Treatment of acute complex fracture-dislocation of the elbow has been associated with a high rate of complications. Internal Joint Stabilizer of the Elbow (IJSE) device appears as a valid option to optimise and improve our results.
Material and methodsWe present a retrospective case series of five patients treated at our institution with IJS-E System (Skeletal DynamicsR) from February 2019 to 2020. Our inclusion criteria was: patients over 18 years old surgically treated with IJS-E due to persistent elbow instability despite of a suitable osteoligamentous surgical repair.
ResultsWe obtained a total of five patients (4 males and 1 female) with an average age of 37.4 years old (24–71). The Injury pattern was posterolateral instability, TTIE in all cases. The mean final postoperative MEP score was 94 points (85–100) and the postoperative DASH score was 11.78 points (4.2–20.6) with an average follow-up of 9.8 months (6–12). We described a final arc of motion of 134° with a range of flexion between 120° and 140° and a mean lack of extension of 12° (5°–20°), with a complete arc of pronosupination. As complications we found one case of heterotopic ossification and one case of elbow stiffness. However, no complications device-related or articular incongruence were reported during follow-up.
ConclusionsThe IJS-E device appears as an effective alternative instead of external fixation. Nevertheless, a high rate of reoperation up to 100% is associated with IJS-E. A larger series, longer follow-up and prospective studies are needed to define properly his role in the surgical treatment of acute elbow instability.
El dispositivo de fijación interna IJS-E se ha planteado recientemente como una alternativa válida a la fijación externa y/o transarticular en la adyuvancia del tratamiento quirúrgico de la inestabilidad aguda compleja persistente de codo tras una correcta reparación osteoligamentosa.
Material y métodosPresentamos un estudio retrospectivo de una serie de casos tratados con IJS-E System(Skeletal DynamicsR)entre Febrero de 2019 y 2020.Como criterio de inclusión se establece: pacientes mayores de 18 años con inestabilidad aguda de codo persistente tras una correcta reparación osteoligamentosa, tratados con fijador interno IJS-E.
ResultadosSe incluyeron un total de cinco pacientes en el estudio (4 varones y 1 mujer) con una edad media de 37.4 años (24–71 años). El patrón lesional fue el de inestabilidad pósterolateral, triada terrible de codo (TTIE),en todos los casos. El seguimiento medio total fue de 9.8 meses (6–12 meses). La puntuación DASH media fue de 11.78 (4.2–20.6) y la puntuación MEP media fue de 94 puntos (85–100). Se obtuvo un arco de movilidad final de 134°. El porcentaje de reintervención fue del 100% debido a la realización de movilización bajo anestesia asociada a extracción programada del dispositivo. Como complicaciones identificamos un caso de osificación heterotópica y un caso de rigidez que precisó de artrolisis abierta. En ninguno de los casos se identificó durante el seguimiento pérdida de congruencia articular ni otras complicaciones mayores.
ConclusionesNuestra serie de casos presenta unos resultados funcionales y radiológicos prometedores mediante el empleo del IJS-E como alternativa a la fijación externa.
Acute instability of the elbow is one of the most frequent clinical pictures in daily clinical practice. Its form of presentation can vary from simple dislocation without associated fracture to complex fracture-dislocation patterns associated with low or high energy trauma, and it is one of the most frequent reasons for ED consultation with an approximate annual incidence of 5.21 per 100,000.1,2 Correct knowledge of the anatomy and biomechanics of the elbow is therefore essential.3
A set of four traditional elbow fracture-dislocation patterns have been identified: posterolateral instability, also known as terrible triad injury of elbow (TTIE), posteromedial rotational instability, transolecranon fracture-dislocation and Monteggia fracture-dislocation. We can include in the fourth group a series of complex fracture-dislocation patterns that are difficult to describe and are often referred to as Monteggia-like lesions. Posterolateral elbow instability or TTIE is characterised by the association of the lesion with the lateral ligamentous complex (LLC), radial head fracture and fracture of the anterolateral facet of the coronoid process,4 and is a lesion traditionally associated with great instability and sequelae.
Although good functional results have been described with early surgical treatment of the lesions (in under two weeks) of this type of elbow fracture-dislocation,5–7 a high percentage of patients require measures associated with surgery such as prolonged immobilisation, in flexion, using splints or orthoses, or external and/or transarticular fixation to maintain joint stability and congruence. Hence this type of injury being classically associated with a high complication (20%–50%) and reoperation (0%–54.5%) rate in the different series published in the literature.8–15 Some of these, such as stiffness, heterotopic ossifications, nerve damage, pin infection, complex regional pain syndrome, adhesive shoulder capsulitis or peri-implant fracture around the pins are associated with limb immobilisation. Others, such as persistent instability, joint subluxation, aseptic loosening of radial head prostheses, discomfort related to the synthetic material or early osteoarthritis are associated with the severity of the lesion and the complexity in treating it.8–15
Therefore, surgeons seek ways to optimise, both conceptually and surgically, the treatment of this type of persistent elbow injury, despite correct restoration of the collateral ligament complex, radial head, and coronoid process.
Seeking these improvements, Orbay et al.16 published their preliminary results using an internal elbow fixation device based on the use of a Steinmann pin through the axis of the ulnohumeral rotation and attached to the proximal ulna with promising conclusions in favour of using this type of dynamic internal fixation technique as an alternative to external fixation. The disadvantage is that it requires a second procedure for removal of the material.
Later, in 2017, Orbay et al.17 published a multicentre study in which they presented the internal joint stabiliser of the elbow (IJS-E) (Skeletal DynamicsR) as an effective alternative to external fixation to treat complex elbow instability, obtaining functional and radiological results at least similar to external fixation with fewer complications.
The aim of our study was to analyse the clinical, functional, and radiological results in patients treated with IJS-E as an alternative to external fixation, describing potential critical points when implanting the device.
Material and methodsA retrospective study was conducted of a series of cases diagnosed with acute complex elbow instability treated with the IJS-E System (Skeletal DynamicsR) between February 2019 and 2020. The inclusion criteria were patients over 18 years of age with persistent acute elbow instability after osteoligamentous repair, treated with the IJS-E internal joint stabiliser. Persistent instability was defined as the presence or occurrence under fluoroscopic control of joint dislocation or incongruence during passive joint mobilisation in the flexion-extension arc. The exclusion criteria were patients under 18 years of age, those with complex elbow fracture-dislocation who did not have persistent instability after successful osteoligamentous repair, with acute persistent elbow instability after osteoligamentous repair treated with external fixation, and cases of chronic elbow instability.
A total of five patients were identified, all of whom had a lesion pattern of either posterolateral instability or TTIE.
In all cases a review of the medical history was performed, and data collected on demographic characteristics, mechanism of injury, pattern of instability, days of delay until definitive surgery, type of surgical approach, type of osteoligamentous repair, active joint range achieved after the surgery and active joint range achieved after removal of the device.
In addition, all the patients were contacted by telephone to make an objective assessment of their final functional status using the Disabilities of the Arm, Shoulder and Hand (DASH) and Mayo Elbow Performance (MEP) scores.
A radiological review of the images was performed to assess for potential short-term complications such as loss of joint congruence (increase or asymmetry of the joint space on anteroposterior [AP] projection, loss of radiocapitellar alignment or posterior displacement of the ulna on lateral projection), heterotopic ossifications, infection (signs of osteolysis or early mobilisation of the implant) or peri-implant fractures.
Description of the deviceThe IJS-E is a temporary internal fixation device, to ensure sufficient stability and joint congruence of the elbow throughout the range of motion, while adequate healing of the primary and secondary stabilisers occurs. To achieve this, it comprises a humeral pin placed in the axis of rotation of the elbow, which articulates through a connecting arm with a distal plate fixed with screws in the posterior region of the olecranon.
Surgical techniqueIn all cases, the surgical procedure, including placement of the device, was performed by one surgeon, a specialist in elbow surgery and previously trained in the use of the IJS-E.
With the patient in the supine position and the presence of an auxiliary hand table, antibiotic prophylaxis was administered during anaesthetic induction with cefazolin 2 g IV or vancomycin 1 g, in the case of associated drug allergy. Ischaemia was performed by compressing the limb, applying a tourniquet at the level of the middle third of the arm.
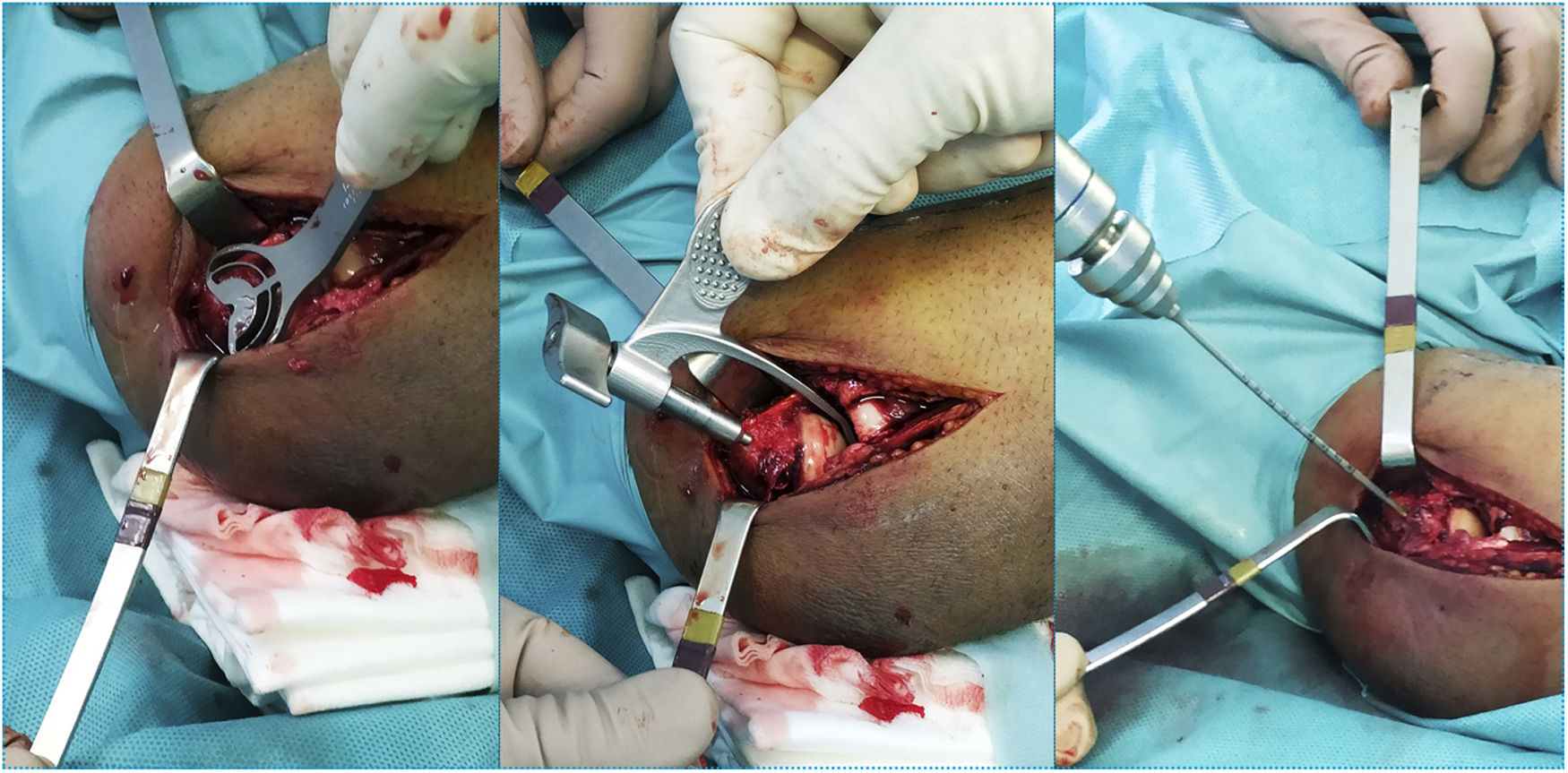
A lateral approach to the elbow was used in all five cases, given the lesion pattern of the cases included (TTIE). When approaching the muscle plane and deep planes it is important to note associated soft tissue damage, as this can indicate the potential degree of instability of the lesion being treated and the need to use the IJS-E (Image 1).
In patients who we believe could require supplementation with IJS-E to maintain stability, as well as those unable to undergo closed reduction, with dislocation beyond 90° of flexion, a new episode of dislocation after closed reduction, or associated significant soft tissue damage, we first place the humeral pin at the level of the isometric point on the distal humerus prior to the osteoligamentous repair.
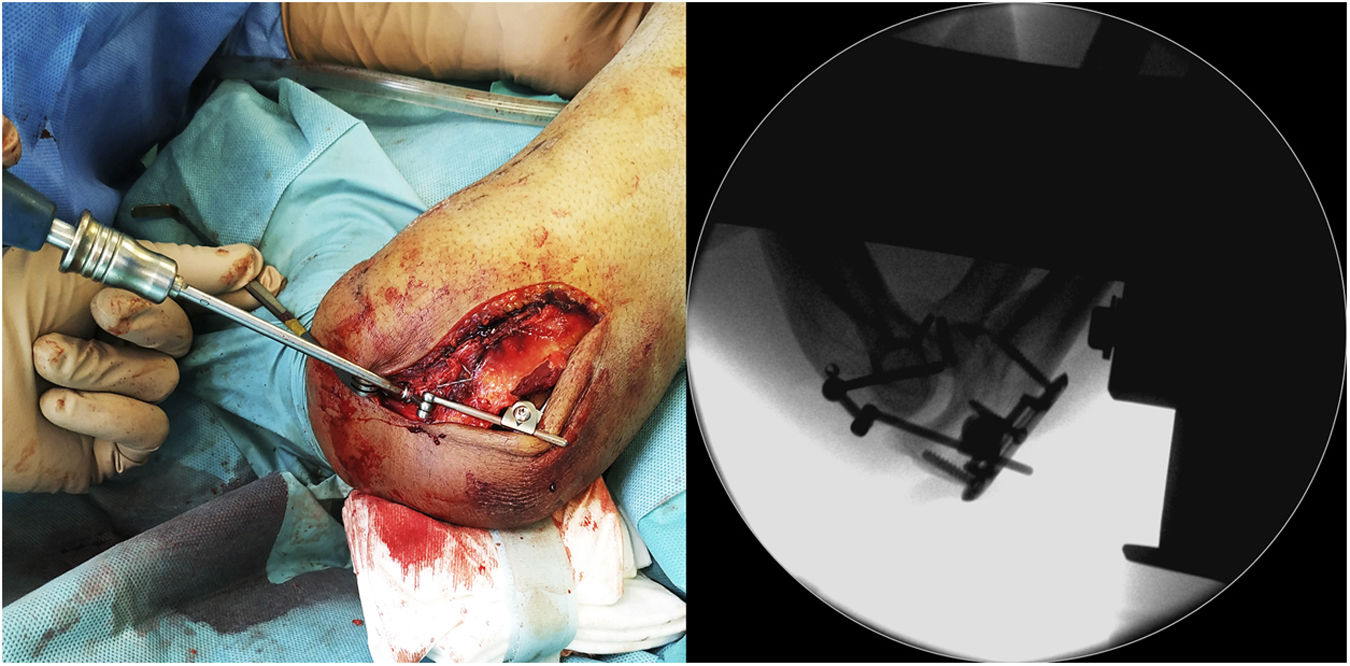
To do this, the guide wire is introduced at the level of the centre of rotation in the lateral portion of the capitellum with the aid of a fluoroscope (Image 2). The distal humerus pin (axis pin) is then placed once the correct guide wire position and length have been confirmed.
It is important to achieve a good biomechanical axis without exceeding the medial cortex due to the possibility of ulnar nerve injury, with the guide pin remaining between the trochlea and epitrochlea, parallel to the joint. It is recommended to use the shorter of the two measurements if there is any doubt between the two lengths.
This preliminary step ensures that an adequate isometric point is achieved at the level of the distal humerus, under fluoroscopic control, without potential interference such as that which might be caused by previous repair of the LLC.
The osteoligamentous repair is then performed. In terms of coronoid fractures, we found coronoid tip fractures or O'Driscoll type I fractures in all cases, none of which were repaired. The management of radial head fractures varied, depending on the type of fracture. Mason type I fractures of the radial head were managed with excision of the fragment, provided the fragment was less than 10%–20% of the joint surface. Single fragments with greater involvement of the joint surface and type II fractures were synthesized with compression screws. In the case of comminuted fractures classified as Mason type III, the radial head was prosthesised. Definitive repair of the LLC was then performed, consisting of reinsertion with a 3.5 mm harpoon inserted immediately distal to the insertion point of the IJS-E humeral pin.
After completing the osteoligamentous repair, the joint stability and congruence in total passive arc of motion in flexo-extension of the elbow is checked. If frank instability with loss of joint congruence is found, the IJS-E device is implanted following the technique described by the manufacturer (Image 3). If, on the other hand, adequate joint congruence is achieved in total passive arc of motion in flexo-extension, as well as correct stability in the coronal plane with the varus and valgus stress manoeuvres, the humeral pin is removed as it is considered that augmentation with the IJS-E device would not be necessary.
We must highlight that in patterns of complex elbow instability, bearing in mind that the patient is usually under general anaesthesia with muscle relaxation, we may observe some subluxation, especially when performing forced varus manoeuvres, which we do not consider clinically relevant for the placement of the IJS-E device if adequate joint congruence is maintained.
Once the surgical repair has been completed, careful haemostasis is recommended after removal of the tourniquet and the elbow is immobilised with a brachiobrachial padding bandage.
Postoperative managementAfter 24 h, the soft tissues are dressed and checked. From the first day, active mobilisation is allowed without restrictions, avoiding overexertion or weight bearing. A clinical check-up is carried out at one week and then at two, four, eight and 12 weeks with radiological control to assess that adequate joint reduction has been maintained and to detect potential complications related to hardware or the appearance of heterotopic ossifications.
The sutures are removed from the surgical wound in the second week, provided that the wound has progressed favourably.
Active joint balance (AJB) is measured using a goniometer at two, four, eight and 12 weeks. In our protocol, we do not use articulated elbow orthoses, since we consider that the stability obtained in the operating theatre with the device means we can start early mobilisation without restrictions, attempting to minimise stiffness as much as possible.
Intensive rehabilitation is started, beginning with weight bearing from the sixth week, adapted for cases with extraordinary circumstances, such as associated fracture of the distal extremity of the radius (DRE) as presented by two of the cases.
Between three and four months postoperatively, and following the manufacturer’s recommendation, we proceeded to the scheduled removal of the device, after measuring the AJB. With this, we assessed the need to combine manipulation under anaesthesia (MUA) or open arthrolysis in this surgical procedure. In cases with a preoperative arc of motion prior to hardware removal of less than 100°, we decided to perform intraoperative MUA to obtain a passive joint balance greater than 100°.
In cases where the arc of motion is less than 70°, as in patient 2, an open arthrolysis consisting of anterior capsulectomy and associated soft tissue contracture release will be performed first. We consider open arthrolysis the surgeon's preferred choice, as it is less surgically complex than arthroscopic arthrolysis.
In addition, if an arc of motion greater than 100° cannot be achieved with manipulation under anaesthesia, open arthrolysis would be considered in addition to removal of the material. However, this was not necessary in any of the cases presented in this series.
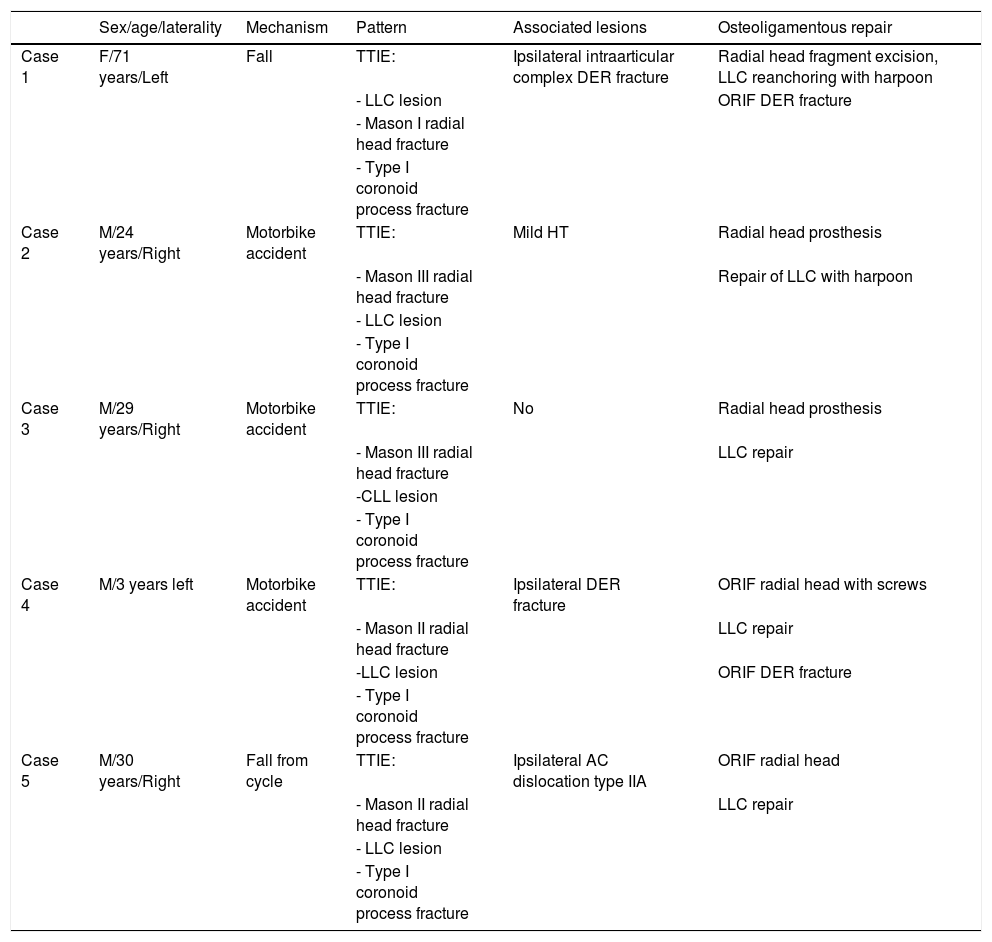
ResultsA total of five patients were identified (four males and one female) with a mean age of 37.4 years (24–71 years). In all cases, the lesion pattern was that of posterolateral instability: TTIE. The demographic data, mechanism, and pattern of injury associated injuries and type of intervention are presented in Table 1. The mean time to intervention was three days (one to seven days), with a mean final follow-up of 9.8 months (six to 12 months).
Demographic characteristics, lesion pattern and type of osteoligamentous repair.
| Sex/age/laterality | Mechanism | Pattern | Associated lesions | Osteoligamentous repair | |
|---|---|---|---|---|---|
| Case 1 | F/71 years/Left | Fall | TTIE: | Ipsilateral intraarticular complex DER fracture | Radial head fragment excision, LLC reanchoring with harpoon |
| - LLC lesion | ORIF DER fracture | ||||
| - Mason I radial head fracture | |||||
| - Type I coronoid process fracture | |||||
| Case 2 | M/24 years/Right | Motorbike accident | TTIE: | Mild HT | Radial head prosthesis |
| - Mason III radial head fracture | Repair of LLC with harpoon | ||||
| - LLC lesion | |||||
| - Type I coronoid process fracture | |||||
| Case 3 | M/29 years/Right | Motorbike accident | TTIE: | No | Radial head prosthesis |
| - Mason III radial head fracture | LLC repair | ||||
| -CLL lesion | |||||
| - Type I coronoid process fracture | |||||
| Case 4 | M/3 years left | Motorbike accident | TTIE: | Ipsilateral DER fracture | ORIF radial head with screws |
| - Mason II radial head fracture | LLC repair | ||||
| -LLC lesion | ORIF DER fracture | ||||
| - Type I coronoid process fracture | |||||
| Case 5 | M/30 years/Right | Fall from cycle | TTIE: | Ipsilateral AC dislocation type IIA | ORIF radial head |
| - Mason II radial head fracture | LLC repair | ||||
| - LLC lesion | |||||
| - Type I coronoid process fracture |
AC: acromioclavicular; DER: distal extremity of radius; F: female; HT: head trauma; LLC: lateral ligament complex; M: male; ORIF: open reduction and internal fixation; TTIE: terrible triad of the elbow.
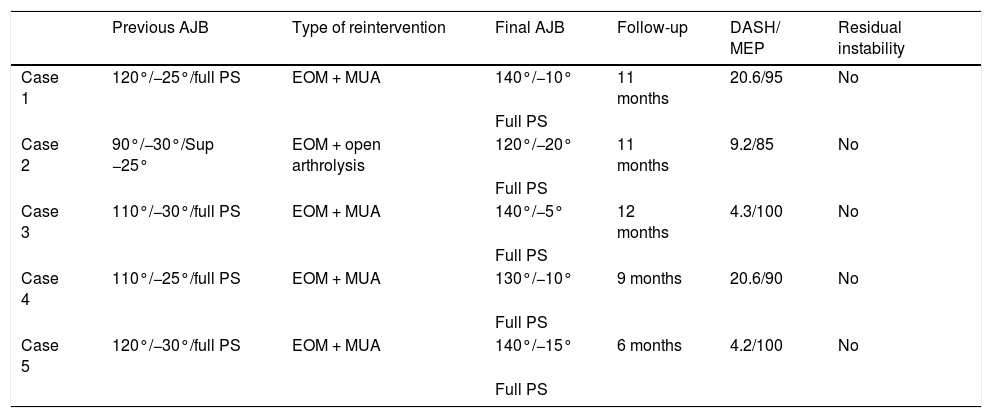
Motion prior to device removal was flexion 110° (90°–120°), extension deficit 28° (25°–30°), pronation 80° and supination 80° (60°–85°). Because the arc of motion was less than 100° in all cases, MUA was performed prior to removal of the device between 12 and 16 weeks, using the second surgical procedure scheduled for removal. After the MUA, an arc of motion greater than 100° was achieved intraoperatively in all cases. Only one case (case 2) had a previous AJB with a range of motion less than 70° related to a deficit in supination of 25°. Therefore, in this case, open arthrolysis consisting of anterior capsulectomy and soft tissue contracture release with early intensive rehabilitation was performed.
However, in none of the cases was loss of joint congruence, subluxation or persistent instability identified during follow-up prior to removal of the device. In addition, we also found no discomfort related to the implant, loosening or breakage prior to removal.
The mean AJB at the end of follow-up was flexion 134° (120°–140°), extension deficit of 12° (5°–20°) and full pronosupination. Functional outcomes were collected using the DASH and MEP scales. The mean DASH score was 11.78 points (4.2–20.6), and the mean MEP score was 94 points (85–100).
As complications in addition to the abovementioned case (case 2) who presented with stiffness, case 3 showed grade II heterotopic ossification at five months follow-up without clinical significance (Image 4). Residual instability, joint incongruity, infection, complicated haematoma, material breakage or neurovascular injury were not identified in any of the cases during follow-up. In sum, the motion values prior to removal of the IJS-E, type of reintervention and functional values are shown in Table 2.
Functional results and type of reintervention.
| Previous AJB | Type of reintervention | Final AJB | Follow-up | DASH/ MEP | Residual instability | |
|---|---|---|---|---|---|---|
| Case 1 | 120°/−25°/full PS | EOM + MUA | 140°/−10° | 11 months | 20.6/95 | No |
| Full PS | ||||||
| Case 2 | 90°/−30°/Sup −25° | EOM + open arthrolysis | 120°/−20° | 11 months | 9.2/85 | No |
| Full PS | ||||||
| Case 3 | 110°/−30°/full PS | EOM + MUA | 140°/−5° | 12 months | 4.3/100 | No |
| Full PS | ||||||
| Case 4 | 110°/−25°/full PS | EOM + MUA | 130°/−10° | 9 months | 20.6/90 | No |
| Full PS | ||||||
| Case 5 | 120°/−30°/full PS | EOM + MUA | 140°/−15° | 6 months | 4.2/100 | No |
| Full PS |
DASH: disabilities of the arm, shoulder, and hand; EOM: extraction of osteosynthesis material; MEP: Mayo elbow performance; MUA: manipulation under anaesthesia; PS: pronosupination.
This case series presents the introduction of the IJS-E device into our surgical protocol for the treatment of persistent acute complex instability of the elbow despite successful osteoligamentous repair as a potentially valid alternative to external fixation. The mean follow-up of our five patients was 9.8 months, with a final arc of motion of 122° flexion-extension with full pronosupination. The DASH and MEP scales averaged a score of 11.78 and 94 points, respectively, which translates into an excellent final functional outcome. In all cases, adequate joint congruence was achieved, allowing immediate and early initiation of active postoperative mobilisation. However, when assessing the results obtained, we must consider that a MUA was performed in all cases, coinciding with the scheduled removal of the device.
Early surgical treatment by repair/reconstruction of primary lesions in TTIE has been associated with good functional outcomes despite the need for transarticular or external fixation as augmentation elements in their treatment. Lindenhovius et al.5 present good functional results with a final flexion arc of 119° and a Broberg and Morrey functional scale of 90 points after protocolised surgical treatment in a total of 18 patients with TTIE. The authors performed a complete osteoligamentous repair of the elbow, including the coronoid process. No case required application of external fixation and they do not indicate the type of subsequent immobilisation or post-surgical rehabilitation protocol used. These results were inferior in the case of a subacute repair (after two weeks) with an average flexion-extension arc of 100°, although maintaining good functional results at 87 points on the Broberg and Morrey scale. In this second cohort, they used external fixation in all cases. However, they do not indicate for how long or the type of postoperative protocol for functional recovery.
Pugh et al.13 and McKee et al.9 achieved similar results in their respective series with an average arc of motion of 112° and 105°, respectively. Álvarez et al.,7 in their series published in 2019 with a total of 62 TTIE treated in a protocolised manner, present good results with an average flexion-extension arc of 100° and mean values on the MEP scale of 92 points. It should be noted in this series that up to 22% of cases required static external fixation, with a complication rate of 27%, the most frequent being nerve injury.
Regarding adjuvancy of primary repair, Ring et al.10 compared external fixation and transarticular fixation, describing a higher percentage of complications associated with external fixation (50% compared to 10%), although with good functional results in both groups: 90 points on the Broberg and Morrey scale and average flexion-extension range of motion of 100°. Other series published in the literature show similar results in motion using external fixation: 109°,12 120°,18 and 105°.11
Orbay et al.17 used the IJS-E device that they had designed themselves in a total of 24 patients as an alternative to external fixation. Their final reported average range of motion was 119° for flexion-extension and 152° for pronosupination, with a minimum follow-up of six months for the treatment of both acute and chronic instability. Other research studies on the IJS-E19,20 give similar results with average flexion-extension of 124° and 106°, respectively, and with a mean final follow-up of 11.3 and 13.4 months. In our series, we achieved values similar to the abovementioned with a flexion-extension arc of motion of 122° and full pronosupination. Unlike other previously published studies, we should mention that we did not include cases of chronic instability.
In our series the DASH score averaged 11.78 points (4.2–20.6) and the MEP score 94 points (85–100); it was more than 90 in four of the five cases presented. These scores represent excellent functional results, being slightly higher than those previously published in other studies with IJS-E devices showing DASH scores in the range of 16–37.3 points.17,19,20 These results also seem to be better than those reported in series using the external fixator as adjuvancy, with DASH scores ranging from 9 to 31 points,5,8,12,21 and MEP scores between 78 and 95 points. This small positive difference may be because, in our series, the IJS-E device was only used in patients with acute elbow instability, with a fewer lesions associated with the diagnosis and the absence of major complications in the short-term follow-up such as infection, persistent dislocation, ulnar and median nerve injury or the need for medial collateral ligament reconstruction described in other studies.17,19,20
In our series MUA was linked to scheduled device removal in patients with an arc of motion of less than 100° between 12 and 16 weeks. The primary objective is to gain an extra point of articular arc. However, we must bear in mind that it must be performed within safety margins, avoiding excessive abrupt manipulation, to obtain a functional arc of motion and never seek complete joint balance. In this way, we minimise potential complications and we stress the importance in the immediate postoperative period of early, intensive rehabilitation with the active collaboration of the patient to achieve optimal results.
As in cases with external fixation or cross-pinning, in which the material must be removed, the IJS-E must be explanted after three to four months.17,20 The internal fixator should be removed in a second surgical procedure through two small incisions. As the requirement for this procedure is known in advance and is included on the product's data sheet, it is expected that 100% of patients will be reoperated. Nevertheless, this procedure should not be considered a complication, but a part of the treatment. In all cases the device was removed between 12 and 16 weeks, following the manufacturer's recommendations.17 Pasternack et al.20 agree on the elective removal of the device in all cases, suggesting it could be removed after six weeks depending on the radiological findings at follow-up, reporting a mean IJS-E maintenance period of 74 days without discomfort or breakage of the material. In contrast, Sochol et al.19 treated a total of 20 patients (nine cases of acute instability) without scheduled device removal unless requested by the patient or in the event of complications. In this series, only six devices (30%) were removed. We believe, because we do not know the potential complications associated with maintenance of the device long term, it is more prudent to follow the manufacturer's recommendations pending further evidence.
One of the main problems classically associated with the treatment of TTIE is the high percentage of complications and reoperation, often related to external and transarticular fixation.8–15 Superficial infection of the pins, peri-implant fracture when inserting the pins, pseudoarthrosis of peri-implant fracture and nerve damage, especially to the radial and ulnar nerve are more specifically associated with external fixation.5,8–15 The recent advent of the IJS-E theoretically seeks to minimise this complication rate, especially complications related to stiffness, infection and nerve injury. Orbay et al.17 report two patients with heterotopic ossifications (preoperatively) and only one individual with superficial infection as complications. No cases of nerve injury or implant-related discomfort were observed.
Sochol et al.19 report a reoperation rate of 55%, regardless of the abovementioned device removal: 11 patients required arthroscopic arthrolysis, MUA or both. In addition, they reported four cases of nerve injury in the form of ulnar neuroapraxia treated with neurolysis and one case of infection treated with device removal and lavage. However, they reported no cases of joint instability or loss of joint reduction during follow-up.
Pasternack et al.20 reported a reoperation rate of 40% (four of the 10 cases treated with IJS-E). One of the patients required salvage surgery in the form of total elbow arthroplasty for early osteoarthritis. In the remaining three subjects, two were cases of ulnar stiffness and neuroapraxia treated with arthrolysis and ulnar nerve transposition, and the last complication was persistent instability treated with medial collateral ligament reconstruction.
Case 2 of our series required open arthrolysis which was performed during the same surgery as the removal of the device due to a motion arc of less than 70° prior to that surgery. In addition, case 3 had heterotopic ossification with no clinical repercussions for the patient. We report no cases of neurovascular injury, implant-related discomfort, or infection during follow-up.
Except for this case of open arthrolysis, we report no reinterventions due to potential complications in our series. In all patients, joint congruence and stability was maintained throughout the time of the device was implanted, which was the primary objective of analysis in this study.
Limitations of the studyWe are aware that this is a retrospective review case series that includes only five patients with a short mean follow-up (9.8 months).
However, we believe the presence of severe persistent elbow instability is a rare condition. Furthermore, the recent introduction of the implant (approved in 2016 by the US Food and Drug Administration) means that few patients are currently being implanted with the IJS-E. The number will increase over time, which will help towards more robust studies on the use of this device.
ConclusionsThe recent IJS-E device is presented as an alternative to external fixation in the treatment of acute persistent elbow instability after osteoligamentous repair, allowing early joint mobilisation.
Our case series presents promising functional and radiological results using this technique. However, future prospective, randomised, multicentre studies with a larger sample size are required to draw definitive conclusions on the advantages and disadvantages of the IJS-E versus external fixation.
Level of evidenceLevel of evidence IV
FundingThis paper has received no funding of any type.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Pardo-García JM, Jiménez-Díaz V, Porras-Moreno M, García-Lamas L, Cecilia-López D, Tratamiento de la inestabilidad aguda compleja de codo con fijador interno IJS-E System. Rev Esp Cir Ortop Traumatol. 2021;65:432–441.