Osteosarcoma is the most frequent malignant spinal tumour in the paediatric age group. Diagnosis and early treatment of this pathology is essential for a good prognosis. The aim of this study was to present the results of treatment of paediatric patients with lumbar osteosarcoma and conduct a literature review.
Material and methodsAll the patients with lumbar osteosarcoma who were operated between 2012 and 2014 in the same centre were included. Demographic and radiological data (Enneking, WBB and Tomita classification), as well as anatomopathological (Broders classification) variables were analysed. All the patients were treated by surgical resection associated with adjuvant therapies (chemotherapy and radiotherapy); according to consensus with the tumour committee. The average follow-up was 62.53 months (47–70 months).
ResultsA total of 3 patients were studied, two girls of 9 and 11, with L5 osteosarcoma, and a 15-year-old boy with L4 osteosarcoma. Two of the cases were initially treated as an osteoblastoma, supported by radiological and anatomopathological images. None of the patients had local recurrences or metastases during follow-up.
ConclusionsDue to a lack of long series of cases of osteosarcoma in the mobile spine during childhood, the optimal treatment and prognosis in these patients is uncertain. Block resection improves local control of the disease, without demonstrating improvement in overall survival. Intralesional resection is associated with a higher rate of local recurrence. Oncological treatment is essential in the treatment of this pathology. A correct differential diagnosis of the tumour (osteosarcoma vs. osteoblastoma) is vital for its correct treatment.
El tumor maligno de raquis más frecuente en la edad pediátrica es el osteosarcoma, su diagnóstico y tratamiento precoces son esenciales. El objetivo del presente trabajo es el presentar los resultados obtenidos en el tratamiento de pacientes pediátricos con osteosarcoma lumbar y realizar una revisión de la literatura.
Material y métodosSe incluyeron aquellos pacientes pediátricos intervenidos de osteosarcoma de columna móvil entre 2012 y 2014 en el mismo centro. Se analizaron datos demográficos, radiológicos (clasificaciones Enneking, WBB y Tomita) y anatomopatológicos (Broders). Todos fueron tratados mediante resección quirúrgica, asociada a distintos protocolos oncológicos (radioterapia y/o quimioterapia) según consenso del comité de tumores. El seguimiento medio fue de 62,53 meses (47-70 meses).
ResultadosSe presentan un total de 3 pacientes, dos niñas de 9 y 11 años con osteosarcoma en L5 y un niño de 15 años con osteosarcoma en L4. En dos de los casos se trató inicialmente como un osteoblastoma, ya que las imágenes radiológicas y anatomopatológicas así lo apoyaban. Ninguno de los pacientes presentó recidivas locales ni metástasis tras la cirugía definitiva.
ConclusionesLos casos descritos en la literatura sobre manejo de osteosarcoma vertebral en columna móvil en la infancia son escasos, por lo que el tratamiento óptimo y pronóstico en estos pacientes es incierto. La resección en bloque mejora el control local de la enfermedad, sin demostrar que mejore la supervivencia global. La resección intralesional se asocia a mayor índice de recidivas. Un correcto diagnóstico diferencial del tumor (osteosarcoma vs. osteoblastoma) es vital para su tratamiento.
Malignant bone tumours in the paediatric age group account for around 5% of all malignant neoplasms, Ewing's sarcoma and osteosarcoma being the most frequent.1 Osteosarcoma (OS) is the most prevalent in the paediatric spine followed by Ewing's sarcoma, lymphoma and metastatic neuroblastoma.2
The annual incidence of OS3,4 is 4.7 cases per million children. Only 4%–5% of all primary OS are located in the spinal column,4–7 the lumbar region being most affected, with a higher incidence between the ages of 10 and 20.
The radiological and histopathological appearance depends on the type of matrix that the tumour produces. Most are osteoblastic and are usually seen radiologically as expansive tumours with increased or reduced density, or mixed pattern, which cause a soft tissue mass.6 They tend to affect the vertebral body and frequently extend to the pedicles and medullary canal (in up to 80% of cases).6 If metastases appear, they tend to be due to haematogenous dissemination to the lung.
When there is no mass in the adjacent soft tissues there can be radiological confusion with osteoblastoma. Ilaslan et al. reported that of the 198 vertebral OS of their series, up to 10% of the radiological images were indistinguishable from osteoblastoma.7 Histologically, there is a subtype of osteosarcoma known as osteoblastoma-like osteosarcoma (OBLOS).8 Unlike osteoblastoma, which is a benign bone tumour, OBLOS are malignant lesions that if not appropriately treated have a high mortality rate. Radiologically and histopathologically both entities are very difficult to differentiate9; differentiation is essential, because the treatment will be drastically different.
Clinically OS can start with back pain or neurological symptoms (present in 40% on diagnosis).6
Although these tumours are rare, prompt diagnosis and treatment are essential for a good prognosis. Complete resection with adjuvant and neoadjuvant chemotherapy is currently the most effective treatment,10 nevertheless, survival of these tumours remains poor.3 Aggressive resection improves neurological and functional status, as well as survival,10 but curative resection with free margins is still a handicap due to the anatomical characteristics of the spine. Advances in surgery have enabled en bloc resection of vertebral OS in selected adult patients, which, combined with adjuvant and neoadjuvant treatment, has been associated with increased survival.
According to the SEER database (U.S.A.), the mean survival rate of spinal OS for adults with an isolated lesion is 18 months, whereas it is 7 months2,3 for those with distant metastases.2,3 In childhood the mean survival rate is 29.5 months6; it seems that this increase is associated with a better response to chemotherapy.11
To our knowledge there are no long series that demonstrate the effects of resection on survival of OS of the mobile spine in childhood.
The aim of this paper is to present 3 paediatric patients with vertebral osteosarcoma treated with surgery, oncological treatment (chemotherapy and/or radiotherapy) and the outcomes achieved, and a review of the literature.
Material and methodsAll patients treated in the same hospital for vertebral osteosarcoma in the mobile spine, under the age of 18, between 2012 and 2014, were included in the study. All the patients underwent diagnostic radiography, and MRI. If a tumour was suspected, a biopsy was performed prior to the definitive surgery, except for case C who underwent a biopsy during the same operation because the lesion was suspected to be benign.
The classification systems of Enneking,3,12 WBB13 and Tomita3,14,15 were used to stage the lesions with radiological measurements, with the RIS® radiological viewer and Broders’16 anatomopathological classification (according to the number of undifferentiated malignant cells found in the sample).
Disease extent studies were undertaken for all the cases which were negative and subsequently assessed together with the oncology department and tumour committee, to decide on the oncological treatments.
In addition to controls of the lumbar spine, subsequent oncological follow-up was performed by computerised tomography (CT) of the chest alternated with plain chest X-ray every 4 months for the first year, and every 6 months for the second, finally annual controls were performed after the third year following surgery. The mean follow-up was 62.53 months (47–70 months): all 3 cases are free from local and distant disease.
Finally, a search of the literature was performed in Pubmed and Bireme using the keywords: “osteosarcoma, lumbar vertebrae, adolescent, child”.
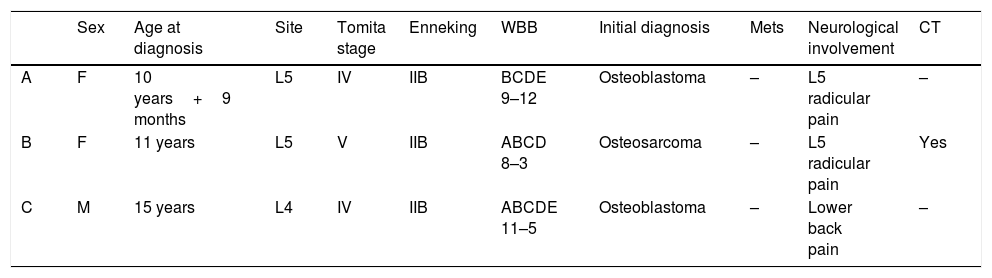
ResultsTwo of the cases we present (patients A and B) are female, aged 9 and 11 at the time of diagnosis, presenting with a primary osteosarcoma in L5. The third case (patient C) is a male with a tumour at L4 diagnosed at 15 years of age that was initially treated in another centre and referred after the tumour recurred. They are described later in detail (Tables 1 and 2).
Patients with lumbar osteosarcoma.
| Sex | Age at diagnosis | Site | Tomita stage | Enneking | WBB | Initial diagnosis | Mets | Neurological involvement | CT | |
|---|---|---|---|---|---|---|---|---|---|---|
| A | F | 10 years+9 months | L5 | IV | IIB | BCDE 9–12 | Osteoblastoma | – | L5 radicular pain | – |
| B | F | 11 years | L5 | V | IIB | ABCD 8–3 | Osteosarcoma | – | L5 radicular pain | Yes |
| C | M | 15 years | L4 | IV | IIB | ABCDE 11–5 | Osteoblastoma | – | Lower back pain | – |
| Tumour resection Sx | Histology | Sx | RT pos | Local recurrence | Sx | Mets | Follow-up | |
|---|---|---|---|---|---|---|---|---|
| A | Intralesional | Osteosarcoma | Corpectomy+interbody mesh+posterior fixation | Yes | No | – | No | 72.8 months |
| B | Corpectomy+posterior fixation | Osteosarcoma | – | Yes | No | – | No | 50.2 months |
| C | Laminectomy+biopsy | Osteoblastoma | – | No | Yes | Hemicorpectomy+posterior fixation | No | 64.6 months |
M: male; F: female; Mets: metastasis; CT: chemotherapy; Sx: surgery; RT: radiotherapy.
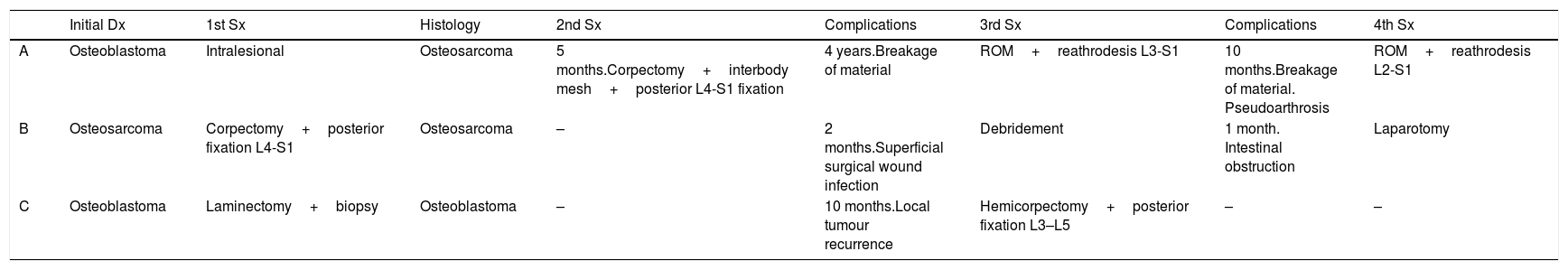
List of surgeries that the 3 cases underwent.
| Initial Dx | 1st Sx | Histology | 2nd Sx | Complications | 3rd Sx | Complications | 4th Sx | |
|---|---|---|---|---|---|---|---|---|
| A | Osteoblastoma | Intralesional | Osteosarcoma | 5 months.Corpectomy+interbody mesh+posterior L4-S1 fixation | 4 years.Breakage of material | ROM+reathrodesis L3-S1 | 10 months.Breakage of material. Pseudoarthrosis | ROM+reathrodesis L2-S1 |
| B | Osteosarcoma | Corpectomy+posterior fixation L4-S1 | Osteosarcoma | – | 2 months.Superficial surgical wound infection | Debridement | 1 month. Intestinal obstruction | Laparotomy |
| C | Osteoblastoma | Laminectomy+biopsy | Osteoblastoma | – | 10 months.Local tumour recurrence | Hemicorpectomy+posterior fixation L3–L5 | – | – |
Dx: diagnosis; ROM: removal of osteosynthesis material; Sx: surgery.
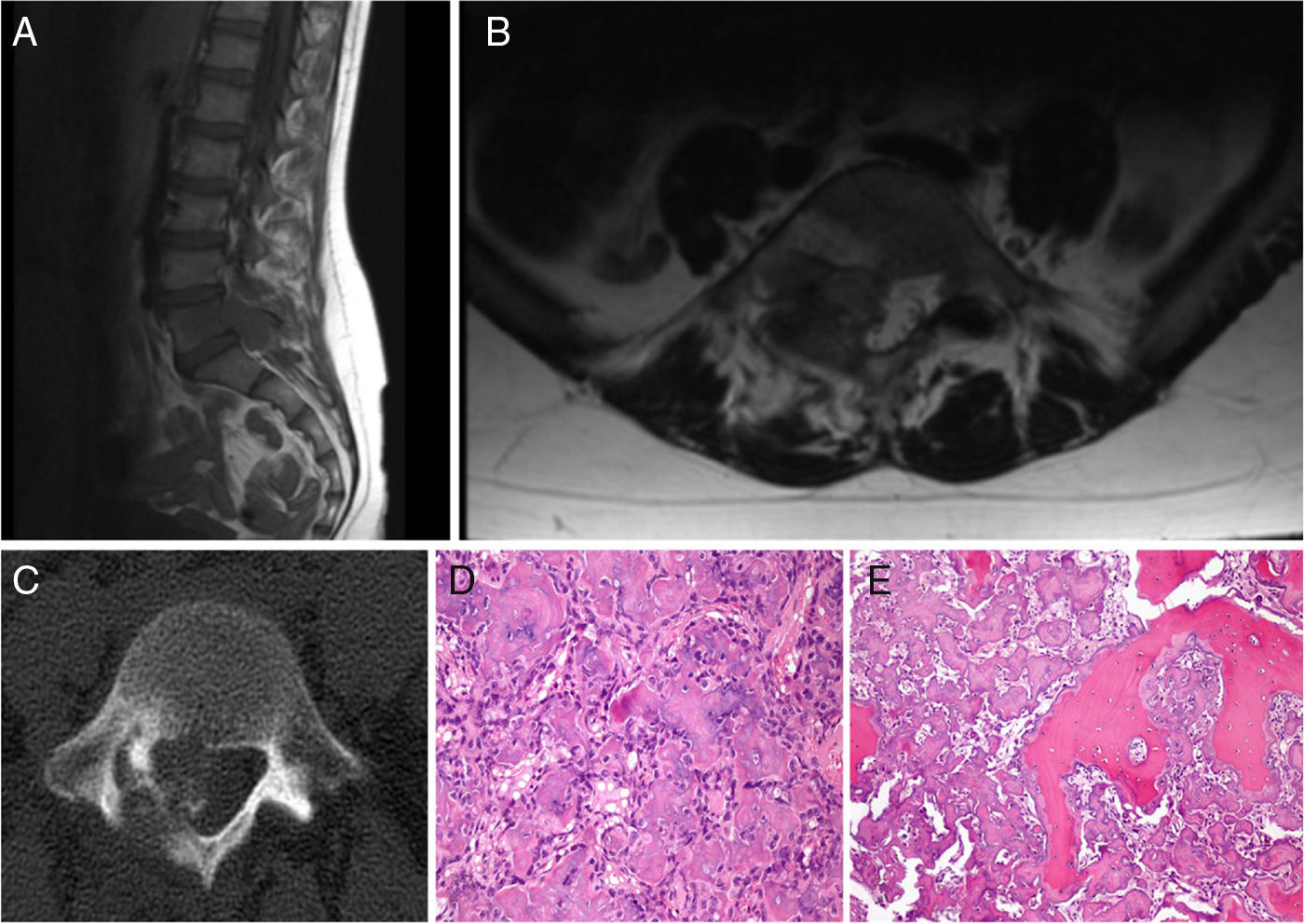
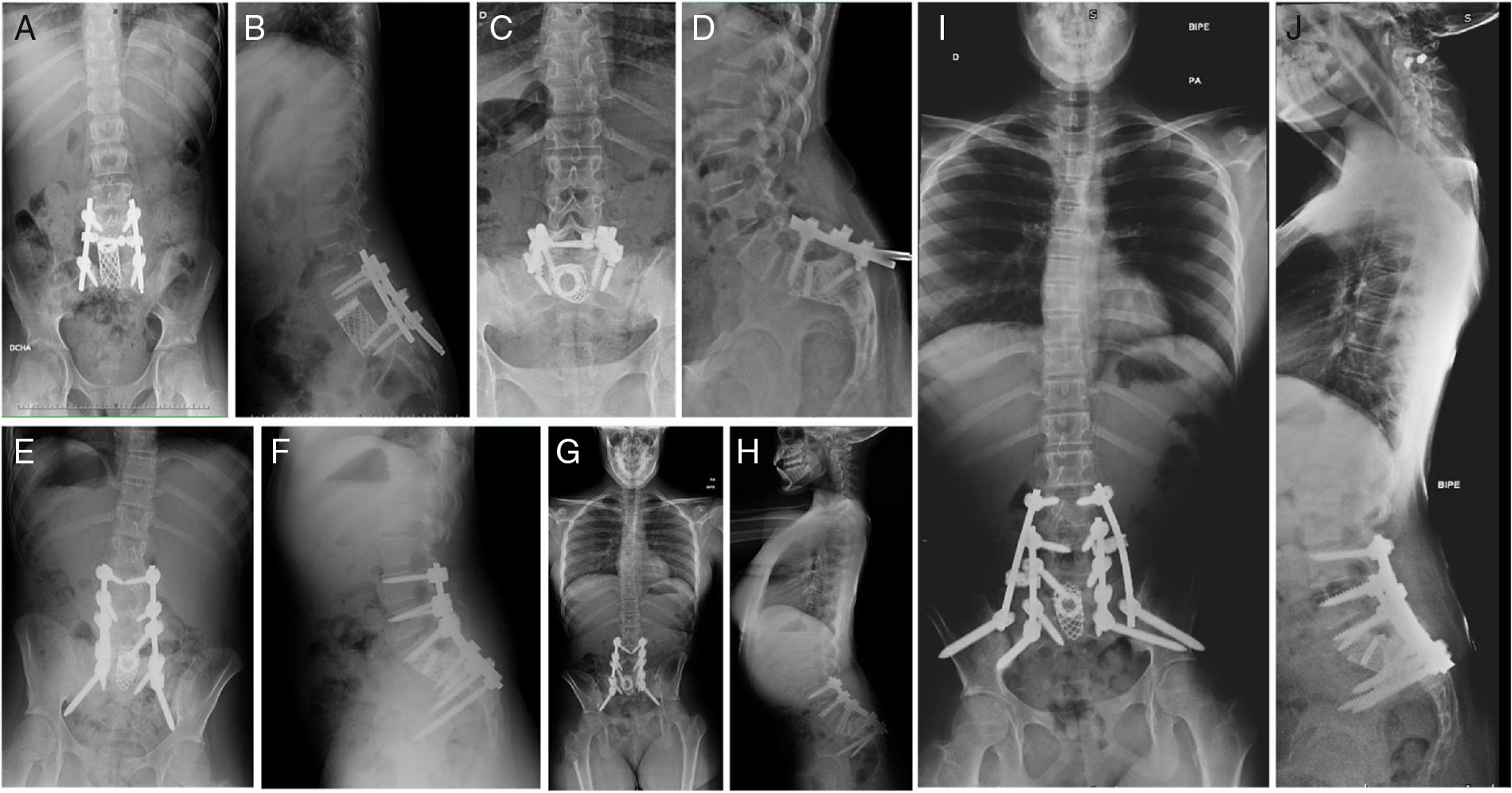
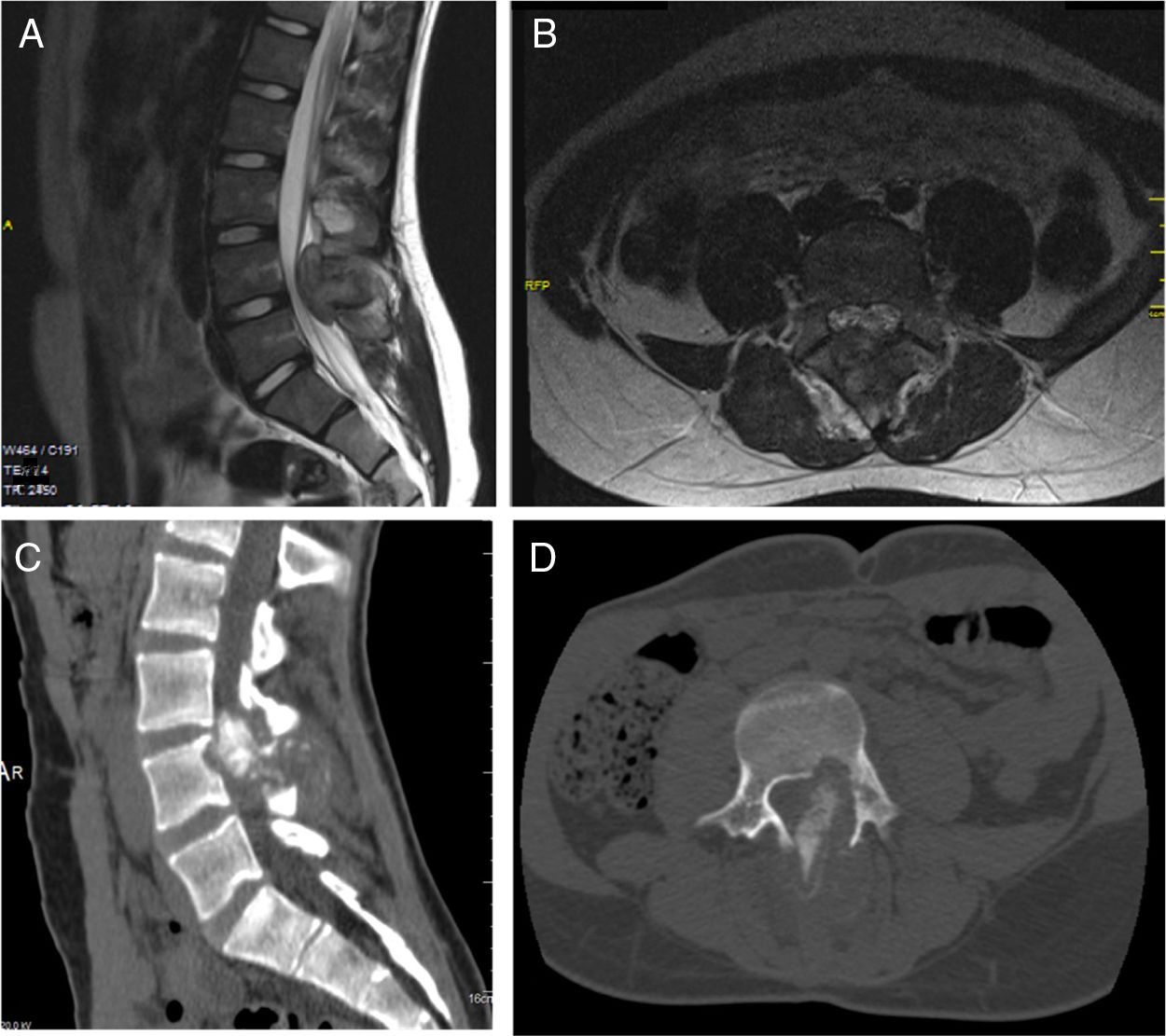
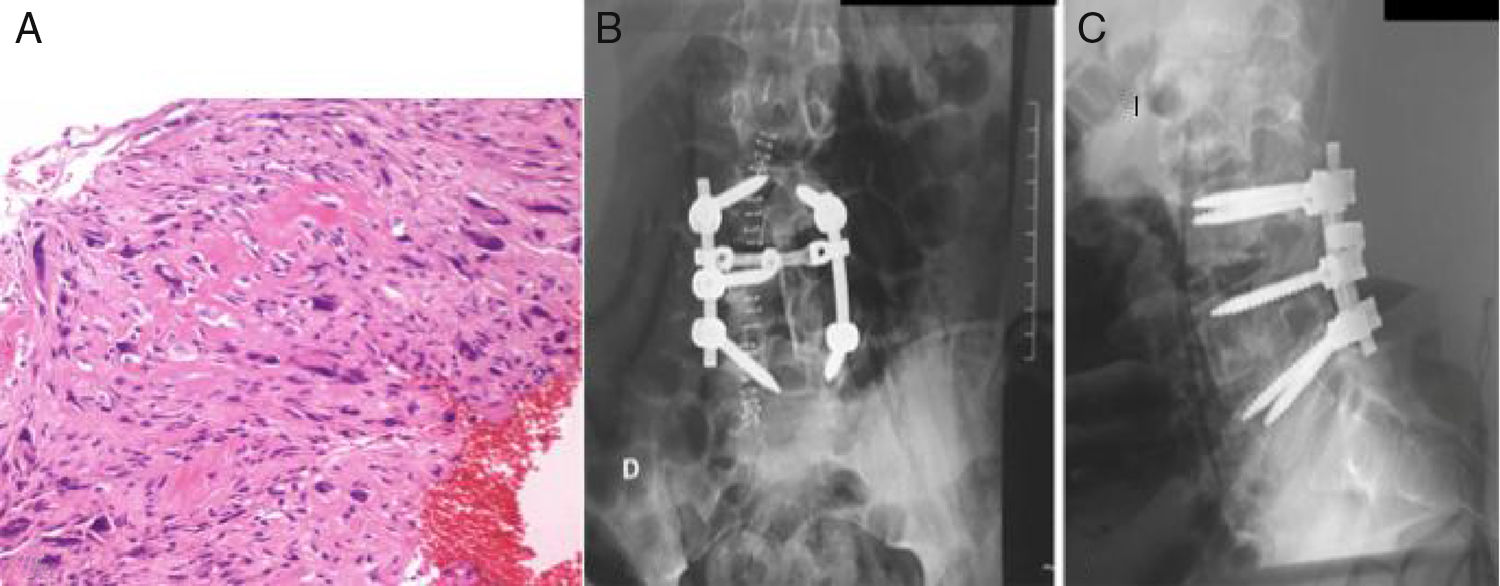
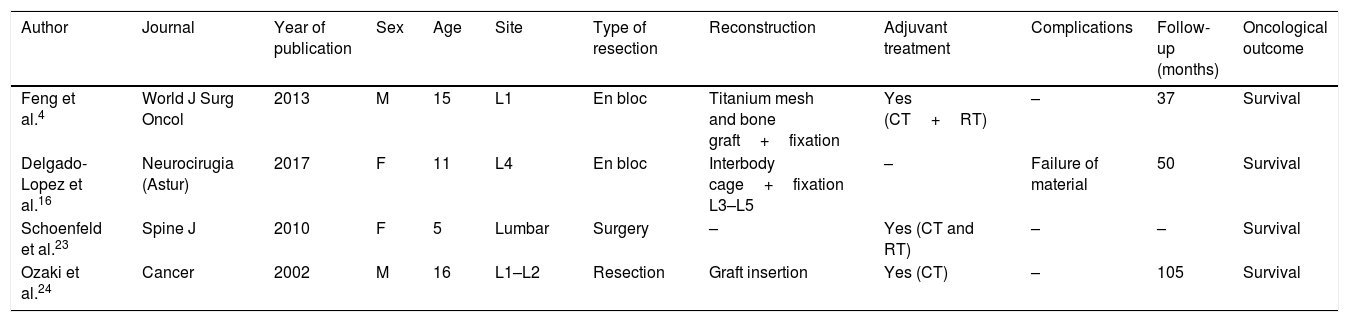
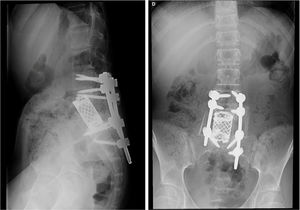
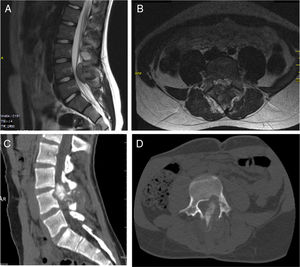
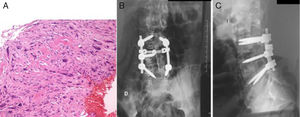
Patient A, aged 9 years+10 months at time of diagnosis (Fig. 1) initially consulted with lumbar pain radiating to the lower right limb. A CT scan and MRI were performed that showed a most probable diagnosis of osteoblastoma located in the right lamina of L5, breaking the cortical bone, invading the spinal canal and displacing the thecal sac, which was subsequently confirmed by biopsy. This is why the neoadjuvant protocol that we use routinely in our hospital was not used, and neither was an en bloc resection initially planned; instead we performed a first operation with an intralesional resection (removal of tumour+L5 laminectomy). After analysing the intraoperative sample the tumour was confirmed as an osteosarcoma classified as Enneking IIB, WBB BCDE zones 9–12, and type 4 according to Tomita's classification, and histopathogically classified as a Broders II. Chemotherapy treatment was started (protocol of the Spanish Society of Paediatric Haematology and Oncology [SEHOP-SO-2010],17 starting treatment with ifosfamide and adriamycin, then later methotrexate, cisplatin and adriamycin) a second operation was scheduled to widen the margins and for reconstruction. During the second operation the patient suffered hypovolaemic shock which meant that only a partial resection of the L5 vertebral body and L4-S1 arthrodesis were performed with a posterior approach; it was completed 6 days later, using a posterior approach, L5 corpectomy and reconstruction with interbody mesh with allograft were performed. The treatment was completed according to the SEHOP-SO-2010 protocol with postoperative chemotherapy (ifosfamide, adriamycin, methotrexate, cisplatin and immunotherapy with mifamurtide) and concomitant radiotherapy. Nine months after the surgery, a chest CT and control MRI of the spine were performed discounting recurrence and lung metastases. Four years following the first surgery, the patient required further surgery due to failure of the osteosynthesis material (breakage of sacral screws) not having achieved fusion in the lumbosacral area, the material was removed and the level of arthrodesis was extended to L2, at 10 months after this operation the osteosynthesis material (rods) broke due to the persistence of pseudoarthrosis and therefore the instrumentation was extended to the iliac bones with a four-rod system (Fig. 2). Both failures were studied by plain X-ray and CT. The patient sustained a superficial surgical wound infection which was resolved with local debridement and treatment with amoxicillin/clavulanic acid. On follow-up the patient had no recurrence but mild neuropathic symptoms persisted in the lower right limb, which were the reason for the initial consultation.
Patient A. (A, B) Preoperative MRI. Tomita IV. Enneking IIB. WBB BCDE 9–12. (C) Preoperative CAT scan showing invasion of the canal displacement of the thecal sac. (D) First biopsy, showing bone tumour comprising anastomosing osteoid trabeculae rimmed by osteoblasts, which occasionally show an epithelioid appearance, with large vesicular nucleus and prominent nucleoli, compatible with osteoblastoma. (E) Second biopsy with areas of abundant lace-like osteoid formation, arranged around cells with atypia, pleomorphism and frequent mitotic figures, some atypical. In the areas of transition between the host bone and the neoplasm, there is permeation, normal bone trabeculae have become trapped, which is an indisputable sign of malignancy.
Patient A. (A, B) Resection of L5 vertebral body. Interbody mesh. Posterior fixation L4-S1. (C, D) Failure of material. (E, F) Extension of instrumentation from L2 to S2. (G, H) Failure of material. (I, J) Definitive postoperative outcome. Extension of instrumentation from L2 to iliac bones.
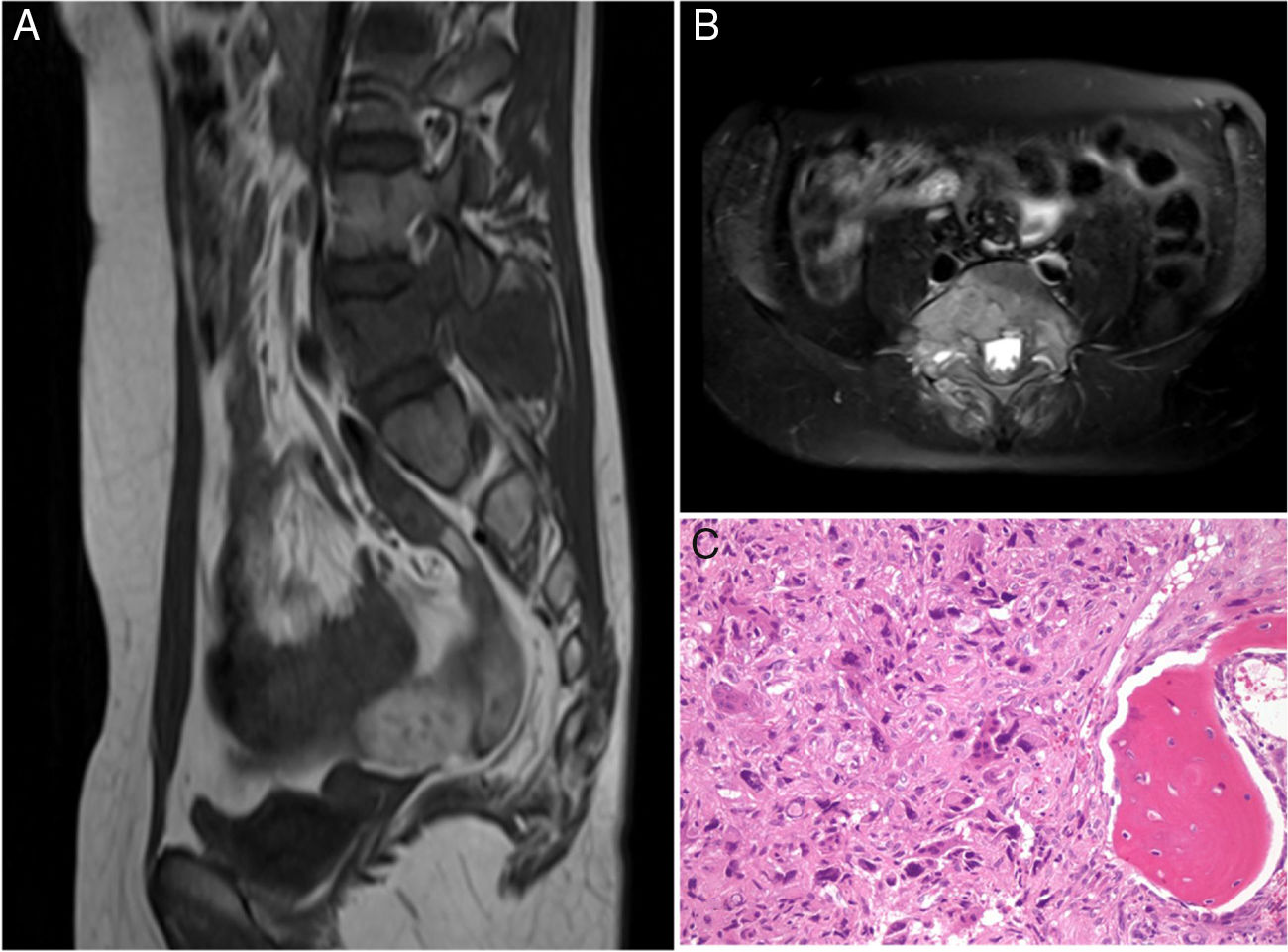
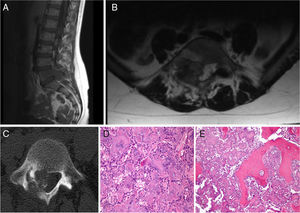
Patient B was 11 years old at the time of diagnosis. The initial clinical symptoms were a 5-month history of lumbar pain which did not respond to analgesics, radiating to both lower limbs and accompanied by asthenia and anorexia. An MRI was performed which revealed a tumour of aggressive characteristics in the posterior elements of L5 (Fig. 3), a CT-guided biopsy was performed and osteosarcoma of L5 vertebra was diagnosed. The chest CT showed no metastatic lesions on diagnosis. The tumour was classified according to the Enneking system as stage IIB, according to the WBB classification ABCD zones 8–3, and type 5 according to the Tomita classification. Histopathologically it was a Broders II. Prior to surgery the interventional radiology department performed selective embolisation. The preoperative chemotherapy protocol was started (according to the SEHOP-SO-2010 protocol17 with ifosfamide, adriamycin, than later methotrexate, cisplatin), in a first stage removal of the posterior arch of L5 and L3-S2 arthrodesis were performed using a posterior approach after failing to resect the vertebral body using the Tomita technique. In a second stage 7 days later, an L5 corpectomy was performed using a posterior approach and reconstruction with interbody mesh filled with allograft, and compression of the L4-S1 space using a posterior approach (Fig. 4). It was decided to complete the local control of the disease with external radiotherapy because, due to the location of the primary tumour, it is not possible to perform an en bloc resection of the tumour and ensure free margins and continue treatment with postoperative chemotherapy according to the SEHOP-SO-2010 protocol. A control MRI was performed one month after the surgery, and radiological controls of the spine every three months for one year following the intervention then continuing with annual radiological controls and complementary oncological tests for follow-up. The patient suffered surgical wound dehiscence two months after the surgery, which was treated by debridement without requiring the material to be removed, and was later reoperated due to an intestinal obstruction that resolved without incident.
Patient B. (A, B) Preoperative MRI. Tomita V. Enneking IIB. WBB ABCD 8–3. (C) Areas of chondral differentiation with chondral nidi with binucleations and cytological atypia and densely cellular that alternate with host bone tissue and other areas showing bone trabeculae of reactive appearance. There are a large proportion of the cylinders that no longer show bone trabeculae, which have now disappeared destroyed by the atypical cellular proliferation in addition to the presence of osteoid, mitoses, some of which are atypical, and obvious pleomorphism. Compatible with osteosarcoma.
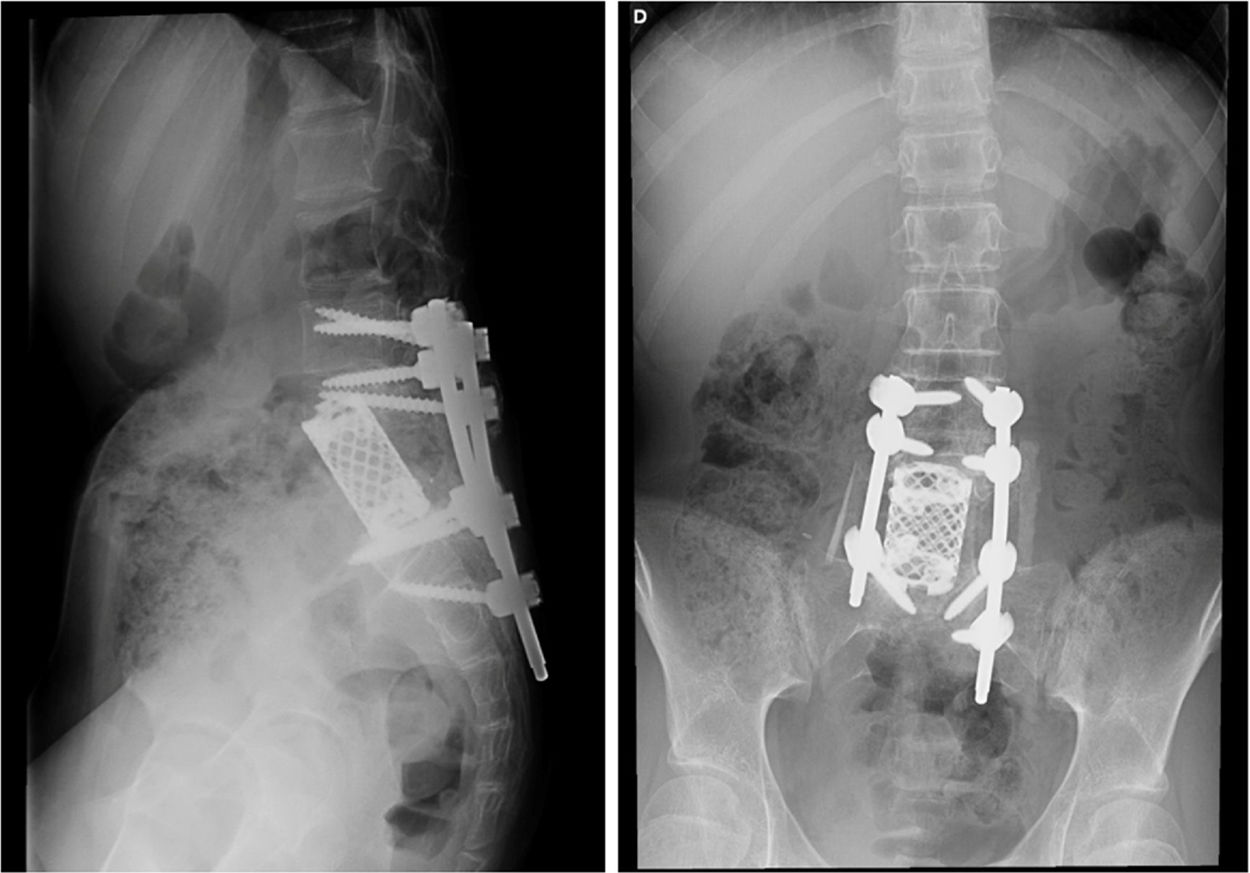
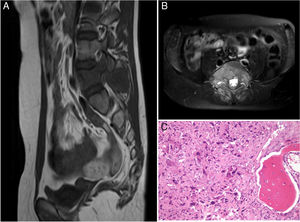
Patient C was 15 years old at the time of diagnosis. The initial clinical symptoms were a 6-month history of lumbar pain, MRI revealed a mass in the spinous process of L4 protruding into the medullary canal, suggestive of osteoblastoma (Fig. 5). A decompressive laminectomy was performed combined with a diagnostic biopsy; anatomical pathology confirmed the initial diagnosis of osteoblastoma. The patient made significant clinical improvement. One year after surgery he was referred to our centre with lumbar pain, and an MRI, CT and bone scan were performed. Because there was suspected recurrence of the tumour, a new biopsy was performed, which confirmed recurrence of the osteoblastoma. Due to the local aggressiveness of the lesion it was decided to perform L3–L5 fixation and L4 hemicorpectomy using a posterior approach, after marginal dissection separating the soft tissue mass posterior to the dural sac until locating the outlet of the L4 and L5 nerve roots. A wide margin resection was performed of the lateral part of the L4 vertebral body until reaching the anterior face of the vertebral body, and placing a malleable valve. Once the lateral face of the L4 body had been dissected and the posterior soft tissue mass had been separated the dural sac was separated medially, at this stage it was necessary to perform a complete intralesional resection around the L5 nerve root, in order to save it. A cut was made in the upper and lower disc, and subsequently a longitudinal and oblique osteotomy from posterior to anterior and towards the right to obtain more margin of the vertebral body. Once the surgical specimen had been released a turn was made laterally, extracting the hemibody, performing a complete intralesional resection, with posterior reconstruction using a tricortical iliac crest allograft in the anterior defect, and performing an L3–L5 fusion (Fig. 6). Anatomical pathology of the extracted sample was diagnostic of vertebral osteosarcoma in L4, Broders II, Enneking IIB, WBB ABCDE 11–5 and Tomita type 4. After the new findings, the patient was given adjuvant chemotherapy as well as local radiotherapy; the appropriate controls were performed with plain X-ray of the operated area as well as the oncological follow-up protocol. The patient improved significantly from the initial lumbar pain symptoms and currently remains free from disease.
None of the patients had local recurrence after the treatment by complete surgical resection (patient A and B vertebrectomy, patient C hemivertebrectomy), or distant metastases during follow-up of 72.8, 50.2 and 64.6 months respectively.
DiscussionEn bloc resection of a malignant tumour is the gold standard technique. Due to the special characteristics of the spinal anatomy, this en bloc resection is sometimes difficult to achieve, but the principles are constant. The nerve elements must be protected and released as far as is possible. The tumour will be resected from a healthy margin of tissue, performing a circumferential dissection. Various implants can be used for reconstruction.11 In the cervical and lumbar regions a dual approach will usually be necessary (anterior and posterior) to minimise the risk of nerve damage on removing the tumour, and to reconstruct the anterior spine.11 When a single posterior approach is used this is termed the Tomita technique.17
The technique for performing a vertebrectomy consists of sectioning both pedicles to separate the posterior arch from the rest of the vertebra. Afterwards, both fragments can be removed separately by a series of delicate gestures that require careful releasing of the nerve and vascular elements. Compared to intralesional piecemeal resection, this technique reduces the risk of local recurrence.17 This procedure is considered effective for patients with spinal tumours with no spread, for whom the vertebrectomy is expected to improve function and survival. However, it is not free from neurovascular morbidity due to its technical difficulty.17 A systematic review by the Spine Oncology Study Group concluded that the grade of recommendation for performing VTB is strong, bearing in mind that the adverse event profile is high even in experienced centres,18 and there is also a high risk of vascular and spinal damage, with increased instability of the spinal column.19 En bloc resection has been seen to improve local control of the disease, and it is believed that it would probably improve overall survival,20 however this has not yet been demonstrated. In this paper we describe three cases that underwent a complete resection, and remain free from local and systemic disease.
In the study published by Boriani et al. in 2010 on the mortality of en bloc vertebrectomy,21 35.1% of the patients had complications. Of the 70 complications recorded in total of the 134 patients in the sample, 41 were major complications (injury to the vena cava, aorta, renal failure, pulmonary embolism, deep infection and paraplegia), and 3 patients died as a result of these complications. Of the 3 cases we describe in this study, the major complication was an intraoperative hipovolaemic shock, the minor complications were 2 failures of the osteosynthesis material, in the same patient, and 2 superficial surgical wound complications. These data coincide with the high morbidity of these procedures, although in 2 of the cases (patient B and C) there were no major or neurological complications.17 There was no death in this series, although in articles such as that of Boriani21 there were, the patients we describe were free from local and systemic disease after 50 months of follow-up. One operation with complete resection reduces the risk of recurrence20 although the potential complications18,21 of this type of surgery must be borne in mind, as confirmed in the study.
The osteoblastoma-like osteosarcoma subtype accounts for 1.1% of all osteosarcomas.8 Histologically OBLOS show permeative and immature surrounding bone tissue, whereas with osteoblastoma it is mature and circumscribed.9 The presence of cellular atypia, nuclear atypia, abnormal mitosis and a permeative pattern are suggestive of osteosarcoma.20 The correct identification and management of aggressive osteoblastoma, OBLOS and borderline osteoblastoma remain a challenge as cases A and C show, who were initially diagnosed with osteoblastoma. Patient C was diagnosed with a malignant transformation of osteoblastoma to osteosarcoma, which is an entity widely described in the literature, although some authors believe that malignant transformation of osteoblastoma could be an undiagnosed OBLOS.22 The initial diagnostic error made subsequent surgeries necessary in both cases, increasing the risk of recurrence and the probability of complications, as serious as hypovolaemic shock in case A.
Research continues for markers to help us correctly identify these entities. In a recent study published with 54 patients,23 it seems that analysis of the distribution of nuclear β-catenin is a useful marker for the identification of osteoblastoma vs osteosarcoma. In OB this is found accumulated in the nucleus, whereas in OS we find it in the cytoplasm or in the membrane. However, β-catenin has also been found in some chondroblastic cells of OS, therefore the anatomopathologist must consider this parameter along with the other anatomopathological, radiological and clinical markers, and not consider it a unique identifying marker.
Treatment with neoadjuvant chemotherapy helps to reduce the tumour size improving surgical outcomes. In this study only one patient underwent neoadjuvant chemotherapy, and all the patients were treated with postoperative chemotherapy and radiotherapy. Although OS could be considered refractory to radiotherapy, according to the literature this could be useful in the small cell subtype, in patients who are not candidates for surgery and those who have undergone subtotal tumour resection.
Schoenfield et al. published the results of 26 patients (mean age 46 years) with osteosarcoma of the mobile spine treated with surgery, chemotherapy and radiotherapy with a mean survival of 29 months.24 The objective of the study was to evaluate the results comparing en bloc resection with positive margins vs negative margins. They concluded that whenever possible an en bloc resection with free margins should be performed, in order to do this it is important that the vertebra has at least one healthy pedicle that enables dissection to be performed.5 The current trend to use more aggressive therapies has improved survival which is now between 18% and 45%.20 Although the study with 20 patients published by Zils et al., obtained 60% at 5 years, and 53% at 10 years.
Table 3 lists the cases of lumbar vertebral osteosarcoma in children under 18 years of age collected in the articles from the literature review. Comparing the sex and age of the patients on diagnosis, tumour site, type of surgery performed, adjuvant treatment and oncological outcome, provided it was shown in the article. A total of 4 cases are presented for whom different resection techniques were performed with subsequent oncological treatment, which confirms the complex management of this disease.
Lumbar osteosarcomas in the paediatric age group described in the literature.
| Author | Journal | Year of publication | Sex | Age | Site | Type of resection | Reconstruction | Adjuvant treatment | Complications | Follow-up (months) | Oncological outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Feng et al.4 | World J Surg Oncol | 2013 | M | 15 | L1 | En bloc | Titanium mesh and bone graft+fixation | Yes (CT+RT) | – | 37 | Survival |
| Delgado-Lopez et al.16 | Neurocirugia (Astur) | 2017 | F | 11 | L4 | En bloc | Interbody cage+fixation L3–L5 | – | Failure of material | 50 | Survival |
| Schoenfeld et al.23 | Spine J | 2010 | F | 5 | Lumbar | Surgery | – | Yes (CT and RT) | – | – | Survival |
| Ozaki et al.24 | Cancer | 2002 | M | 16 | L1–L2 | Resection | Graft insertion | Yes (CT) | – | 105 | Survival |
The major limitation of this article is the small case load, although this is not surprising if the low frequency of this neoplasm in the paediatric age group is taken into account. All the patients were treated in the same centre; therefore, the sample could have been increased in a multicentre study. The descriptive nature of this study is another limitation.
We found few reported cases on osteosarcoma of the spine in the paediatric age group and how they were managed.4,17,24,25
ConclusionsVertebral osteosarcoma is a rare lesion, even more so in the paediatric age group, only four cases in the spine are described in the literature. There is high mortality in the series and high surgical morbidity, although in children this can be improved by adjuvant treatment. The survival in our study was longer than 50 months.
It is essential to differentiate entities with outcomes and treatment as different as those of osteoblastoma, osteoblast-like osteosarcoma and osteosarcoma. Correct diagnosis and staging of the lesions will enable precise treatment, and improve the possibilities of a cure.
Intra and postoperative complications are frequent, even in expert hands, therefore surgery has to be planned beforehand to minimise these as far as is possible.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Egea-Gámez RM, Ponz-Lueza V, Cendrero-Torrado A, Martínez-González C, Certucha-Barragán JA, González-Díaz R. Osteosarcoma lumbar en edad pediátrica: reporte de casos y revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2019;63:122–131.