and objective The aim of this work was to evaluate clinical outcomes of patients with biceps brachii tendon rupture who underwent a surgical tendon reconstruction using our own modified double approach technique.
PatientsThe study was performed in 20 patients (21 cases) with biceps brachii tendon rupture. Patients were treated with our own double-approach surgical technique consisting of 2 minimum incisions. After one year follow-up, functional evaluation was assessed using the mayo Elbow Performance Score, muscle strength was estimated with the Medical Research Council questionnaire and pain was evaluated with the Visual Analogic Scale. Range of motion was determined by measuring extension and flexion.
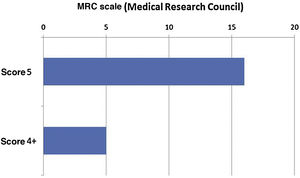
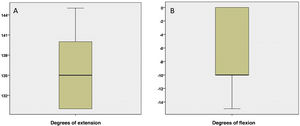
ResultsOne year after surgery all patients had returned to sports at the same level they had previously. Visual Analogic Scale was 1.90±0.89 (mean±standard deviation) and median Mayo Elbow Performance Score was 90 (minimum–maximum: 80–100). Of them, 16 patients (76.2%) showed the highest Medical Research Council score, score 5, while 6 cases (26.1%) still scored 4+. Patients had a mean of 136.67° flexion (95% CI: 134.14°–139.19°) and −7.38° extension (95% CI: −10.04° to −4.72°).
ConclusionsDouble-incision surgical approach for distal biceps brachial tendon rupture anatomical repair is a safe technique, providing results that allow patients muscle recovery and return to sports.
En este trabajo se estudió la evolución clínica de pacientes con rotura de tendón del bíceps braquial tratados mediante reconstrucción quirúrgica según nuestra propia técnica de doble incisión.
PacientesSe incluyó a 20 pacientes (21 casos) de rotura de tendón del bíceps braquial tratados mediante nuestra propia técnica quirúrgica de doble abordaje modificada, consistente en 2incisiones mínimas. La evaluación funcional se determinó mediante la escala Mayo Elbow Performance Score, la fuerza muscular se determinó con el cuestionario Medical Research Council y el dolor mediante la Escala Analógica Visual a los 12 meses de seguimiento. Se determinó el rango de movilidad midiendo los grados de flexión y extensión.
ResultadosUn año después de la cirugía todos los pacientes habían vuelto al deporte al mismo nivel que tenían previamente. La puntuación de Escala Analógica Visual fue de 1,90±0,89 (media±desviación estándar) y la mediana de la escala Mayo Elbow Performance Score de 90 (mínimo-máximo: 80-100). Del total, 16 (76,2%) presentaron la máxima puntuación en la escala Medical Research Council (puntuación 5), mientras que 5casos (23,81%) tuvieron una puntación de 4+. La media de extensión fue de 136,67° (IC 95%: 134,14°-139,19°) y −7,38° de flexión (IC 95%: [−10,04°]-[−4,72°]).
ConclusionesEl abordaje quirúrgico de la doble incisión para la reparación anatómica de las roturas de tendón distal del bíceps braquial es seguro y proporciona resultados que permiten la recuperación muscular y la vuelta al deporte de los pacientes.
Biceps brachii tendon rupture is a rare injury that accounts for about 3% of all biceps tears.1,2 It mainly occurs in middle-aged men (40–50 years), with pre-existing degenerative changes that predispose to this injury,3–7 predominating in the dominant arm.3
Previous studies suggest that the mechanism of injury may be excessive concentric contraction in arm flexion and supination.8 Sudden pain followed by functional impotence is a constant in these injuries and is occasionally accompanied by bruising or ecchymosis on the anteromedial facet of the arm. Due to proximal retraction of the muscle, an aesthetic deformity often appears, which may go unnoticed in patients with little muscle or a degree of obesity. O’Driscoll et al.9 described the hook test, which shows high sensitivity and specificity, as well as the squeeze test, for the diagnosis of complete distal biceps brachii rupture.10
Chronic injuries lead to loss of arm strength in flexion and supination, combined with asymmetry with respect to the contralateral arm. Irritation of the lateral cutaneous nerve may cause pain: surgical reconstruction is advisable in these patients.3,11 Boyd and Anderson12 first described the two-incision approach to avoid the risk of posterior interosseous nerve injury. Morrey et al.2 published a modification of this double approach technique with the aim of reducing any potential heterotopic calcification after incising the musculature of the external aspect of the olecranon.
In this paper we assess the return to sports and clinical outcome of patients with biceps brachii tendon rupture who underwent surgical reconstruction of the tendon using our own modified double-approach technique.
Materials and methodsPatientsThis is a retrospective study conducted in 20 patients, with 21 cases of biceps brachii tendon rupture (one patient had rupture in both arms), treated in our unit from 2008 to 2017. The study was conducted in accordance with the ethical principles approved in the 1964 Declaration of Helsinki, revised in 2013. The study was approved by the institution's ethics committee and patients signed their informed consent to participate. At the time of injury, the patients had a mean age of 44.7±6.6 years (mean±SD). The injury was in the right arm in 14 cases (66.7%) and the in the left in the other 7 (33.3%). All the patients practised sports and the injury occurred during sports.
Surgical procedureThe surgical technique consisted of a series of modifications to existing surgical procedures. Locoregional anaesthesia of the limb is used with the patient in the supine position and with the aid of a hand table. A tourniquet is used on the arm and the surgical field is prepared.
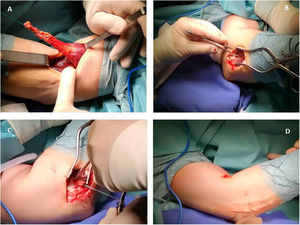
A limited transverse incision of 2–3cm is made just above the ulnar crease; the avulsed tendon is sought and located with blunt dissection; we carry out a thorough inspection of the avulsed tendon and the last 5–6mm of the degenerated tendon is resected. We then place 2 two non-absorbable number 5 Ethibond Bunnell sutures in the avulsed tendon. This suture allows us to traction the tendon in its entirety up to its bony insertion (Fig. 1A).
We then palpate the radial tuberosity and make a second incision in the radial tuberosity, transmuscularly, separating the common and supinator extensor muscle, with the forearm in maximum pronation. We never expose the ulna. We prepare the bed of the radial tuberosity with high-speed burs in a trench 1cm wide and several millimetres deep and leave a bone anchor with the threads, which will be used to anchor the tendon (Fig. 1B).
We pass a curved, blunt haemostasis forceps from the forearm towards the arm, sliding it under the radial tuberosity and advancing proximally, between the radius and ulna, using flexion-extension manoeuvres until we reach the arm: the blunt tip of the forceps emerges from the transverse incision.
We insert the Ethibond threads into the tip of the forceps and pull it distally until the threads pass into the forearm. Once the threads have been passed, we pull on them using flexion-extension manoeuvres until the avulsed tendon is completely extracted through the distal incision of the forearm; we remove the Ethibond suture and re-suture the tendon with Bunnell type stitches with the threads belonging to the transosseous anchor that has been previously placed in the radial tuberosity, knot and tightly tension the suture until the avulsed tendon is completely attached to the radial tuberosity with the arm in a neutral position.
We then check for full elbow motion, in supination-pronation, flexion and full extension, free and without anomalies throughout the range of motion.
We close in layers, release the tourniquet for adequate haemostasis, leave no drain and place a splint with a compressive bandage in 90° elbow flexion with the forearm in a neutral position.
To minimise any ectopic calcifications, we avoid passing the dissecting forceps between the ulna and the anconeus or between the anconeus and the ECU (Kocher's interval). As a fixation system we used a transosseous suture using a non-absorbable, 5.5mm Healix anchor (DePuy Synthes, Madrid, Spain) (Fig. 1C). After suturing (Fig. 1D), patients are immobilised for 4 weeks in a splint and sling and then follow a 6-week rehabilitation programme.
Evaluation of clinical progressOne year after surgery, the functional progression of the injured arm was assessed using the Mayo Elbow Performance Score (MEPS).13 Muscle strength was assessed using the Medical Research Council (MRC) questionnaire.14 Pain was assessed using the Visual Analogue Scale (VAS). Range of motion (ROM) was determined by measuring degrees of extension and flexion.
Statistical analysisThe data were analysed using IBM® SPSS® Statistics, version 22 (New York, USA). Qualitative variables were expressed in counts or percentages. Relationships between these variables were studied using contingency tables and analysed using Pearson's χ2 test. Quantitative variables were expressed with the mean or median as a measure of central tendency and the standard deviation or minimum and maximum values as a measure of dispersion. The mean and the 95% confidence interval (95% CI) of the mean were estimated for ROM. Normality was analysed with the Kolmogorov–Smirnov test. The distribution of quantitative variables within the different categories of qualitative variables was tested using the non-parametric Mann–Whitney U (2 categories) or Kruskal–Wallis (more than 2 categories) test. Spearman's correlation coefficient was used to identify possible relationships between variables. All statistical comparisons were bilateral, with a significance level of 5%.
ResultsThe median time until the patients underwent biceps brachii tendon reattachment was 7 days (minimum: 1 day; maximum: 30 days). After surgery, one patient developed neuroapraxia, which resolved spontaneously. After surgery, the mean recovery time (time between surgery and discharge) was 4.43±1.21 months. All patients returned to their previous level of sporting activity.
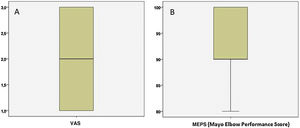
One year after surgery, the patient's clinical and functional progression was assessed. The median pain measured using the VAS scale was 1.90±.89 (Fig. 2A) and the median MEPS scale was 90 (80–100) (Fig. 2B). Muscle power evaluated using the MRC scale is shown in Fig. 3. The results of the MRC scale assessment showed the maximum score (score 5) in 16 cases (76.2%) while in the remaining 5 cases (23.8%) the score was 4+. Regarding assessment of ROM one year after surgery, patients had 136.67° mean extension (mean 95% CI 134.14–139.19) and −7.38° mean flexion (mean 95% CI: −10.04 to −4.72) (Fig. 4). As expected, flexion and extension degrees were highly correlated (ϱ=−.726; p<.001). Likewise, a statistically significant correlation was found between degrees of flexion and the MEPS scale (ϱ=.470; p=.032) and the MRC score (ϱ=.581; p=.006).
Table 1 shows the epidemiological factors that could influence the clinical outcomes of surgical treatment. Eight patients had a medical history of interest, including severe allergies, asthma, hepatitis C virus infection, hypertension, thalassaemia minor, dyslipidaemia, or psoriasis. Of these, 6 patients with a medical history were under pharmacological treatment; 4 patients had undergone surgery for trauma, such as anterior cruciate ligament reconstruction, disc herniation, knee prosthesis or frontal bone reconstruction (Table 1). A statistically significant relationship was only found between the MEPS scale and pharmacological treatment in those with a medical history of interest. Thus, the median MEPS in the patients without treatment was 100 (80–100), significantly higher than in the patients with treatment, whose median MEPS was 90 (80–90) (p=.010).
DiscussionThe present study evaluated the benefits of an anatomical repair technique for distal biceps brachial tendon rupture using a double-incision surgical approach. The results were evaluated in terms of clinical outcome and the patients’ return to their previous level of physical activity. Distal biceps brachial tendon rupture is a relatively rare injury affecting 1.2 per 100,000 patients,4 primarily middle-aged men aged 40–50 years. Our results are in line with the literature.4,15 Thus, the patients included in the present study were all men with a mean age of 44.5 years and practised high-intensity sport. We found one bilateral case in a patient who trained with weights and simultaneously ruptured both distal biceps brachii tendons. In this regard, there are publications that indicate that the risk of rupture of the biceps brachii tendon in the contralateral arm may be increased by 8%.16 The injury was in the dominant arm in the other patients and occurred while practising a medium- or high-intensity sporting activity, in competition or training.
There was only one complication in our series of patients, a neuroapraxia probably caused by the placement of intraoperative spacers and which resolved spontaneously. According to our results, there are clear advantages in terms of few postoperative complications and the athlete's full recovery. They were able to return to physical activity at the same level as before the injury. In this regard, Lang et al.17 conclude, in a retrospective study of 47 patients, that a double incision approach in the hands of an experienced surgeon is a simple and inexpensive method with satisfactory clinical results.
In our technique, we used a 5.5mm “Healix” anchor, and found no cases of radioulnar synostosis. In addition, surgical exposure using our double incision technique allows excellent visualisation of the anatomical areas. This proves it to be a very convenient technique. Once the tendon is anchored, we perform all possible movements of the elbow to check for full range of motion.
One year after surgery, the mean pain score on the VAS scale was almost 2. Similar results have been published by other authors using other methods.18 However, we found that assessing pain to evaluate the benefits of this technique is irrelevant, since the patients presented hardly any pain, including the patient with a posterior interosseous injury, who, despite presenting neuroapraxia, had no pain. We find that other parameters are more useful to evaluate this surgical procedure. Indeed, pain, along with motion, stability, and function, was assessed with the MEPS scale. The patients included in this study showed a median score of 90 out of 100 at 12 months, which we consider an excellent result and in line with that published by other authors.19 We observed a statistically significant difference in MEPS score between the patients who had received some form of treatment for another medical reason and those who had received no treatment at all; the MEPS score was lower in the former than in the latter. Although we have no clear explanation for this, one could speculate that drug treatments might influence patients’ ability to heal or their own perception of their ability to heal, which could be reflected in the MEPS score. We believe that the MRC scale is another useful parameter to assess the benefits of this technique, used to measure muscle strength after surgery. The results obtained with respect to the MRC scale showed that most of the patients (73.9%) had full motion against resistance (score 5) and the rest (26.1%) had almost full motion against gravity and against resistance compared to the healthy contralateral side at 12 months after surgical treatment. These results demonstrate that after surgery the patients had regained their muscle function and were able to return to sport and reach the same sporting levels as before the injury. Finally, ROM was measured to evaluate the patient's progress. Here, we found that 12 months after surgery, the patients presented almost normal levels of motion (137.17° mean extension and −6.96° average flexion, considering that 145° and 0°, respectively, are the normal ROM of the elbow). These results show that our technique can restore full arm function, which helps patients return to sport.
A major advantage of the two-incision approach is that it allows more anatomical reinsertion of the avulsed distal biceps brachii tendon over its insertion in the radial tuberosity compared to the single anterior incision. Rollo et al.,20 using their own modification of the two-incision approach, conclude that the technique gives very good results because the anatomical structures are preserved. Tarallo et al.,19 in a study of the advantages and disadvantages of anatomical repair using the two-incision technique in 63 patients, concluded that, although the most serious complications that can occur are nerve palsy and reduced motion, the technique is a valid treatment option, especially in young active patients, in whom flexion and supination strength are restored thanks to the anatomical reinsertion.
Although there are studies and series that speak of the benefits of early mobilisation of the reinserted tendon,18,21 we agree with Prof. Bernard F. Morrey2 that, when reinsertion is performed using suture anchors, we doubt that it is strong enough to allow early mobilisation. In our series we had no cases of stiffness and mobilisation in all the cases treated was satisfactory. Therefore, for our own peace of mind we opt for joint mobilisation and starting rehabilitation treatment after 4 weeks of immobilisation if we have used the two-incision approach for reconstruction.
This study's main limitation is its retrospective design. In its favour is that all the patients followed the same treatment and follow-up protocol. Another limitation of the study is its small sample size. However, considering the very low incidence of this type of injury and the consistency of the results, this relatively small number of patients included should not be a serious limitation of the study. The main strength of the study is the consistency of the results obtained. Indeed, the small degree of variation found among the patients included in the study strongly supports the conclusions of the paper.
In conclusion, the double incision surgical approach for anatomical repair of distal biceps brachii tendon rupture is safe, provides good clinical results and allows patients to return to sport at pre-injury levels.
Level of evidenceLevel of evidence IV.
FundingThis work was funded by the Fundación Dr. Pedro Guillén.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank Mario Wensell for the critical review of the manuscript.
Please cite this article as: Ibáñez E, Araiza E, Rodríguez-Iñigo E, Guillén-García P, López-Alcorocho JM. Reparación anatómica de las lesiones del tendón distal del bíceps braquial utilizando la técnica quirúrgica de doble incisión. Rev Esp Cir Ortop Traumatol. 2021;65:305–311.