Pseudoarthrosis is a complication that occurs in up to 12% of astragalus fractures. In this situation, 2 main treatment options are considered: arthrodesis and secondary reconstruction. In this text we present the case of a patient who suffered this complication after not being diagnosed with the fracture he suffered and opted for secondary reconstruction with good results.
Fracture nonunion affects up to 12% of patients suffering a talar fracture. Classically, most authors proceed to joint arthrodesis when facing such complication. A more recent approach consists on secondary reconstruction of the nonunion. In this paper we present the case of a reconstructed talar nonunion after an unnoticed talar body fracture with encouraging results.
La seudoartrosis es una complicación que se presenta en hasta un 12% de las fracturas del astrágalo. Ante esta situación se plantean 2opciones de tratamiento principales, la artrodesis y la reconstrucción secundaria. En este texto presentamos el caso de un paciente que sufrió dicha complicación tras no diagnosticarse la fractura que presentaba y se optó por la reconstrucción secundaria, con buenos resultados.
Talar fractures comprise 3% of tarsal fractures, the second most frequent in this location after calcaneal fractures.1
Characteristically, they occur after high-energy impact (traffic accidents, falls, etc.) and are usually not detected in an acute situation, which reflects the diagnostic challenge they pose.
The most frequent complications after talar fractures are post-traumatic osteoarthritis and avascular necrosis (AVN), the latter being closely related to the initial displacement of fragments.2 According to published series, pseudoarthrosis occurs in up to 12% of cases.3 We present the case of a patient who presented with this complication.
Clinical caseOur case is a 40-year-old patient, with a history of personality disorder and consumption of multiple toxic substances, who suffered a fall from 9m under the effect of alcohol and amphetamines. On arrival at our emergency department as a polytrauma patient, he was diagnosed with multiple fractures (right ulnar diaphysis, left distal radius, pelvic branches, orbit and multiple ribs). At the time of the initial assessment, no impairments were seen, and the patient did not report any alterations to the foot or ankle.
Two weeks after admission, the patient reported pain in his right ankle, and antero-posterior and lateral X-rays were taken (Fig. 1Fig. 1A and B), but no fracture lines were detected. The patient was treated as having an ankle sprain and conservative treatment was given with rest, analgesia and cryotherapy.
(A and B) X-rays on admission for polytrauma. No fractures were found. (C and D) CT scan requested in outpatient clinics. Complete of the astragalus body associated with osteochondral fractures and free bone fragments; no bone bridges seen. (E and F) Postoperative control X-rays. (G and H) Control CT scan at 2 months. Evidence of bone bridges.
In successive check-ups, and in view of the persistent discomfort at this level, the patient was referred to our Foot and Ankle Unit.
On the first visit to our unit, 14 months after the polytrauma, the patient attended non-weight bearing with crutches due to pain. A study was carried out with radiography and tomography (Fig. 1C and D) in which a complete fracture of the astragalus body was visualised, associated with osteochondral fractures and free bone fragments, with no evidence of bone bridges. The study was completed with an MRI that did not show AVN. Given this situation, the patient was diagnosed with pseudoarthrosis of the astragalus body.
In our case, considering the available literature and the characteristics of the patient, it was jointly decided to perform a secondary reconstruction of the pseudoarthrosis.3–8
To perform this reconstruction, 2 approaches were used: anterolateral and anteromedial. Once the fracture site had been located, the pseudoarthrosis tissue was abraded and excised. The bone defect was then corrected with an autograft of the iliac crest. Once the correct alignment of the fragments through both approaches was verified, internal fixation of the reconstruction was performed with 2 cannulated titanium screws 4mm in diameter with incomplete thread (manufactured by AAP®, Berlin, Germany; distributed by MBA®, Gijon, Asturias, Spain) from the anterolateral approach and a 4mm cannulated screw of the same characteristics from the anteromedial approach.
ResultsDuring the postoperative period, the limb was kept immobilised with a plaster cast. No incidents were detected on the postoperative control X-rays (Fig. 1E and F). Since the surgical wounds progressed without incident, when the suture was removed the plaster splint was replaced by a walking boot, although the limb was kept non-weight bearing.
Two months following the intervention a control scan was performed that showed the presence of bone bridges (Fig. 1G and H). During this time, the patient started partial weight-bearing on that limb.
At 4 months, the walking boot was removed, and the patient began sports activity (swimming), and full weight bearing was allowed.
In successive controls, no crutches were required, and the pain reported was 2/10 on the visual analogue scale. At the last control, 18 months after the surgery, the patient presented complete plantar flexion with a deficit of 10 dorsiflexion, with no limitations in subtalar mobility.
DiscussionPseudoarthrosis of the astragalus poses a challenge in terms of treatment given the relatively low prevalence of this condition and the lack of studies that consistently support different therapeutic approaches. The main options in this situation are arthrodesis (the classical approach) and secondary reconstruction (the more current and promising approach).4–6,8
Arthrodesis targets pseudoarthrosis-affected or painful joints. Secondary reconstruction, on the other hand, requires abrasion of the pseudoarthrosis site, placement of allograft or autograft and internal fixation. In certain locations (lateral and posterior processes), exeresis without secondary reconstruction is preferred.7
The literature stresses the importance of considering the general factors (comorbidities, bone quality, adherence to treatment, etc.) and local factors (AVN, osteoarthritis, infection, state of the articular cartilage, etc.) of the patient to decide the best therapeutic option.5
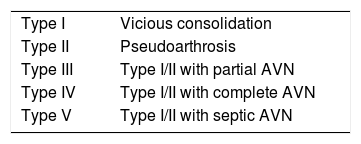
Zwipp and Rammelt made their classification taking only local factors into account, which differentiates 5 types of pseudoarthrosis and vicious consolidation (Table 1).5 In type I–III patients, without significant local involvement, reconstruction could be considered provided the patient does not present clinical osteoarthritis or comorbidities that would compromise the final result (poorly controlled diabetes, peripheral vascular disease at stage ≥IIb, severe immunodeficiency or osteoporosis), has a relevant degree of functional demand and is committed to treatment. In patients with type IV–V or who do not meet the criteria for reconstruction despite being type I–III, arthrodesis is recommended. Following these guidelines, these authors report high consolidation rates without onset or progression of AVN. In their review of 10 cases with an average follow-up of 4 years, all the patients were satisfied with the outcome of the surgery, reporting a mean AOFAS Ankle Hindfoot Score of 86. The only exception was a patient who was arthrodesed 8 years after the procedure.8
Classification of post-traumatic deformities of the astragalus.
| Type I | Vicious consolidation |
| Type II | Pseudoarthrosis |
| Type III | Type I/II with partial AVN |
| Type IV | Type I/II with complete AVN |
| Type V | Type I/II with septic AVN |
Partial AVN: AVN that affects less than one-third of the body of the astragalus; AVN: avascular necrosis.
Source: Zwipp and Rammelt.5
In our case, the result after secondary reconstruction of pseudoarthrosis of the astragalus body in a type II patient was satisfactory. This result is along the lines of the latest case series that advocate secondary reconstruction as a valid option, before arthrodesis, in a given segment of patients. Even so, more extensive studies with longer follow-ups are needed to understand in detail the long-term implications of this approach.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Corró S, Duarri G, Busquets R. Reconstrucción secundaria de seudoartrosis del cuerpo del astrágalo tras fractura no diagnosticada. Rev Esp Cir Ortop Traumatol. 2020;64:223–226.