Management of injuries to the articular cartilage is complex and challenging. Our purpose was to assess outcomes of a cohort of patients who underwent hip arthroscopy with full-thickness chondral damage treated with microfracture and compare these outcomes with those from a similar cohort of patients who did not.
Material and methodsWe prospectively gathered the data of 31 hips treated with microfracture from January 2009 to January 2016. In the cohort of hips without chondral damage there were 49 hips. All patients were assessed pre- and postoperatively with 4 patient-reported outcome instruments.
ResultsThe mean follow-up was 36.2 months in the cohort of patients with full-thickness chondral damage, and 36.6 months in the cohort of patients without chondral damage. Both groups demonstrated significant improvement in all patient-reported outcome instruments between preoperative and final follow-up. There was no statistically significant difference between both cohorts at final follow-up.
DiscussionThis study showed that patients undergoing microfracture during hip arthroscopy had significant improvement in all patient-reported outcome instruments during follow-up. The greatest improvement was noted at 6 months postoperatively. Both groups showed no significant difference in final patient-reported outcome instruments scores.
El tratamiento de las lesiones cartilaginosas de espesor completo constituyen un reto para el cirujano ortopédico. Nuestro objetivo fue determinar los resultados clínicos de una cohorte de pacientes con lesión cartilaginosa acetabular de espesor completo tratados mediante microfracturas, y comparar los resultados con una cohorte similar sin lesión cartilaginosa acetabular.
Material y métodosEstudio prospectivo de 31 caderas con lesión cartilaginosa acetabular de espesor completo intervenidas mediante microfracturas por cirugía artroscópica entre enero de 2009 y enero de 2016. La cohorte sin lesión cartilaginosa constaba de 49 caderas. Se utilizaron 4 cuestionarios de valoración clínica.
ResultadosEl seguimiento medio fue de 36,2 meses en la cohorte de pacientes con lesión cartilaginosa de espesor completo y de 36,6 meses en la cohorte de pacientes sin lesión cartilaginosa. La puntuación media se incrementó significativamente en ambas cohortes en los cuestionarios de valoración clínica entre el valor preoperatorio y al final del seguimiento. No hubo diferencias significativas entre ambas cohortes al final del seguimiento.
DiscusiónEl estudio muestra que el tratamiento de la lesión cartilaginosa de espesor completo mediante microfracturas permite una mejoría significativa en los cuestionarios de valoración utilizados, que se mantiene durante el seguimiento del estudio. El mayor incremento de la puntuación en los cuestionarios de valoración clínica se produce en los 6 primeros meses. Al comparar los resultados con una cohorte de pacientes sin lesión cartilaginosa no hubo diferencias significativas al final del seguimiento.
In young adult hips without dysplasia, the most common mechanism leading to acetabular chondral damage is femoroacetabular impingement (FAI). Direct contact during flexion of the hip, of an aspherical femoral head in the head-neck transition (cam type FAI) against a normal acetabulum, or the normal femoral neck on a retroverted or profound acetabulum (pincer type FAI), leads to injury of the acetabular labrum and subsequently of the acetabular cartilage.1,2
Chondral damage affects the joint's functional result due to the limited curative capacity, regardless of whether damage is acute or chronic. As there are no nociceptive receptors, isolated chondral damage does not produce painful symptoms. On occasion, at diagnosis, chondral damage is already at full thickness.3,4
Arthroscopic hip surgery (AHS) has led to early diagnosis of acetabular chondral damage, either through its indication in patients due to inexplicable inguinal pain and with normal diagnostic tests, or in the context of intraarticular disease through loose bodies, labrum damage or FAI.5,6 A high percentage of patients who undergo FAI by AHS present with associated joint chondral damage, although no degenerative signs appear in the preoperative radiologic study.7
Outcomes with treatment for full thickness chondral damage using microfractures at knee level8,9 have extended their usage to the hip with favourable short term outcomes.10–15
The aim of our study was to determine the clinical outcome of a cohort of patients with FAI diagnosis and treatment of full thickness acetabular chondral damage using arthroscopic microfracture hip surgery. For greater awareness of the influence of acetabular chondral damage on functional outcome, the results were compared with a cohort of patients with a diagnosis of FAI with no acetabular chondral damage. Our working hypothesis was that the clinical outcome between both groups would be similar on termination of follow-up.
Material and methodPatient selectionDuring the period between January 2009 and January 2016 a cohort of patients were selected from our data base of prospective patients who had undergone AHS, all of whom met with the following criteria: aged under 50, diagnosed with FAI, Tönnis 0-1 status, articular height over 2mm, acetabular full-thickness chondral damage acetabular treated with microfractures, and a minimum follow-up of one year. Patients with hip dysplasia which was determined by a central-rim angle under 25° were excluded, as were those with Legg-Calve-Perthes disease, previous hip surgery, avascular necrosis and those under 18.
For comparative effects, a cohort of patients who met with the same inclusion and exclusion criteria but who did not present with any acetabular chondral damage were chosen.
All the patients gave their informed consent for the inclusion in the study and this was approved by the Ethics Committee of the Clinical Research of our institution.
Clinical assessmentClinical assessment was made using 4 questionnaires: the modified Harris scale (mHHS)16; hip assessment questionnaires with sections on daily life activities (HOS-AVD) and the practice of sports (HOS-SSS),17 translated into Spanish and validated18 and the iHOT-1219 questionnaire. The patient was asked how they thought the affected hip worked compared with the healthy one, with 4 possible responses: normal, almost normal, abnormal and severely abnormal. If both hips of the patient were affected, or the contralateral hip had been operated on previously, they were asked to consider how the affected hip functioned compared with the previous situation, when there were no limits to daily activities and/or sports activities. Clinical assessments were made preoperatively, after 6 months, after one year and subsequently on an annual basis.
Preoperative physical activity was recorded according to the Tegner scale.20
Imaging studiesAnteroposterior radiologic studies of the pelvis were requested of all patients in standing position and Dunn axial projection. The presence of a cam and/or pincer type lesion was determined,2 together with the height of the joint space in the load region,21 alpha angle,2 acetabular angle,2 Tönnis angle2 and degree of articular degeneration according to the Tönnis scale.22
The imaging study was completed with a conventional NMR in a Tesla 3 device, to rule out the presence of avascular necrosis, tendinopathies or intra-articular damage.
Surgical proceduresSurgery was performed with spinal anaesthesia, in accordance with the previously described surgical technique.23 The procedure commenced with examination of the central compartment. The acetabular overcoverage or “pincer” type lesion was determined by the presence of diffuse equimosis of the labrum, labral ossification, intralabral cystic degeneration and/or the extension of the acetabular bone ridge beyond the chondro-labral union.24 If a pincer type lesion presented, the acetabular overcoverage anomalies were corrected by direct examination and radioscopic control. Labral lesions were repaired with suturing whenever possible and particularly if they affected the chondro-labral union. If not, debridement was performed whilst maintaining the largest amount of chondro-labrum possible.25 The presence of tendon disease of the psoas with a base of inflammation or rupture of the labrum at psoas location level in the acetabular rim was determined, and tenotomy of the psoas in the central compartment was performed when necessary.26
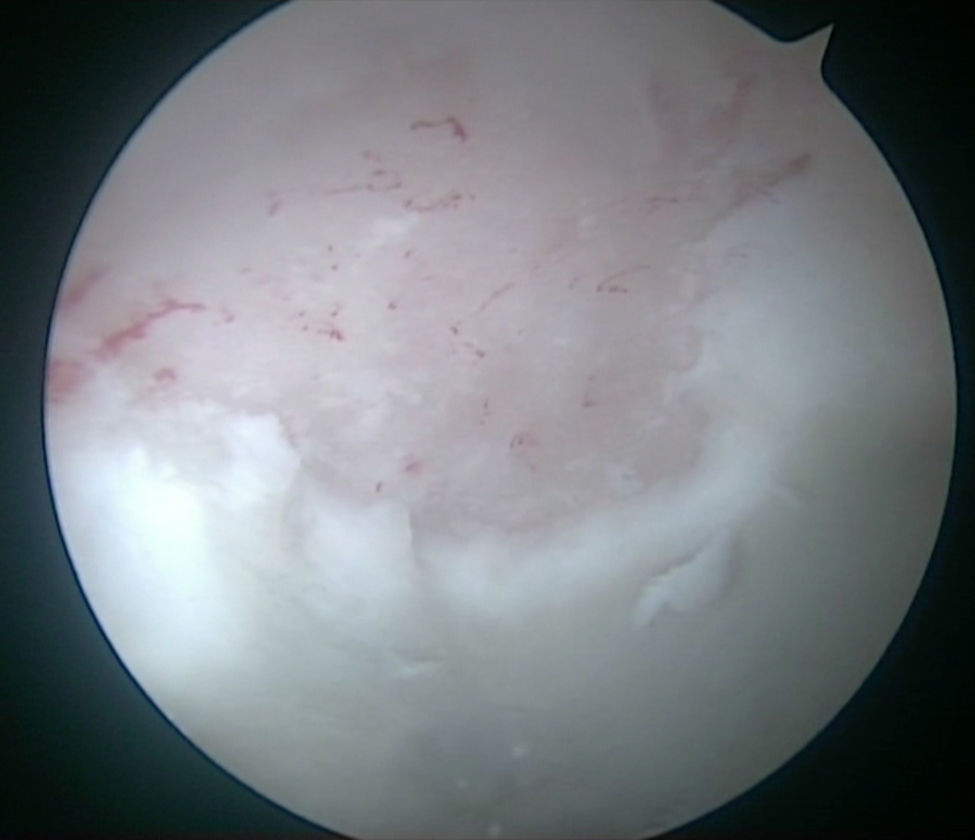
Chondral damage of the acetabular rim was classified according to the recommendations of the Multicenter Arthroscopic Hip Outcome Research Network.27
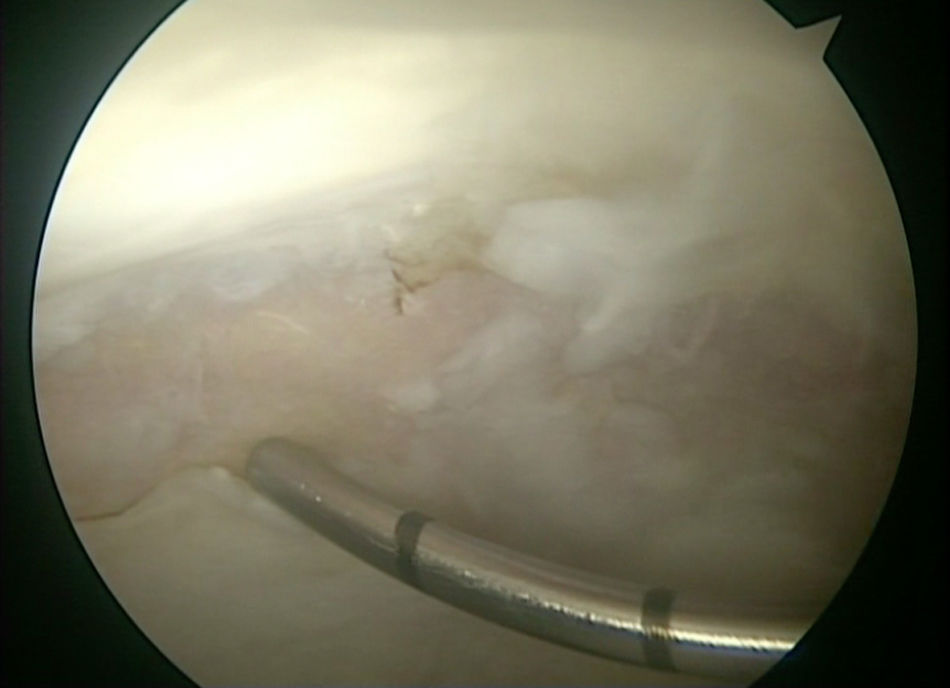
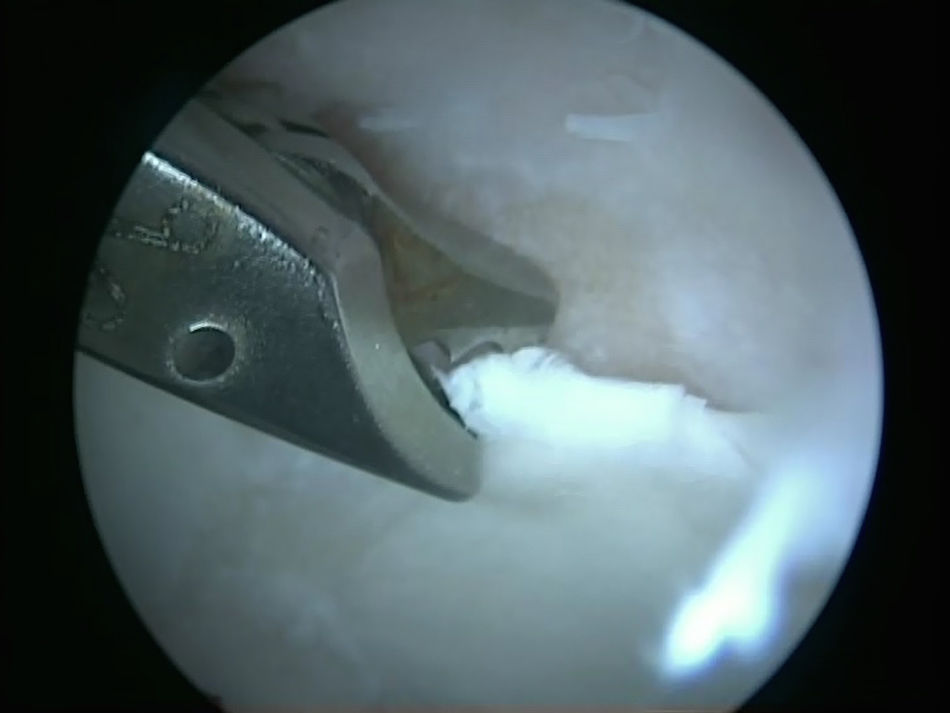
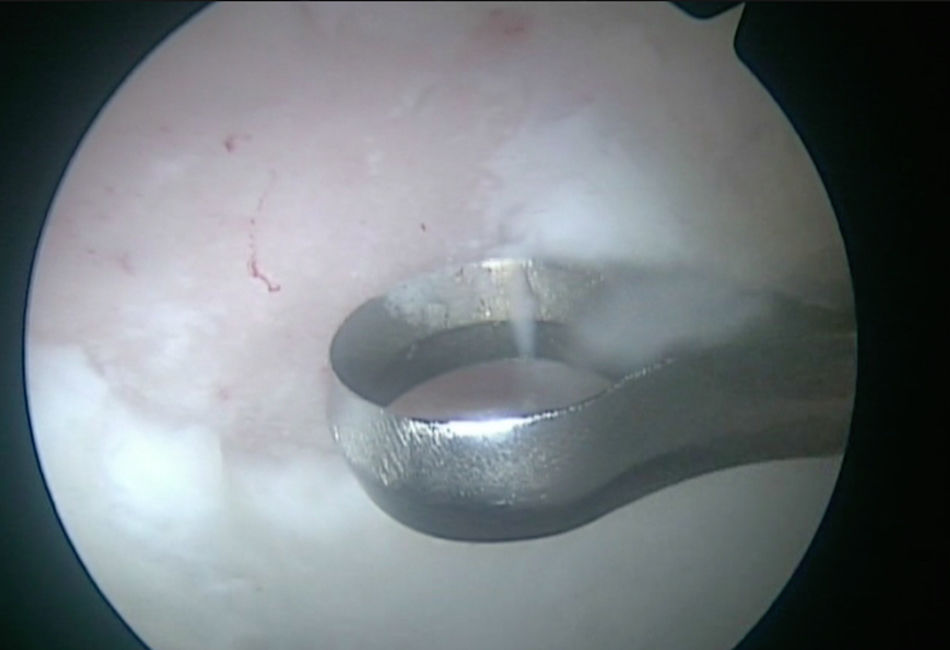
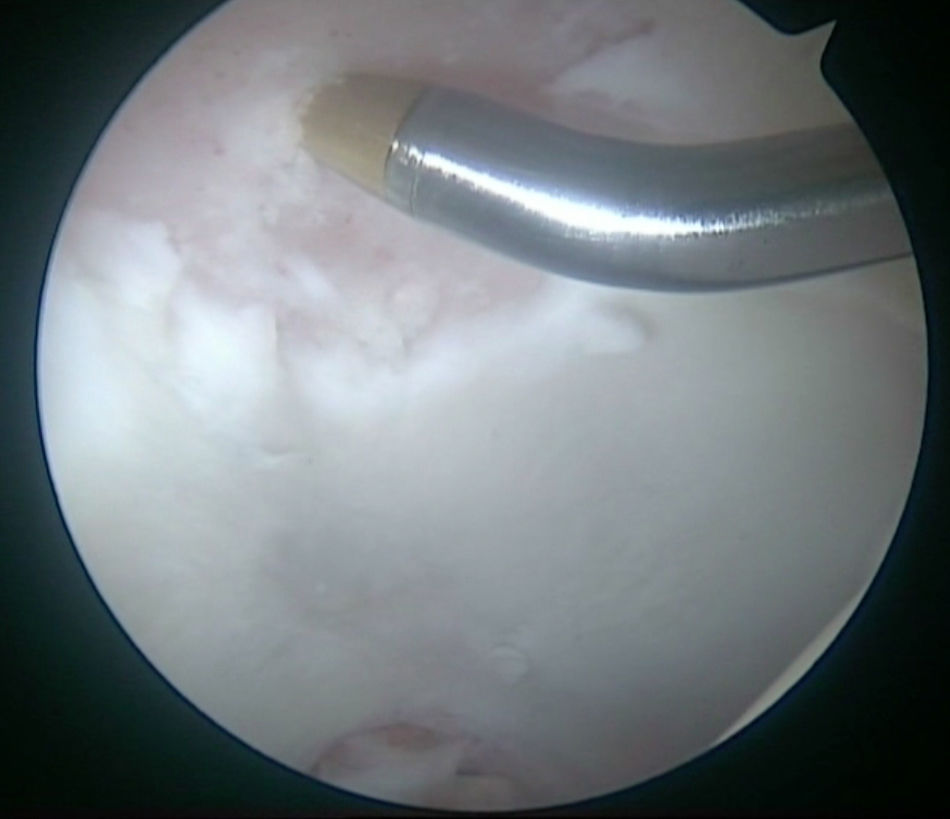
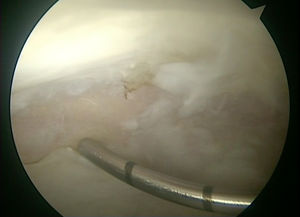
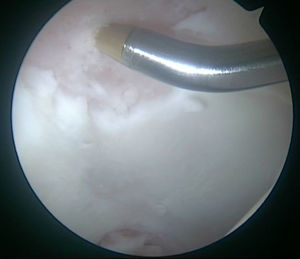
When full thickness chondral damage was detected, its location was determined according to the geographic zone method described by Ilizaliturri et al.,28 and its size, with the use of a measurement probe (Fig. 1). For microfracture surgery, the anterolateral portal vein was used as the viewing portal and the medioanterior portal as the working portal for insertion of material. The microfracture technique was performed in accordance with the procedure described by Crawford et al.29 The first step of the process consisted in ensuring there was a stable chondral rim. For this, the loose delaminated cartilage was cleaned with pincers (Fig. 2) and swing motor (Fig. 3). The acetabular labrum was accurately repaired to ensure that we finally had a full thickness chondral damage which was well defined geographically and able to contain the coagulation of pluripotent cells from the deep spongy bone which was reached with the microfractures. The calcified tissue layer was resected with a curette (Fig. 4), avoiding destructuring of the subchondral bone. Once the stable chondral rim was ensured, we proceeded to manually perforate with a 30 or 45° spike, always perpendicular to the subchondral bone, from the periphery of the lesion. The perforations were separated from one another by 3–4mm and had a depth of 3–4mm (Fig. 5). Finally the intraarticular fluid flow was cut off to determine issue of blood or fat through the holes made (Fig. 6).
Following this, the peripheral compartment was examined. If full thickness chondral damage was detected at femoral head level, microfractures were performed using the same technique as at acetabular level. The cam type lesion was treated with direct low vision osteoplasty and fluoroscopy. The joint capsule was systematically repaired with simple sutures.
Postoperative managementThe patients were discharged after 24h. Passive mobility was initiated on discharge, with restrictions of hip rotations for 4 weeks. The specific rehabilitationist protocol was identical in both cohorts. No restrictive mobility orthetics were used.
In all cases partial assisted weight bearing with 2 crutches was allowed, in the microfractures cohort, for 8 weeks, and in the patients without chondral damage, for 4 weeks.
Statistical analysisStatistical analysis was performed with the SPSS programme, version 18.0 (SPSS Inc., Chicago, U.S.A.). P values equal to or lower than .05 were considered significant. To determine normal distribution the Kolmogorov–Smirnov test was used. To compare continuous variables the Student's t-test and the Mann–Whitney U test were used, and for categorical variables, the chi-square test was used in those with normal distribution or the Mantel-Haenszel for non-parametric data.
ResultsThe cohort of patients with full thickness chondral damage comprised 31 hips. Mean age was 39 years (SD 7.2; range 21–50). Bilaterality was present in 12 patients. By gender, 16 were male and 3, female. In the cohort of 49 patients without chondral damage mean age was 38.4 (SD 7.7; range 18–50). Bilaterality was present in 12 patients. By gender, 25 were male and 12 female.
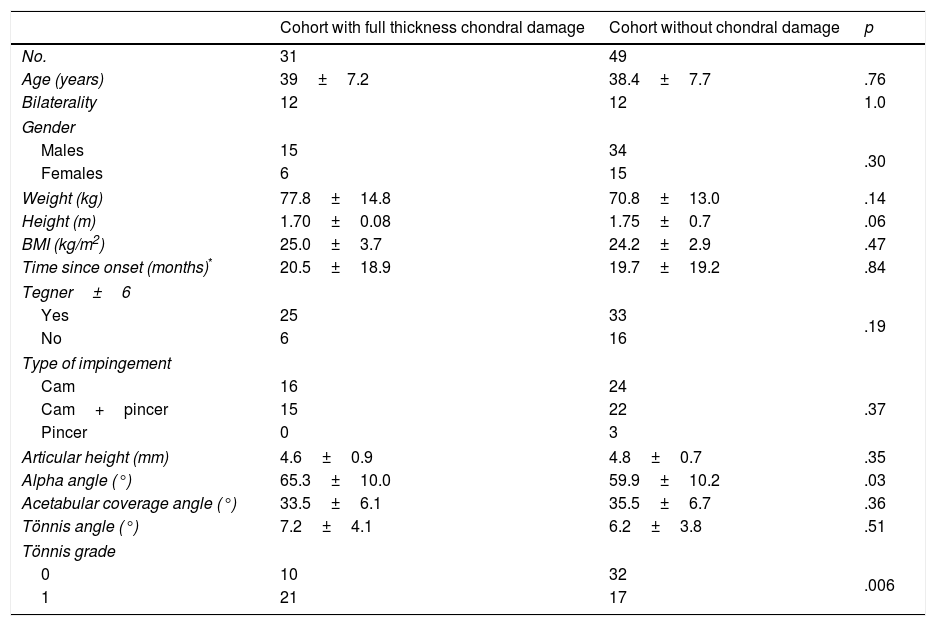
There were no significant differences between both cohorts with regard to age, bilaterality, gender, side, weight, height, body mass index, symptom onset time, level of physical activity and type of FAI. Radiologic variables were similar with regard to articular height, acetabular coverage angle and Tönnis angle. However, the mean value of the alpha angle and the percentage of patients with Tönnis 1 grade articular degeneration were higher in the cohort of patients with full thickness chondral damage with both differences being significant (Table 1).
General data of the series.
| Cohort with full thickness chondral damage | Cohort without chondral damage | p | |
|---|---|---|---|
| No. | 31 | 49 | |
| Age (years) | 39±7.2 | 38.4±7.7 | .76 |
| Bilaterality | 12 | 12 | 1.0 |
| Gender | |||
| Males | 15 | 34 | .30 |
| Females | 6 | 15 | |
| Weight (kg) | 77.8±14.8 | 70.8±13.0 | .14 |
| Height (m) | 1.70±0.08 | 1.75±0.7 | .06 |
| BMI (kg/m2) | 25.0±3.7 | 24.2±2.9 | .47 |
| Time since onset (months)* | 20.5±18.9 | 19.7±19.2 | .84 |
| Tegner±6 | |||
| Yes | 25 | 33 | .19 |
| No | 6 | 16 | |
| Type of impingement | |||
| Cam | 16 | 24 | .37 |
| Cam+pincer | 15 | 22 | |
| Pincer | 0 | 3 | |
| Articular height (mm) | 4.6±0.9 | 4.8±0.7 | .35 |
| Alpha angle (°) | 65.3±10.0 | 59.9±10.2 | .03 |
| Acetabular coverage angle (°) | 33.5±6.1 | 35.5±6.7 | .36 |
| Tönnis angle (°) | 7.2±4.1 | 6.2±3.8 | .51 |
| Tönnis grade | |||
| 0 | 10 | 32 | .006 |
| 1 | 21 | 17 | |
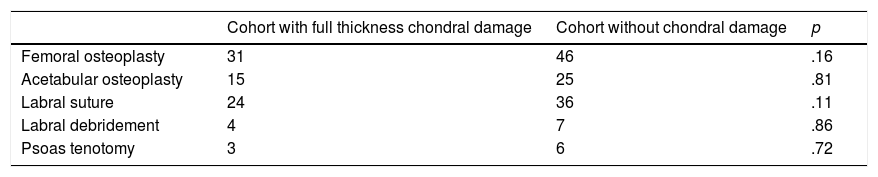
During AHS, in the cohort with full thickness chondral damage a cam type lesion was detected in all hips (100%), a pincer type lesion in 15 hips (48.3%), labral rupture in 24 hips (77.4%), labral degeneration in 4 hips (12.9%) and tendon disorder of the psoas in 3 hips (9.6%). In the cohort without chondral damage, cam type lesion presented in 46 hips (93.8%), pincer type lesion in 25 hips (51.0%), labral rupture in 36 hips (73.4%), labral degeneration in 7 hips (14.2%) and tendon disorder of the psoas in 6 hips (12.2%). Associated surgical procedures during AHS are described in Table 2.
The mean size of the full thickness chondral damage was 19.4mm in length (SD 9; range 11–30mm) and 12.2mm width (SD 7; range 10–30mm). Their location in 19 hips (61.3%) was in region 2 and 3, in 8 hips (25.8%) in region 2, in 3 hips (9.7%) in region 3 and one hip (3.2%) in region 1. All lesions were located at chondrolabral union level. The mean region of full thickness chondral damage was 222mm2 (SD 75; range 75–450mm2). In 9 hips (29%) the region was greater than 400mm2. Only one patient presented with femoral head level chondral damage, which was 5mm wide by 10mm long.
Mean follow-up was 36.2 months (SD 21.3; range 12–84 months) in the cohort of patients with full thickness chondral damage and 36.6 months (SD 24.5; range 12–84 months) in the cohort of patients without chondral damage, differences which were not statistically significant (p=.90).
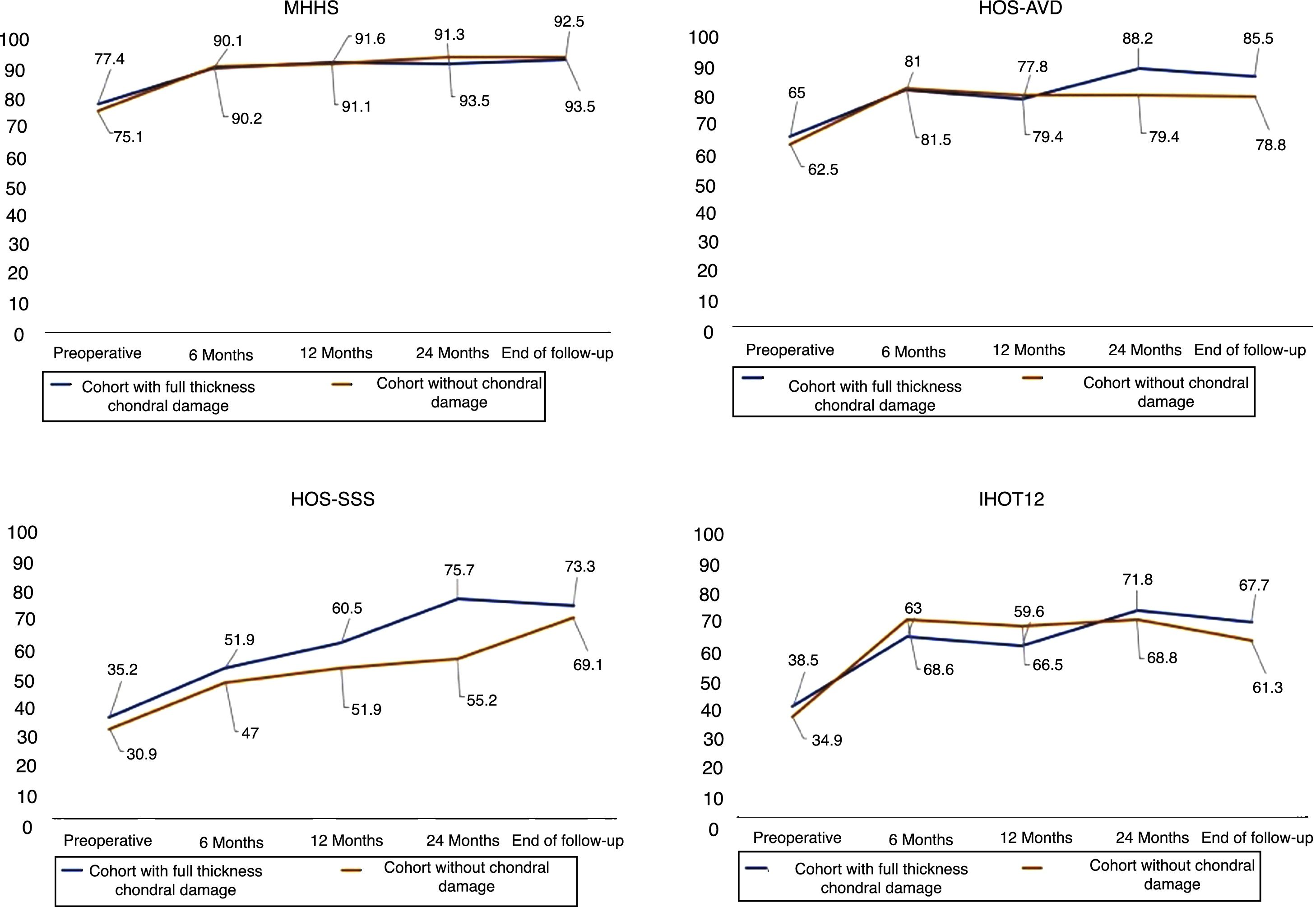
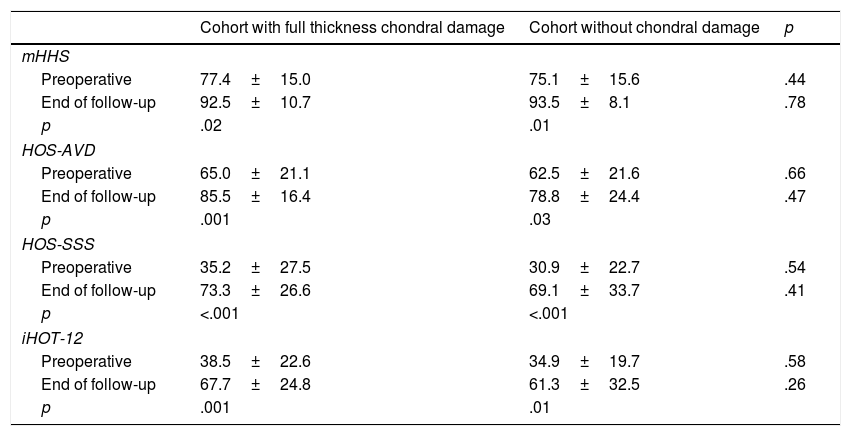
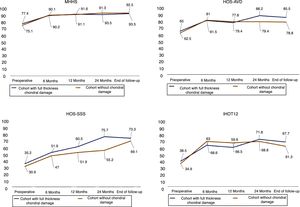
The mean score increased significantly in both cohorts in the clinical assessment questionnaires between preoperative and follow-up termination values. When analysing these values in both cohorts, the differences were not significant (Table 3). There was no significant relationship between the area of the chondral damage and the preoperative clinical assessment questionnaires nor those at the end of follow-up (p>.05). Fig. 7 shows the evolution of mean scores in the clinical assessment questionnaires during follow-up.
Functional results of both cohorts in the different questionnaires of clinical assessment.
| Cohort with full thickness chondral damage | Cohort without chondral damage | p | |
|---|---|---|---|
| mHHS | |||
| Preoperative | 77.4±15.0 | 75.1±15.6 | .44 |
| End of follow-up | 92.5±10.7 | 93.5±8.1 | .78 |
| p | .02 | .01 | |
| HOS-AVD | |||
| Preoperative | 65.0±21.1 | 62.5±21.6 | .66 |
| End of follow-up | 85.5±16.4 | 78.8±24.4 | .47 |
| p | .001 | .03 | |
| HOS-SSS | |||
| Preoperative | 35.2±27.5 | 30.9±22.7 | .54 |
| End of follow-up | 73.3±26.6 | 69.1±33.7 | .41 |
| p | <.001 | <.001 | |
| iHOT-12 | |||
| Preoperative | 38.5±22.6 | 34.9±19.7 | .58 |
| End of follow-up | 67.7±24.8 | 61.3±32.5 | .26 |
| p | .001 | .01 | |
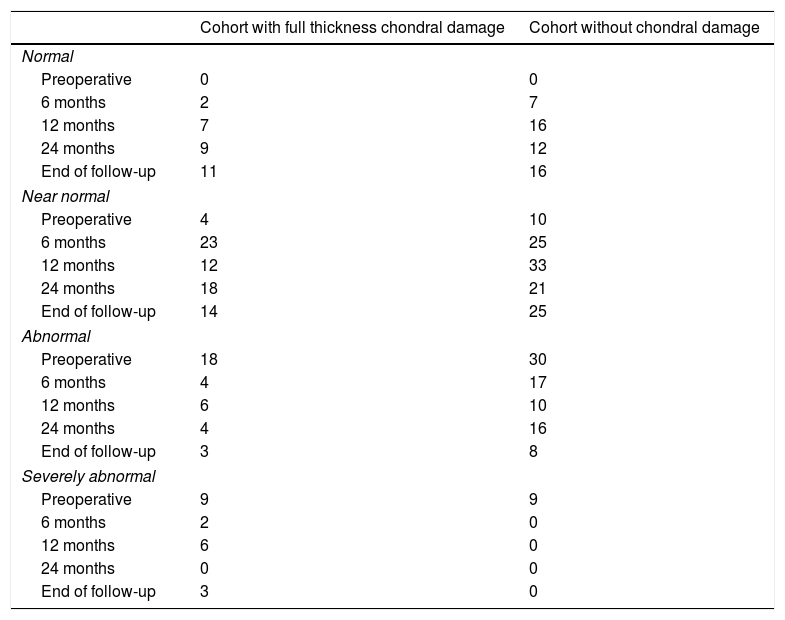
The function of the affected hip perceived by the patient in both cohorts is reflected in Table 4. Preoperatively, the function of the hip was abnormal or severely abnormal in 27 hips (87.0%) in the cohort of patients with full thickness chondral damage, compared to 39 hips (79.5%) in the cohort of patients without chondral damage. At the end of follow-up, the number of hips dropped to 5 (16.1%) in the cohort of patients with full thickness chondral damage, and 8 (16.3%) in the cohort of patients without chondral damage. The differences in both cohorts between the function of the preoperative hip and the end of follow-up were statistically significant (p<.001). The region of chondral damage was not significantly related to the function of the affected hip perceived by the patient preoperatively or at the end of follow-up (p>.05).
Function of the affected hip according to the subjective assessment of the patient in both cohorts.
| Cohort with full thickness chondral damage | Cohort without chondral damage | |
|---|---|---|
| Normal | ||
| Preoperative | 0 | 0 |
| 6 months | 2 | 7 |
| 12 months | 7 | 16 |
| 24 months | 9 | 12 |
| End of follow-up | 11 | 16 |
| Near normal | ||
| Preoperative | 4 | 10 |
| 6 months | 23 | 25 |
| 12 months | 12 | 33 |
| 24 months | 18 | 21 |
| End of follow-up | 14 | 25 |
| Abnormal | ||
| Preoperative | 18 | 30 |
| 6 months | 4 | 17 |
| 12 months | 6 | 10 |
| 24 months | 4 | 16 |
| End of follow-up | 3 | 8 |
| Severely abnormal | ||
| Preoperative | 9 | 9 |
| 6 months | 2 | 0 |
| 12 months | 6 | 0 |
| 24 months | 0 | 0 |
| End of follow-up | 3 | 0 |
No complications were recorded relating to the microfracture technique. In the cohort with full thickness chondral damage, one patient required surgical reinvention 19 months after AHS with the implantation of a total hip replacement. This was a 45-year-old male with full thickness chondral damage 12mm wide by 40mm long (region 480mm2), and full thickness chondral damage in the femoral head 5mm wide by 10mm long.
DiscussionThe most significant findings of our study were: (1) full thickness chondral damage treatment with microfracture which led to significant improvement according to the assessment questionnaires used, and this was maintained throughout study follow-up; (2) no significant differences with a cohort of patients without chondral damage; (3) the highest score increase in the assessment questionnaire occurred during the first 6 months.
Recommendation for microfractures referred to in the literature comprises focal and contained full thickness chondral damage, at least 400mm2,11,13,15 in size. In the FAI context, acetabular chondral damage starts at chondolabral level, and prior repair of the labrum is therefore recommended as a contention method for coagulation which forms after performing microfractures.13 Different publications report favourable outcomes from microfracture treatment in full thickness chondral damage with short term follow-up. Byrd and Jones report an increase of 20 points in the mHHS (from 65 to 85) in their series of 58 patients, with a mean follow-up of 16 months (range 12–24 months).30 Domb et al. indicate a significant improvement in assessment questionnaires used (mHHS, NAHS, HOS-ADL) in 30 patients with mean follow-up of 35 months (range 20–50 months).31 Later, Domb et al. compared the clinical outcomes of 79 patients with full thickness chondral damage treated with microfractures with 158 patients without chondral damage with a minimum follow-up of 2 years, and no significant differences are found between the two groups.10 Lodhia et al.12 found no significant differences either between 35 patients with full thickness chondral damage treated with microfractures with 70 patients without chondral damage, with a mean follow-up of 36 months (range 24–55 months). MacDonald et al.15 and Marquez-Lara et al.11 published systematic reviews of the outcome of microfractures in patients with full thickness chondral damage in the FAI. 12 studies were selected which included 267 patients, and in 11 of the 12 studies referred to satisfactory results with a mean follow-up of 29.5 months (range 4–60 months). Fontana and de Girolamo32 compared the results of 42 patients treated with microfractures with 55 patients treated with the autologous matrix-induced chondrogenesis technique, with a 5-year follow-up. Both groups significantly improved in the mHHS at 6 and 12 months, but they refer to posterior worsening in patients treated with microfractures, especially in lesions over 400mm.2 In our series of comparative cohorts we have found significant differences in the clinical assessment questionnaires used, with a mean follow-up of 36 months (range 12–84 months).
Bleeding after microfractures enables pluripotent cells to be selected from deep spongy bone with the ability to differentiate into chondrocytes and regenerate chondral tissue, repairing the articular defect. Karthikeyan et al.33 performed a review AHS in 20 patients after a mean of 17 months after microfracture, with a mean repair of the lesion of 93%, and defining the cartilage as microscopically stable. In 2 patients repair tissue biopsies were taken which reported on fibrocartilage with collagen fibres distributed in an extracellular matrix. Philippon et al.34 indicate similar results of repair in 8 patients with a damage coverage of between 95% and 100% after a mean 20-month follow up.
The majority of studies recommend partial weight bearing with crutches after performance of microfractures. The period of partial weight bearing was established between 4 and 16 weeks. The protocols of rehabilitation are varied, without determining which is the ideal for this group of patients.11,15
Microfracture technique is a safe procedure. MacDonald et al.15 refer in a systematic review to a .7% of complications in 297 patients. In our series we did not record any complication associated with the procedure.
The need for surgical reintervention after microfractures is 1.1% with a mean follow-up of 29 months in 267 patients, according to the systematic review of MacDonald et al.15 However, Domb31 published a 6.6% conversion to total hip arthroplasty (THA) and a 6.6% of revision THA, in 30 patients with a mean follow-up of 35 months. Lodhia et al.12 refer to 8.6% conversion to THA and 20% revision THA, in 35 patients with a mean follow-up of 36 months. Domb et al.10 indicate a 12.6% conversion to THA in 79 patients with a mean follow-up of 24 months. Fontana and de Girolamo,32 a 7.8% conversion to THA in 77 patients with a minimum follow-up of 36 months. The risk factors relating to THA conversion described by Fontana and de Girolamo are the presence of cam type lesion, the chondral defect larger than 400mm2, the association with chondral damage of the femoral head and a preoperative value in the mHHS under 50 points.32 In our series there was a 3.2% conversion to THA with a mean follow-up of 36 months.
Our study has several imitations. Given that the patients with microfractures had also undergone other surgical procedures, it is practically impossible to know the effect of the microfractures in the final clinical outcome. The series is short in the number of cases and follow-up is short term. The cohorts were not comparable with regard to the degree of articular degeneration according to the Tönnis scale, and in the cohort of patients with full thickness chondral damage there were 70% of Tönnis 1 patients, compared with 34.6% in the cohort of patients without chondral damage.
A strength to highlight is that this is a prospective cohort study in which 4 clinical assessment questionnaires were used, aimed at increasing the scientific evidence in the final result of this patient group.35
ConclusionClinical results of a cohort of patients with full thickness chondral damage in the FAI treated with microfractures are similar to a cohort of patients without chondral damage after 36 months of mean follow up. Greater follow-up of the cohort was needed to determine stability of clinical outcome obtained.
Level of evidenceLevel of evidence III.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments have been conducted on humans or animals for this research study.
Confidentiality of dataThe authors declare that they have adhered to the protocols of their place or work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflict of interests to declare
Please cite this article as: Más Martínez J, Sanz-Reig J, Verdú Román CM, Bustamante Suárez de Puga D, Morales Santías M, Martínez Giménez E. Tratamiento artroscópico mediante microfracturas de la lesión cartilaginosa acetabular de espesor completo. Estudio de cohortes con seguimiento medio a 3 años. Rev Esp Cir Ortop Traumatol. 2018;62:248–256.