogonal. The decision between parallel or orthogonal was conditioned by the fracture characteristics and the surgeon's criterion.
All patients were given review and study data collection appointments. X-rays were performed with anteroposterior and lateral projections of the elbow and functional evaluation was made using the MEPS. The said scale considers a result of a >90 points as excellent, 75–89 points as good, 60–74 points acceptable and <60 points as bad. The patients’ quality of life was also assessed using the SF-36 test on review. We also evaluated the rate of reincorporation into normal daily activity, associated complications and surgical reintervention rate.
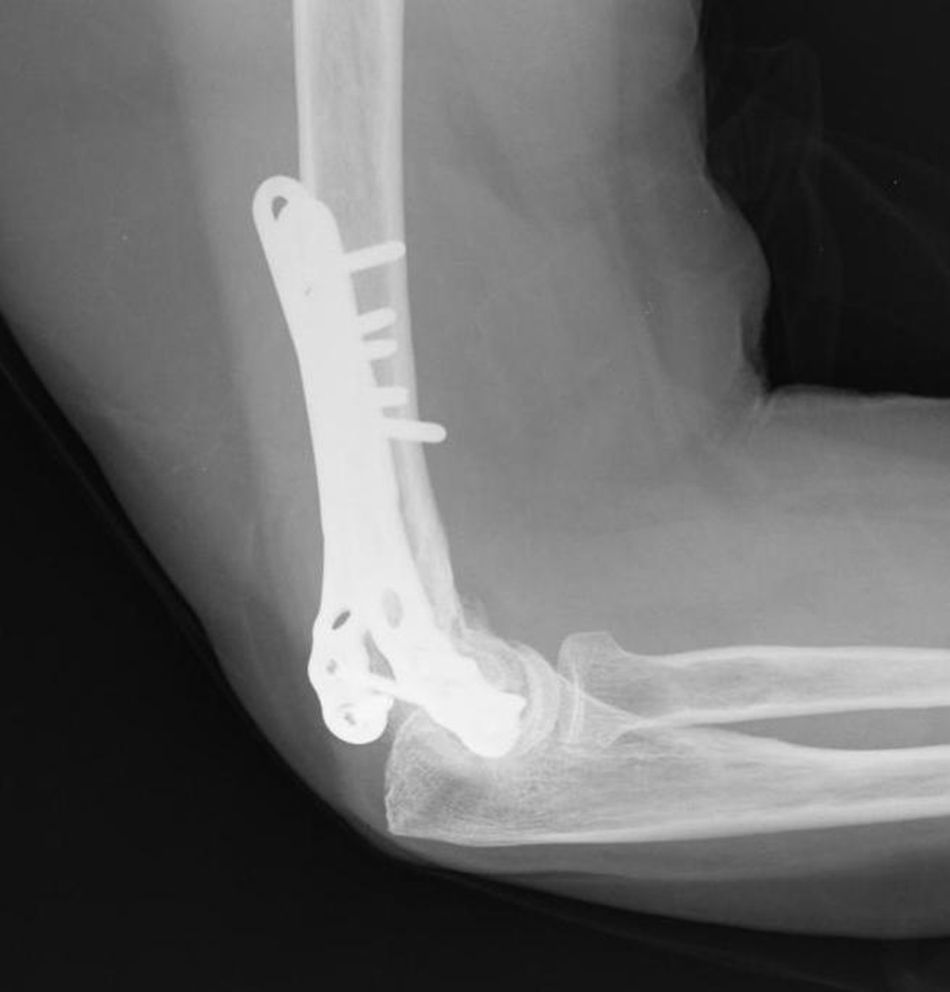
Union was considered to have been made when the patient did not mention any elbow pain and the anteroposterior X-ray and profile demonstrated signs of union (Figs. 1–4).
Newcastle approachThe incision was made 10–12cm proximal to the tip of the olecranon, along its lateral edge to the subcutaneous edge of the ulnar, 8–10cm distal from the tip of the olecranon (Fig. 5).
The 2 skin flaps were kept separate with 2 proximal sutures and 2 distal sutures.
The ulnar nerve has to be proximally identified and distally released at the level of the 2 muscle heads of the FCU muscle, with no transposing.
The fascia is opened by following the skin incision path up to the edge of the ulnar.
After this, the proximal aponeurosis is released from the raphe using a suture (Fig. 6).
The anconeus is separated from the ulnar sub-periostically and we continue in proximal direction up to the intermuscular septum of the triceps.
The raphe is opened longitudinally at proximal level and is distally retracted through a 2cm incision proximal to the olecranon.
The muscle heads of the triceps are displaced towards the lateral and medial columns of the humerus leaving the entire shoulder exposed.
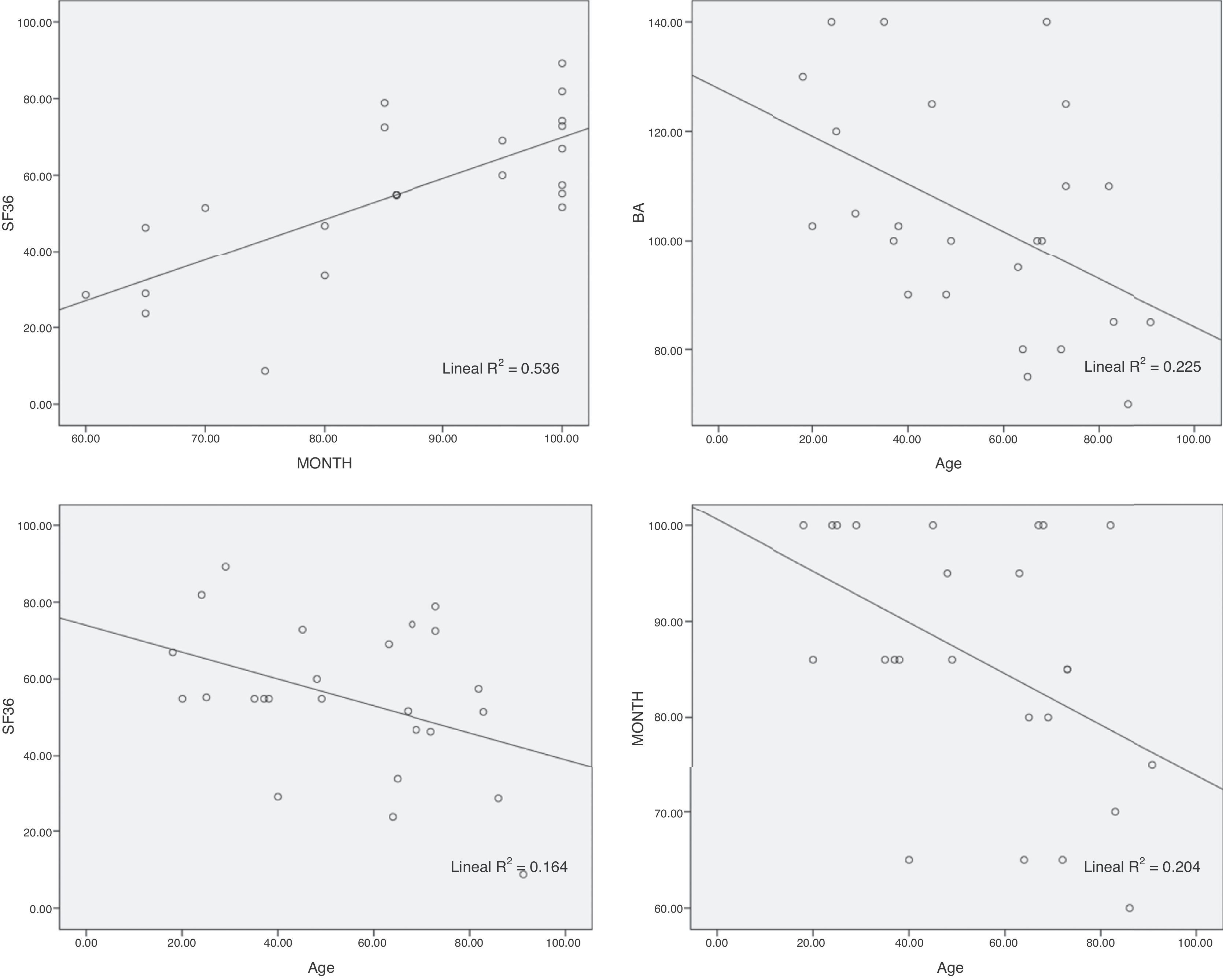
Statistical analysisResults were expressed as a percentage for qualitative variables and as mean and standard deviation for the quantitative variables. Quantitative variables (age, range of joint movement [RJM], MEPS, SF-36) were compared using lineal regression. In all comparisons a statistical level of 0.05 was used. The SPSS 19.0 (SPSS Inc., Chicago, IL, U.S.A.) programme was used for statistical analysis.
ResultsUnion was achieved of 24 fractures (96%) before 6 months had passed. Only one patient presented with a pseudoarthrosis of the fracture which required secondary surgery.
Mean RMA was 102.7° (range: 70–140°). Mean functional results according to the MEPS scale was 86 points (range: 60–100 points). In 17 patients the result was excellent, in 3 good, in 5 acceptable and in no cases was it poor.
Ten patients stated they suffered from no pain, 9 referred to mild pain and 6 to moderate pain. There was no elbow instability and there were 2 cases of elbow stiffness.
The mean SF-36 was 54.87 points (range: 8.66–89.22). 60% of patients were successfully reincorporated into their normal daily pre-fracture life activities.
The lineal regression study between MEPS and SF 36 obtained a direct relationship between functioning and quality of life (p<0.01). There was 53.6% of variability in the quality of life SF-36 questionnaire which was explained by the MEPS functioning of the patients (Fig. 7). Age was also inversely related with MEPS (p=0.023), SF-36 (p=0.045) and RMA (p=0.017). 20.4% of the MEPS, 16.4% of the SF-36 and 22.5% of the RMA were explained by age.
The presence of ulnar neuropathy was assessed at patient reviews. Sensory and motor involvement were assessed. No electromyographical study was used. Patient senses were considered to have been affected when they showed signs, however, mild, at ulnar level. No patient was affected with regards to movement. Nine patients presented with paresthesia at fifth finger level and on the palm surface of the fourth finger.
Nine patients referred to discomfort related to the osteosynthesis material. One patient presented with osteonecrosis at capitellum level 3 months after the fracture, having been asymptomatic at the time of review, and no further intervention was required. One patient presented with pseudoarthrosis at metaphysodiaphysary level, and further surgery was performed with new osteosynthesis and support from an autologous bone graft, and another patient presented with pseudoarthrosis of the olecranon osteotomy but without clinical expression.
Reintervention rate was 12% (3 cases). Two were due to elbow stiffness where open arthrolysis was practised and osteosynthesis material was removed with the consolidated fracture and the other was used to metaphysodiaphysary pseudoarthrosis.
DiscussionIn our series osteosynthesis of the supracondylar fractures was performed with parallel fixation plates in the majority of cases (23), as described in the article by Sánchez-Sotelo et al.3 Only in 3 cases were the plates fixed in orthogonal position according to the surgeon's criterion and fracture characteristics. Although the biomechanical studies showed superiority, with regards to resistance of construction, of synthesis with parallel implants, this was not expressed in vivo,7–12 and we therefore believe it necessary to adapt technique to each fracture type.
The importance of achieving stable synthesis for early mobilisation and obtainment of optimum functioning, which could guarantee better quality of life for these patients, is reflected through a direct relationship of lineal regression between functioning and quality of life (p<0.01).
Age is inversely related to MEPS (p=0.023), SF-36 (p=0.045) and RMA (p=0.017), which reflects that in the young patient quality and stability of synthesis lead to better functional recovery than in the elderly patient (Fig. 7).
Affecting the sensitivity of the ulnar nerve was the most common complication in our patient series. Although none of the patients presented with motory problems, 9 of them (36%) presented with paresthesias in the ulnar region which persisted to review time, in several cases one year after surgery, despite careful management of the ulnar nerve during surgery. This rate of affectation of sensitivity is comparable to that published in other series.4–13 The ulnar nerve was not transposed in any of the patients. We believe that transposing should be assessed in those situations where there is a conflict between the synthesis material and the nerve.
The standard approach for treatment of this type of fracture is posterior with olecranon osteotomy since this offers extensive exposure, although complications have been described.19 Delay in consolidation of the osteotomy and local discomfort caused by the synthesis material at said level are the most common problems with this approach. In our series there was a case of olecranon pseudoarthrosis with no clinical expression. In 12 cases we used the Newcastle approach which avoids this type of complication.
There were no cases of infection in our series.
High incidences of bone and soft tissue complications have been described after open elbow supracondylar fractures. In our series 2 grade I open fractures according to the Gustilo classification were included, with no presentation of complications.
Grant et al., reported an infection rate of 28%after immediate internal fixation in open fractures of the distal humerus although 45% of the fractures of this series were grade III open fractures.7–16
We had one case of pseudoarthrosis. Although the intraarticular region of the fracture was cured without event, a bone graft was required, in addition to osteosynthesis to obtain metaphysodiaphysary consolidation.
The limitations of our study included its retrospective nature and the relatively low number of patients. Furthermore, surgical treatment and surgical approach selected were chosen by the surgeon, and were therefore not always the same. However, our results suggest that open reduction and internal fixation of supracondylar fractures of the humerus with double plated osteosynthesis is a safe and effective technique, leading to good functional outcome and a complication rate comparable to those of studies published in the literature. A strong point to be highlighted is the long-term evaluation of quality of life (between 3 and 10 years) for a joint fracture.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments on humans or animals have been performed for this research.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Salvador J, Castillón P, Fuentes I, Bernaus M, Anglès F. Tratamiento de fracturas supracondíleas de húmero mediante osteosíntesis con doble placa. Rev Esp Cir Ortop Traumatol. 2017;61:324–330.