The treatment of massive osteochondral defects in young patients constitutes a challenge for the orthopaedic surgeon. On the one hand, facing the biological filling and on the other, guaranteeing the function in the short and long term. Defects in the lateral femoral condyle are extremely rare.
We studied 7 cases of massive bone defects in the lateral condyle, 2 of them bilateral, with a median surface area of 6.8 cm2 (IQR: 4.9−7.0 cm2) and a median depth of 2.8 cm (IQR; 2.2–3.2 cm). The patients were between 17 and 21 years old, without any previous traumatic background and were treated with autologous iliac crest graft and collagen mesh (Cartmaix-Matricel). Pre and postoperative clinical (Lysholm, Tegner, Koos) and radiological tests (3d Mocart) have been carried out.
Best improvement have seen in clinical parameters have been normalized in all patients, with a return to sports activities. Likewise, the radiological defect has been recovered in all of them, subtotally but more than 50%.
Massive osteochondral defects in the lateral condyle could be treated by filling with autologous crest bone and a collagen mesh, with good clinical and radiological results, constituting a rational option in the therapeutic approach.
El tratamiento de los grandes defectos condrales en el paciente joven constituye un reto para el cirujano ortopédico. Por un lado afrontar el relleno biológico y por el otro, garantizar la función a corto y largo plazo. Los defectos en el cóndilo femoral externo constituyen una rareza.
Estudiamos 7 casos de defectos masivos en cóndilo femoral externo, 2 de ellos bilaterales, con una superficie mediana (Md) de 6,8 cm2 (rango intercuartílico (RIC): 4,9−7,0 cm2) y una profundidad mediana de 2,8 cm (RIC: 2,2–3,2 cm). Los pacientes tenían edades de 17 a 21 años, sin antecedentes traumáticos previos y fueron tratados con injerto autólogo de cresta ilíaca y malla de colágeno (Cartmaix-Matricel). Se han efectuado test clínicos (Lysholm, Tegner, Koos) y radiológicos (3d Mocart) pre y postoperatorios a los 2 años.
La mejoría más importante fue la normalización de los parámetros clínicos en todos los pacientes, con retorno a las actividades deportivas. Asimismo, se ha recuperado el defecto radiológico en todos ellos, de forma incompleta, pero en más del 50%.
Los defectos masivos osteocondrales del cóndilo femoral externo pueden tratarse mediante relleno de hueso autólogo de cresta más malla de colágeno, con buenos resultados clínicos y radiológicos, constituyendo una opción racional en su enfoque terapéutico.
Chondral defects may condition functional limitations, especially in young, active patients. Most of these defects are superficial and are sometimes associated with other joint lesions such as meniscal or ligament damage, but on occasion they may appear in isolated form with their appearance being idiopathic.
In young patients, juvenile osteochondritis dissecans usually affects the internal femoral condyle, and although several causes have been reported, the most common is essential or idiopathic. In this entity, involvement of the lateral condyle is much less common (15%).1 It is a rarity and in conditions regarded as stable, the treatment is rest or fixation with osteosynthesis, which usually suffices.
Massive osteochondral defects are much less common and particularly those affecting the lateral femoral condyles, which are the purpose of this study. Several different therapeutic options have been proposed for their treatment, including structural bone graft or even prosthetic replacement, although the latter would not be contemplated as first line treatment.
Chondrocyte grafts produce good outcomes, as do frozen osteochondral grafts.2
Among the many options, treatment using autologous graft combined with collagen mesh may have the advantage on being a simpler and more reproducible technique in all hospital centres, and may improve the outcomes of other alternative treatments with regards to clinical and radiologic results.
The aim of this study was to evaluate the results of these massive defects through autologous bone graft of the iliac crest, combined with collagen mesh (Cartimaix-Matricel).
Material and methodsFrom December 2016 until January 2018 prospective data from 52 cases of massive osteochondral defects (>4 cm2) in femoral condyles were collected, of which 38 belonged to young patients in the first 2 decades of life. Of these, 31 cases were defects which affected the internal femoral condyle and 7 cases (5 patients) the external femoral condyle.
All cases were operated on in the same centre by the same surgical team, using autologous graft and collagen mesh, except in medial femoral condyles where other techniques were used, such as ostechondral fixation and perforations.
This study included patients affected by external lateral condyle defects. Of these 7 cases, 2 were bilateral, all were young males with a median age of 18 years, with an interquartile range of 17–20 years (Table 1). None of the patients presented with a previous disease or history of trauma, or changes to metabolism or obesity. All patients presented with a normal axis (0−3° varus). Regarding sports activity, all played impact sports: 3 football, one basketball and one motorcycling. No defect met with fixation criteria, and therefore in all of them the fragments were loose, ivory-coloured bodies, which were smaller than the defects in question, and in all cases there were several fragments. Nonetheless, only 2 cases presented with loose bodies with blockages.
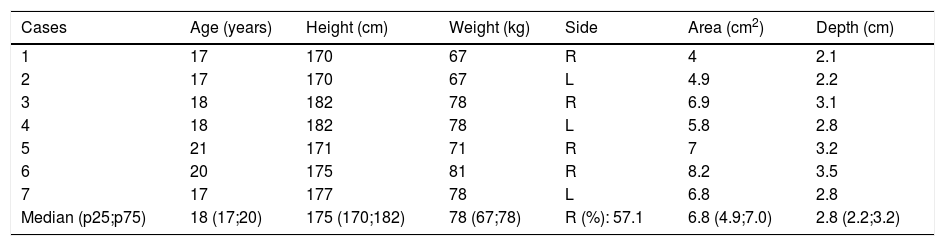
Baseline table.
| Cases | Age (years) | Height (cm) | Weight (kg) | Side | Area (cm2) | Depth (cm) |
|---|---|---|---|---|---|---|
| 1 | 17 | 170 | 67 | R | 4 | 2.1 |
| 2 | 17 | 170 | 67 | L | 4.9 | 2.2 |
| 3 | 18 | 182 | 78 | R | 6.9 | 3.1 |
| 4 | 18 | 182 | 78 | L | 5.8 | 2.8 |
| 5 | 21 | 171 | 71 | R | 7 | 3.2 |
| 6 | 20 | 175 | 81 | R | 8.2 | 3.5 |
| 7 | 17 | 177 | 78 | L | 6.8 | 2.8 |
| Median (p25;p75) | 18 (17;20) | 175 (170;182) | 78 (67;78) | R (%): 57.1 | 6.8 (4.9;7.0) | 2.8 (2.2;3.2) |
L: left R: right.
All the patients presented with pain, which was described according to the visual analogue scale (VAS 6/10: one case; 7/10: 2 cases; 8/10: 2 cases) and with major functional limitations in the preoperative period.
Defects had a median area of 6.8 cm2 (interquartile range [IQR]: 0.0 4.9−7.0 cm2) and a median depth of 2.8 cm (IQR: 2.2–3.2 cm). Preoperative levels are contained in Table 1.
The defects were measured intraoperatively and did not differ from those analysed in the magnetic resonance imaging (analysed and measured with the RAIM programme).
In all cases the radiologic exploration was performed with tele-radiology, with anteroposterior, profile and Fick radiographs, together with a magnetic resonance (tesla 1.5).
All patients were operated on with open and extensive arthrotomy, by internal parapatellar approach lateralising the patella and with preventative ischaemia, in order to appropriately fill and compact the cancellous bone and mark out the mesh area better (Image 1). We used the anterior and medial route in all massive chondal defect surgery so as to avoid medial or lateral scars which could interfere in later surgery should it be required, thus avoiding possible skin necrosis. The mesh used (Cartimaix-Matricel) is a collagen I/III and elastin matrix biodegradable membrane type, bi-layered structured: porous on the joint side and flat on the defect side to protect clotting and facilitate the settlement and proliferation of the pluripotent cells. The mesh is cut marking out the contours of the defect and stuck with tissue adhesive (Tisseel-Baxter) on both sides. This mesh has a joint side and a bone side and for this reason we mark the joint side so as not to get confused (marked with a cross on the joint side in Image 1). It is important to know that the mesh increases in size by approximately 10% upon hydration, and this should be taken into account during preparation. After this, it is left to dry for 5 min to proceed with layered closure and the attachment of a compression bandage. The preventative ischaemia is then removed, with no aspiration drainage to ensure good sealing of the defect.
The 2 patients affected bilaterally were operated on their knees consecutively. In other words, 3 months passed between operating on the first knee and the contralateral one. The results shown correspond to 2 years from the most recent surgery.
Postoperative procedure consisted in immobilising the knee with a brace for 6 weeks in extension and total non weight bearing of the limb for 3 months. After 3 months partial progressive weight bearing was allowed until total weight bearing at 6 months. At 9 months they were allowed to carry out sports activities in closed kinematic chain such as walking swimming or cycling and after one year normal life was resumed.
ResultsDemographic data is reflected in Table 1. These were young patients, all of whom were male, none overweight, all with normal axes and no predominance of side.
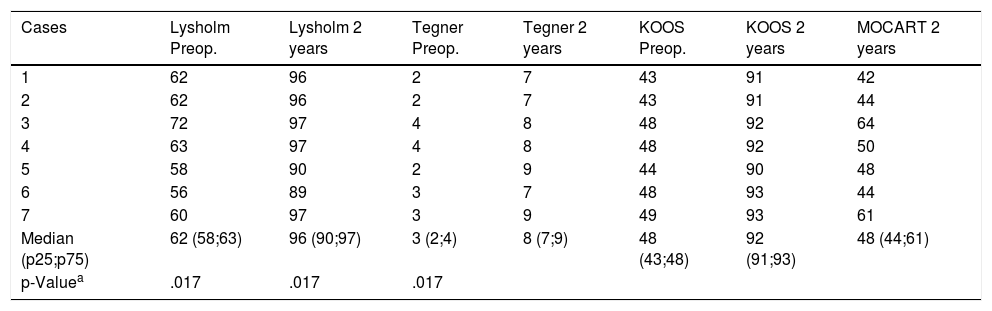
The patients were studied using clinical tests at the beginning and after 2 years; Lysholm who studied function, Tegner to evaluate the return to sports and KOOS who assessed the quality of life. The results at 2 years are contained in Table 2.
Results at 2 years.
| Cases | Lysholm Preop. | Lysholm 2 years | Tegner Preop. | Tegner 2 years | KOOS Preop. | KOOS 2 years | MOCART 2 years |
|---|---|---|---|---|---|---|---|
| 1 | 62 | 96 | 2 | 7 | 43 | 91 | 42 |
| 2 | 62 | 96 | 2 | 7 | 43 | 91 | 44 |
| 3 | 72 | 97 | 4 | 8 | 48 | 92 | 64 |
| 4 | 63 | 97 | 4 | 8 | 48 | 92 | 50 |
| 5 | 58 | 90 | 2 | 9 | 44 | 90 | 48 |
| 6 | 56 | 89 | 3 | 7 | 48 | 93 | 44 |
| 7 | 60 | 97 | 3 | 9 | 49 | 93 | 61 |
| Median (p25;p75) | 62 (58;63) | 96 (90;97) | 3 (2;4) | 8 (7;9) | 48 (43;48) | 92 (91;93) | 48 (44;61) |
| p-Valuea | .017 | .017 | .017 |
All patients improved in function to scores which were considered good, returned to demanding sports practising after a year and achieved a good or excellent quality of life. The statistical significance of the change in pre and postoperative scores was researched using the Wilcoxon test, demonstrating improvement in the 3 functional indexes.
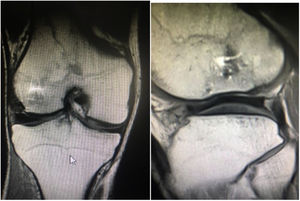
On a radiological level they were assessed after 2 years on the 3D magnetic resonance observation of cartilage repair tissue (MOCART) score scale. All patients showed patterns of similar repair, incomplete repair of the defect but >50%, without hypertrophies, interphase of the cartilage marking a visible edge, a surface area affected to <50% of depth, with correct adhesion and homogenous structure, signal intensity almost normal, intact subchrondral laminate, intact subchondral bone and with no effusion. A coronal and sagittal image may be appreciated in one of the cases after 2 years of follow-up (Image 2). A mean result of 50.43 points was obtained (range: 42–64) over a maximum of 100 (0–100). Furthermore, no association could be established between the KOOS and MOCART values after 2 years (coefficient of lineal correlation®: 0.410; p-value: .361).
None of the patents presented with complications from surgery, and evolved favourably.
DiscussionThe cases described in this study are a rarityAt present no series has been published on massive chondral defects treatment of the external femoral condyle in young patients and therefore we had no references to guide us regarding the most appropriate treatment for these patients.
Chondral defects are more common in males and occur in 85% of cases in the medial condyle, with only 25% of cases being bilateral.1 In our series all the patients were male and 2 of them bilateral in keeping with the general rate of these lesions.
If we extrapolate the treatment of osetochondritis dissecans, we see that on certain occasions they are usually treated using osteosynthesis of the loose fragment or even rest and immobilisation of the limb in stable fragment, although in our case we found several loose fragments, ivory in colour and smaller in size than the defect and only 2 patients presented with cracks and joint blockage. In all cases the defects which we described in our series are massive defects and were therefore therapeutically challenging.
This is even more demanding still in a young patient, where the possibilities of arthroplasty should be carefully examined. Also, the fact that it occurs in the lateral compartment implies an additional difficulty on being the external compartment, one with greater mobility than the internal one.
With these defects, we prefer autologous bone fill aimed at ensuring its maximum viability, obtaining a levelled joint line. Once achieved, the defect is sealed with a dual-purpose collagen mesh. Firstly it provides biological lattice capable of promoting cellular growth and secondly it provides a primary stabilisation element of support to the bone graft, sealing the mesh with fibrin.
The use of meshes which include chondrogeneis are well recognised in the literature and produce promising outcomes.3,4 Bertho et al., described a study of 13 cases, 9 of which had previous surgery, treated with meshes with similar outcomes to those obtained in our series, although the patients studied presented with defects of slightly lower dimensions than those of our series. In their series the results continued being stable after the first year, similarly to our study. In a meta-analysis Zamborsky et al. reported the advantages of different techniques of cartilage repair concluding that techniques such as MACI, ACI or in combination with meshes presented better results than isolated micro-fractures.
Choosing arthrotomy has a dual aim. Although it is true that these meshes may be arthroscopically positioned,5 adding compacted bone did not ensure acute anchorage. Also, an anterior approach meant that in the event of a possible fitting of a prosthesis in the future the same access route would be available, avoiding several scars which could interfere in this.
We ruled out mosaicplasty due to the sizable defects. We also avoided the use of cryo-preserved structured grafts, due to their disputed results in young patients.2 Different authors published good results in femoral head lesions in patients affected by severe chondral defects, and meta-analysis supported good outcomes with fresh or cryo-preserved allographs in knee defects.6,7 At present, the application of biological treatments such as platelet-rich plasma or pluripotent mesenchymal cells in the treatment of chondral defects is an increasingly normal occurrence, normally as a coadjutant treatment, although in our centre we did not use it because they were not available. In our case there was a lack of a clearly structural element such as the autologous bone to fill in the defects. Some published studies enrich collagen meshes with these biological adjuvants with promising outcomes. 8 Other studies suggest the same combination of graft and mesh with good results in the internal femoral condoyle, even with a MOCART score higher than ours.9
Although in the operating theatre the aim is to always achieve a levelling of the defect, we realised that in magnetic resonance performed after 2 years, this was partially lost in all cases by approximately 1 mm of joint line. We are aware that on occasion hypergrowth may occur and therefore it is difficult to know to what extent and where the filling is to go to then apply a mesh which increases in size by approximately 10% upon hydration. No second-look arthroscopies were performed in any patients because of favourable clinical evolution and because it was not strictly necessary to subject patients to “only “revision surgery, this was ruled out.
Regarding postoperative measure of immobilisation we were more restrictive than most authors consulted. Treating very young patients and with very large defects was a determining factor in prolonging times of immobilisation, no weight-bearing and reincorporation to sports activity, compared with other series.
A limitation of this study is that we are unaware of both the long term evolution of neocartilage and also the quality of the histology of the neoformed tissue, since no biopsies exist.
Another limitation is the lack of a comparative study with other techniques used to treat these defects, although the rarity of the cases impedes extensive series being made to randomise treatments.
After the good clinical results obtained, and bearing in mind that the series is testimonial, we can state that the treatment of massive chondral defects in external femoral condyles of young patients using iliac crest autologous graft and collage mesh (Cartimaix-Matricel), is an option to be considered.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Villalba J, Peñalver JM, Sánchez J. Tratamiento de los grandes defectos osteocondrales de cóndilo femoral externo en pacientes jóvenes mediante autoinjerto y malla de colágeno. Rev Esp Cir Ortop Traumatol. 2021;65:317–321.