To determine the factors that affect functional recovery after a hip fracture.
MethodsA study was conducted on a cohort of 333 patients aged 65 years or over with hip fractures who were admitted to Carlos Haya hospital between February 2004 and February 2005. Epidemiological, clinical and functional activity data were recorded by applying generally used scales to determine the patients’ functionality before and after the fracture, by means of telephone interviews 6 months after the fracture.
ResultsPrognostic factors of functional incapacity 6 months after the fracture were age, being institutionalized, having poor functionality before the fracture, being dependent for basic activities of daily living and having had an extracapsular fracture or undergoing osteosynthesis.
ConclusionsIt is possible to determine the prognosis of a hip fracture patient on admission. The use of extramedullary fixation systems failed to show good results compared with arthroplasty. Intramedullary osteosynthesis (used only in 5 patients), and an early start of rehabilitation could improve the functional results of these patients. In fact, intramedullary nailing has demonstrated better outcomes in unstable trochanteric and sub-trochanteric femoral fractures versus Dynamic Screw and Plate.
Conocer los factores que determinan la recuperación funcional tras haber sufrido una fractura de cadera.
MétodoSe ha realizado un estudio de cohortes sobre 333 fracturas de cadera en pacientes mayores de 65 años, que ingresaron en el Hospital Regional Universitario Carlos Haya entre febrero de 2004 y febrero de 2005. Hemos recogido datos epidemiológicos, clínicos y de actividad funcional de dichos pacientes mediante la aplicación de escalas de uso generalizado, para conocer la funcionalidad que presentan antes de la fractura y en el seguimiento posterior, mediante entrevistas telefónicas a los 6 meses tras la misma.
ResultadosA los 6 meses de la fractura los factores pronósticos de incapacidad funcional son la edad, el hecho de estar institucionalizado, presentar una mala funcionalidad previa a la fractura, ser dependiente para las actividades básicas de la vida diaria y la circunstancia de haber presentado una fractura extracapsular o que haya sido sometida a osteosíntesis.
ConclusionesPodemos conocer el pronóstico del paciente con fractura de cadera al ingreso, el uso de sistemas de fijación extramedular no ha mostrado buenos resultados en nuestro trabajo frente a la artroplastia. La osteosíntesis intramedular (usada únicamente en 5 casos) junto a un inicio precoz de la rehabilitación podrían mejorar los resultados funcionales de estos pacientes, ya que ha demostrado ser superior en las fracturas pertrocantéreas inestables y en las subtrocantéreas.
Hip fracture is prevalent among the elderly population, occurring in more than 85% of times in persons over 65 years of age. It has been estimated that, in 1990, there were 1.26 million hip fractures throughout the world, a figure that is expected to reach 4.5 million in 2050.1 The annual incidence of hip fractures in United States is currently 250,000 and this figure is forecast to double by 2050.2 In Spain, about three million patients suffer from osteoporosis and, in view of the ageing of the current population, this number is expected to increase along with the number of associated fractures. The AFOE study (Memorandum on Osteoporotic Fracture in Spain) conducted by the GEIOS group in 2003 gave confirmation that the incidence of osteoporotic fractures in Spain was much greater than had been thought: versus the 33,000–40,000 hip fractures per annum in the population over 60 years of age reflected in the literature, there were actually 60,000, in other words 720 cases every year for every 100,000 people over the age of 60.3,4
Although there are several doctoral theses on the subject of hip fractures, most of them focus on such aspects as their morbi-mortality,5,6 the associated nutritional factors7,8 or even more extensive aspects covering incidence, risk factors, treatment, the functional consequences and the mortality of this kind of fracture.9 However, in our setting there are fewer studies of this type focusing on the factors constraining the functional capacity of elderly patients after suffering a fracture of this type.10
The idea behind this paper has been to describe the factors determining the functional prognosis of these patients, posed with a view to verifying our functional outcomes in this kind of fracture and understanding those factors on which we can act to improve these results and, in this way, to propose measures of a clinical nature affecting the treatment of this health problem so frequent nowadays.
These fractures often occur in patients with other health problems, osteoporotic and in permanent decubitus position, generally requiring multidisciplinary treatment. Furthermore, it is necessary to plan from the outset for intensive rehabilitation intended to achieve their return to social life as quickly as possible.
Material and methodsA total of 333 patients aged 65 years or more, admitted to and treated at the Orthopaedic and Traumatology Department were studied at “Carlos Haya” Regional University Hospital in Málaga (Spain) from February 2004 to February 2005, because they presented a low-energy fracture of the proximal third of the femur. It was a prospective monitoring study with a pre-formed questionnaire to collect all the variables and scales evaluating their physical, mental and functional status, pain and social support. Patients were excluded if they had isolated fractures of the trochanter majoris and fractures of the head of the femur (Pipkin type), or if they had suffered multiple trauma or multiple serious fractures. The follow-up continued throughout their hospital stay and subsequent to discharge by means of telephone interviews with the patients, their relatives or carers, 6 months after the fracture.
Type of fracture: These were classified as sub-capital, basicervical, pertrochanteric and sub-trochanteric. The first of these was considered to be intracapsular and others extracapsular.
Prior pathology: The ASA scale allows us to know the general status of the patient prior to surgery. Although it is divided into 5 sections, since number V is only applicable in extreme cases (no patient in our study), we regrouped the remaining 4 into 2 categories: 1 or 2 and 3 or 411 for the purpose of statistical analysis of the functional capacity.
Social support scales: The social support scale has been divided into 3 categories:
- -
Person living alone in own home: when they lived without any company and have to deal with their personal needs by themselves.
- -
Person living at home with relatives: this group includes those patients living with a spouse and/or their children in either their own home or else with relatives at a home belonging to someone else.
- -
Living in a publicly- or privately funded institution: patients living with other people of the same age at a dedicated centre, whether belonging to the social services or private enterprise. We have also included patients living at psychiatric centres in this category.
Functional evaluation scale (Katz): This is divided into 6 items (washing, dressing, using the toilet, mobilization, continence and eating) with a score reflecting the degree of dependency as 0 (total dependency), 1 (moderate dependency) or 2 (independent). Therefore, 12 represents the maximum degree of independence and 0 absolute dependency for the activities of daily living.12
Mental evaluation scale (Pfeiffer): In order to understand the mental status of patients prior to and after the fracture, and the influence this has had on the recovery of their functional capacity.
Hip function and pain scale: This scale is fundamental to establish a comparison between the patient's status prior to the fracture and in the subsequent follow-up after 3 and 6 months. We have used the model devised by Martí-Valls and Alonso13 as it is simpler and easy to interpret. It has 3 items: pain, function and mobility-force. The possible scores on the scale range from 85 (no functional limitation in the hip) to 0 (maximum possible functional limitation). Based on personal information from the authors, by analogy with other hip scales, interventions can be considered to have achieved a good result if a score of 65 or higher is achieved (75% of the maximum possible) as the total score for the scale. This scale is completed by the physician based on information provided by the patient. This scale, together with the Katz scale, constitutes our main reference when it comes to identifying the functional status of our patients alive after 6 months, with functional impairment being understood as scores under 65 points.
Type of intervention: We are interested in knowing their functional recovery in the light of the type of fracture and intervention carried out. Treatment was classified into 2 large groups: arthroplasties (intracapsular) and osteosynthesis (extracapsular).
Data analysis has been done using SPSS 11.5 software (Statistical Packages for the Social Sciences).
A descriptive analysis has been made of all the variables (demographic, clinical, analytical details, medical, surgical and rehabilitation treatments, scores on the physical, social support, activities of daily life and functionality scales described). Continuous quantitative variables have been summarized with their mean, standard deviation, quartiles and ranges. Discrete qualitative or quantitative variables have been expressed in terms of their absolute and relative frequencies.
In order to identify any relationships existing in our cases between the various characteristics (demographic, clinical, social support, functionality, mental impairment), we have used the χ2 test in comparisons of 2 qualitative variables, Student's t-test or ANOVA to compare a quantitative variable in 2 or more groups. The functional, mental and social evolution from admission until 6 months later has been analyzed using ANOVA of repeated measures, and also the influence of age and gender on the results.
The prognostic factors for functional impairment at the end of the follow-up have been obtained by linear regression, considering the Katz scale score after 6 months as a quantitative variable, and by logistic regression with the hip function-pain scale, considering the score of 65 as the cut-off. In both cases, bivariant and multivariant analyses have been carried out. The level of significance has been set at p<0.05.
The multivariant analysis has considered all the independent variables that turned out to be significant in the bivariant analysis. The backward mode for automatic variable selection was used with the Wald statistic.
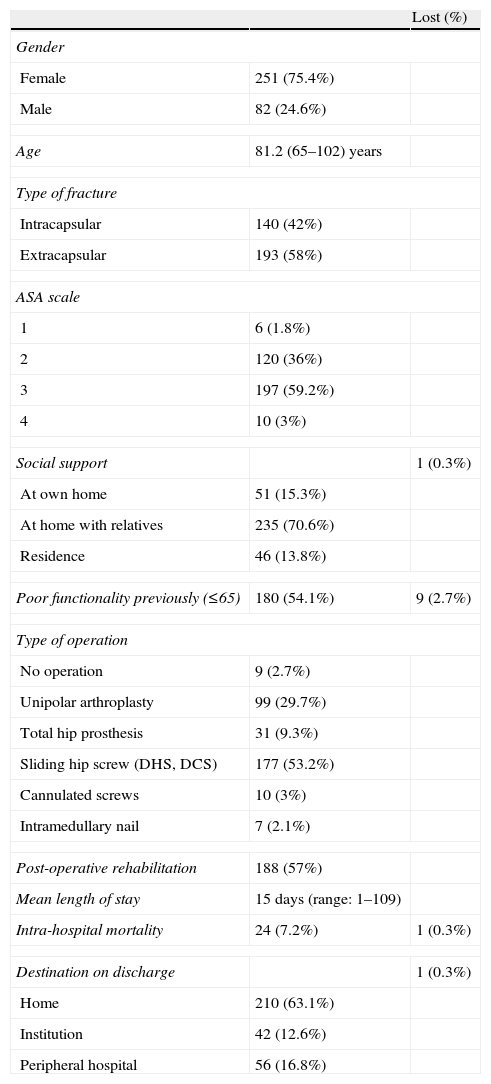
ResultsThe epidemiological characteristics of the population under study are shown in Table 1.
Characteristics of the sample (N=333).
| Lost (%) | ||
| Gender | ||
| Female | 251 (75.4%) | |
| Male | 82 (24.6%) | |
| Age | 81.2 (65–102) years | |
| Type of fracture | ||
| Intracapsular | 140 (42%) | |
| Extracapsular | 193 (58%) | |
| ASA scale | ||
| 1 | 6 (1.8%) | |
| 2 | 120 (36%) | |
| 3 | 197 (59.2%) | |
| 4 | 10 (3%) | |
| Social support | 1 (0.3%) | |
| At own home | 51 (15.3%) | |
| At home with relatives | 235 (70.6%) | |
| Residence | 46 (13.8%) | |
| Poor functionality previously (≤65) | 180 (54.1%) | 9 (2.7%) |
| Type of operation | ||
| No operation | 9 (2.7%) | |
| Unipolar arthroplasty | 99 (29.7%) | |
| Total hip prosthesis | 31 (9.3%) | |
| Sliding hip screw (DHS, DCS) | 177 (53.2%) | |
| Cannulated screws | 10 (3%) | |
| Intramedullary nail | 7 (2.1%) | |
| Post-operative rehabilitation | 188 (57%) | |
| Mean length of stay | 15 days (range: 1–109) | |
| Intra-hospital mortality | 24 (7.2%) | 1 (0.3%) |
| Destination on discharge | 1 (0.3%) | |
| Home | 210 (63.1%) | |
| Institution | 42 (12.6%) | |
| Peripheral hospital | 56 (16.8%) | |
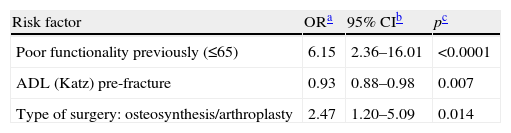
The status of the patients was analyzed after 6 months had elapsed since the date of the fracture. When the independent variables (ASA scale and fracture type are not included as they are similar to comorbidity and surgical intervention type, respectively) were contrasted to the dependent variable (functional impairment) by means of a multivariant logistic regression model, it was concluded that the prognostic factors for functional impairment after 6 months according to the hip function-pain scale are as reflected in Table 2.
Hip fracture: prognostic factors for functional impairment of the hip after 6 months using multivariant linear regression factors.
The patients presenting previous poor hip function (<65 points on the Martí-Valls scale) have 6 times more risk of presenting functional impairment (p<0.0001).
With respect to the activities of daily living, the higher the score on this scale prior to the fracture, the lower the risk of impairment. In fact, there is 7% less risk for each point scored by the patient on the scale prior to the fracture (p<0.007).
Patients subjected to osteosynthesis have 2.5 times higher risk of presenting functional impairment after 6 months than those who underwent arthroplasty (p<0.014).
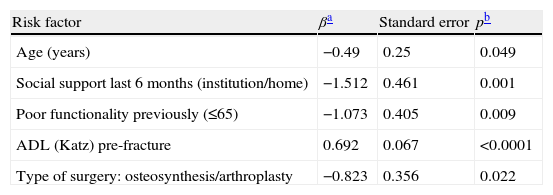
When the independent variables (comorbidity and fracture type are not included as they are similar to ASA scale and type of surgery, respectively) were contrasted to the dependent variable (Katz scale after 6 months) by means of a multivariant linear regression model, the prognostic factors for functional impairment for the activities of daily life in our study after 6 months are set out in Table 3.
Hip fracture: prognostic factors for functional impairment for the activities of daily living after 6 months using multivariant linear regression.
Age is a prognostic factor for presenting greater dependency in the activities of daily life (ADL) 6 months after suffering a hip fracture, unlike what happens for hip functionality (p<0.05).
Patients living in an institution or hospital 6 months on score on average 1.5 points lower on the Katz functional scale after 6 months, versus those living at home, whether in their own house or that of a relative (β=−1.512; standard error=0.461; p=0.001).
As occurs with the hip function-pain scale, previous poor functionality (<65 points) is a prognostic factor for greater dependency in the ADL after 6 months (p=0.009), a fact that is also repeated in those patients presenting a low score on the Katz scale prior to the fracture (p<0.0001).
Finally, patients undergoing osteosynthesis score on average almost one point less on the Katz scale after 6 months versus those receiving prostheses. Therefore, the type of surgery (and thus the fracture type) is a prognostic factor for functional impairment (dependency) in the activities of daily living after 6 months in patients over 65 years of age with hip fracture (β=−0.823; standard error=0.356; p=0.022).
DiscussionThose patients presenting poor hip function prior to the fracture, greater dependency in the activities of daily living and subjected to osteosynthesis have a higher risk of presenting functional impairment of the hip and dependency for the activities of daily living 6 months later. Therefore, the functional evolution of these patients might be predetermined on their admission to hospital.10
Age appears as a prognostic factor for functional impairment in the activities of daily living after 6 months.10–12,14–17 Holt et al.18 present good results (able to walk alone or with a cane) in 53.6% of the patients between 75 and 89 years of age, versus 9.7% of those over 95. However, Intiso et al.19 published a series in which 40% of their individuals over 90 years of age recovered the ability to walk unaided. These divergent results may be due to the lower mean age of their samples (92.6 years versus 96 years). Shah et al.20 coincide with our study, with impairment in the ADL (p=0.03) and walking ability (p=0.01) in patients over 90 years of age.
We did not find any differences between genders, the same as Saluelsson et al.,21 versus another study in which the multivariant analysis showed worse outcomes in males.22
Social support after 6 months is seen as a prognostic factor for functionality in the ADL.17 Independence is greater in patients living in a family setting versus those institutionalized or hospitalized. In addition, the risk of institutionalization is in turn related to greater age and poor functionality prior to the fracture.16
Poor functionality prior to the fracture seems to be the greatest underlying factor associated with the functional prognosis after 6 months, although it is suggested that cognitive function and depression may predict this functionality in the shorter term.23 Söderqvist et al.24 applied the SPMSQ (Short Portable Mental Status Questionnaire) to 213 patients with hip fracture and those scoring <3 had a worse functional prognosis in connection with the ADL, a higher risk of institutionalization, greater inability to walk and lower quality of life (p<0.001). In a sample with 73 individuals, Folden et al.25 established that cognitive function (p=0.01) together with balance (p<0.01) are the best predictors for functional capacity 3 months later.
Our results show that dependency with regard to the activities of daily living prior to the fracture is a predictive factor with great statistical significance for both the ability to walk (p=0.007) and to carry out these ADL 6 months after the fracture (p<0.0001), as confirmed by other authors.10–12,25
In our study, the type of intervention is closely related to the fracture type, as already explained above. In fact, extracapsular fractures undergo extramedullary osteosynthesis in 97.25% of cases, versus intracapsular cases that are mostly operated on with arthroplasty (91%). Walking with assistance is authorized from the start in the latter case, whereas extracapsular fractures (particularly if they are unstable) require a load-free period, thus delaying rehabilitation and their functional recovery. Long periods of hospitalization reduce muscle mass and the ability to move around, causing worse functional outcomes.26
In addition, extracapsular fractures are associated with a greater loss of bone mass, greater prevalence of vertebral fractures, greater age and a lower body mass index, i.e. a number of factors that might influence functional recovery.17
In our study, all extracapsular fractures (except for 5 cases) have been treated using extramedullary synthesis, whether they were stable or unstable and also sub-trochanteric fractures. Most of the studies comparing intramedullary synthesis with sliding hip screw find no differences in the outcomes for stable fractures.27–29 On the other hand, the results are better in unstable and sub-trochanteric fractures with the use of intramedullary devices.30–32
In conclusion, the profile of a patient admitted due to a hip fracture with the greatest risk of functional impairment would correspond to an individual over 85 years of age with an extracapsular fracture, a prior history of poor hip functionality, dependent on others for the activities of daily living and hospitalized or institutionalized 6 months on.
The best functional prognosis would correspond to a patient aged between 65 and 74 years of age with an intracapsular fracture, good hip functionality prior to the fracture, independent with regard to the activities of daily life and living in a family setting 6 months after the fracture occurred.
Level of evidenceLevel of evidence II.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Conflict of interestThe authors have no conflict of interests to declare.
Dr. Antonio Hinojosa and Dr. Francisco Díaz for their collaboration in data collection. Ana, Emi and Mari for their selfless collaboration in obtaining case reports.
Please cite this article as: Bravo-Bardají MF, et al. Factores pronósticos de incapacidad funcional en pacientes con fractura de cadera. Rev esp cir ortop traumatol. 2011;55(5):334–339.