Total quality, from a clinical management point of view, is a vast multidimensional concept. Its goal is providing a greater degree of satisfaction to patients and other users through planning and management of clinical and management activities, taking their needs and organisational and health expectations as a benchmark.
Currently, establishing total quality models means dealing with the stabilisation of 3 good practice subsystems from clinical management:
- •
Organisational subsystem: patient accessibility, the ability to respond to demand, and management of know-how and health technologies.
- •
Technical scientific subsystem: safe medical-surgical care, avoiding errors and variability, and effective practices through the implementation of protocols based on evidence or better experience.
- •
Benefit subsystem voiced by patients: establishing active listening mechanisms to improve the state of health, social and labour rehabilitation, as well as communication and comfort during their hospital stay.
There are presently different models that serve as a benchmark to work on total quality. In our case, once the different options were reviewed, we decided to endorse the International Standard ISO 9004:2000 project, which is aimed at managing and achieving incremental improvement in quality (benefits) by achieving guidelines framed within the 5 chapters contained in the Standard.
We need a precise perspective to be able to achieve the majority of these benefits. Its starting point is a diagnosis of the maturity level in performance, later attaining a vision that guides us towards a high level of definition and control over each of the processes subject to, not only to clinical unit management (management and support processes), but also operative factors (clinical processes based on diagnoses by homogeneous patient groups, Diagnosis-Related Groups [DRG]).
In this paper we present, first of all, the result of self-assessment by the Orthopaedic Surgery and Traumatology Department (from now on, OSTD) of the Hospital Infanta Cristina, located in Parla (Community of Madrid), after Standard's questionnaire was applied. Secondly, we describe the conceptual framework of clinical management by processes and to finish off, we set out 2 cases of stabilisation processes: a management process and a clinical process that form part of the OSTD process map.
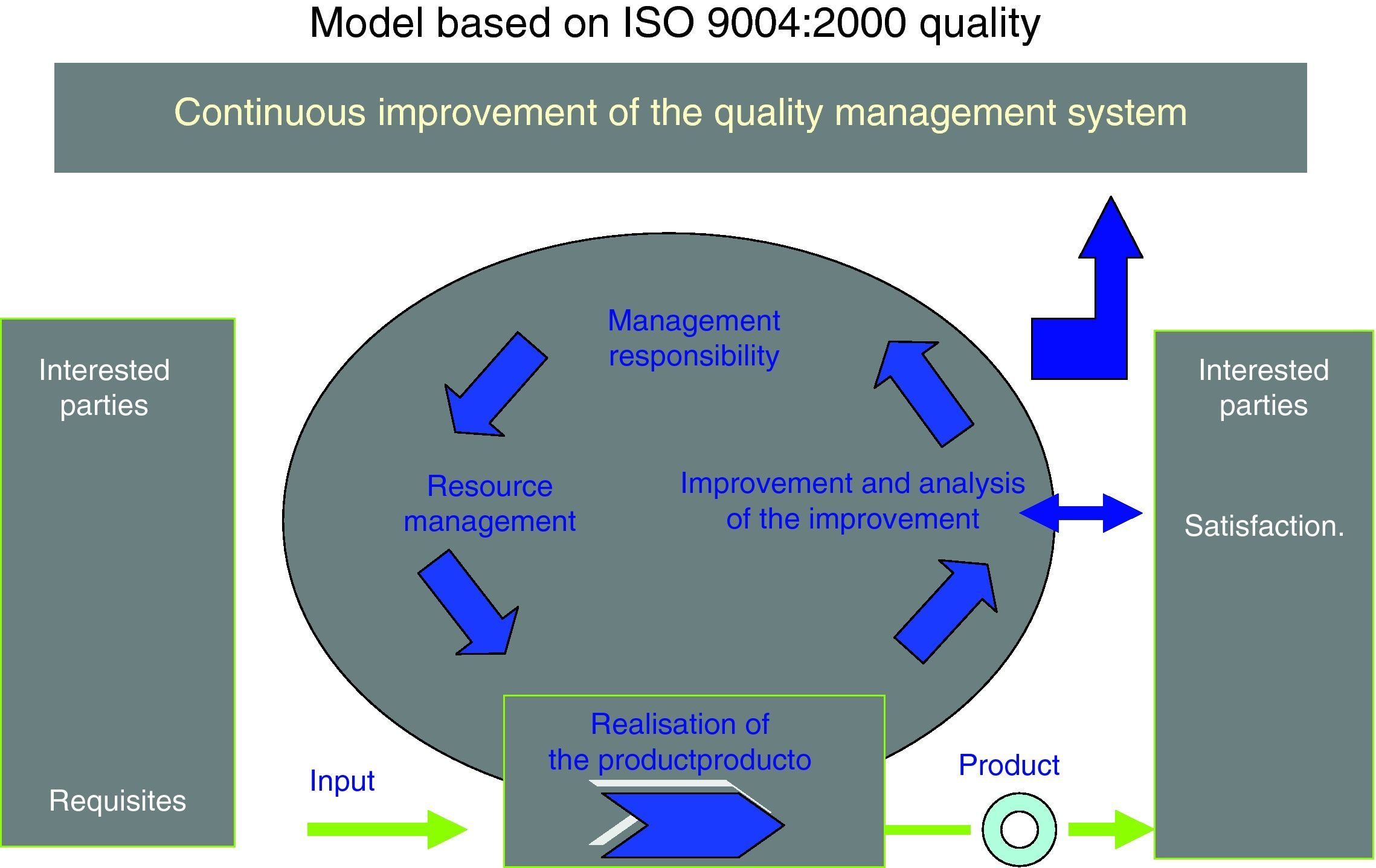
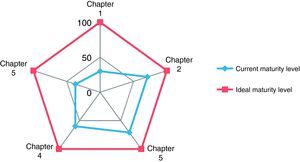
Self-assessment and determination of OSTD maturity in applying the ISO 9004:2000 StandardThe International ISO 9004:2000 Standard (Fig. 1) provides general guidance on an expansive range of an organisation's quality system, that is, it does not include specific guidance on the management systems for goods and services and therefore represents an effort to adapt to the sector where it is to be applied. In the case of the health sector, we have not found any previous references to self-assessment using this Standard. Consequently, we have made an effort to adapt the quality objectives of the OSTD to the principles that the Standard sets out, through validating the questionnaire that it proposes.
The Standard is therefore a tool for continuous improvement towards excellence. It considers, as a starting point, what to improve (weak points identified through self-assessment) and how to improve (focus on management by processes) (Fig. 1).
As we can see in this figure, there are 5 chapters or assessment areas in the model to gradually increase quality: quality management system, management responsibility, resource management, product realisation, and improvement measurement and analysis. Properly managing the clinical organisation of these chapters would produce the following benefits, which are benchmarks to achieve:
- •
There would be a systematic and visible way to conduct and operate the clinical service that would continuously improve its performance within the processes.
- •
Department heads would be coherently and visibly involved with quality management.
- •
The centre's management would ensure through a contract/management programme with the clinical department that there would be sufficient resources available (in terms of staff, infrastructures and technology, a safe working environment, partners, external suppliers, etc.) to reach these targets.
- •
This would be combined with institutional support in the approach to processes and other departmental activities so as to obtain the desired results.
- •
There would be a clinical information system that would ensure effective and efficient data collection, validating it, processing it, and generating the evaluative metrics to continue improving.
The Standard's directives, as part of the excellence applied, set out 4 phases to achieve excellence targets in our clinical department:
- I.
Establish a preliminary self-assessment to determine how advanced a service is with regard to clinical performance and management.
- II.
Identify the prevalent problems and convert them into opportunities to improve.
- III.
Go from a task-based performance system contained in procedures to a system of clinical management by processes aimed at satisfying needs and expectations of both the users of the service and the other interested parties in internal hospital organisation.
- IV.
Reassess the management system and set parameters according to the improvement achieved, which in turn would deeply motivate members of staff to continue improving.
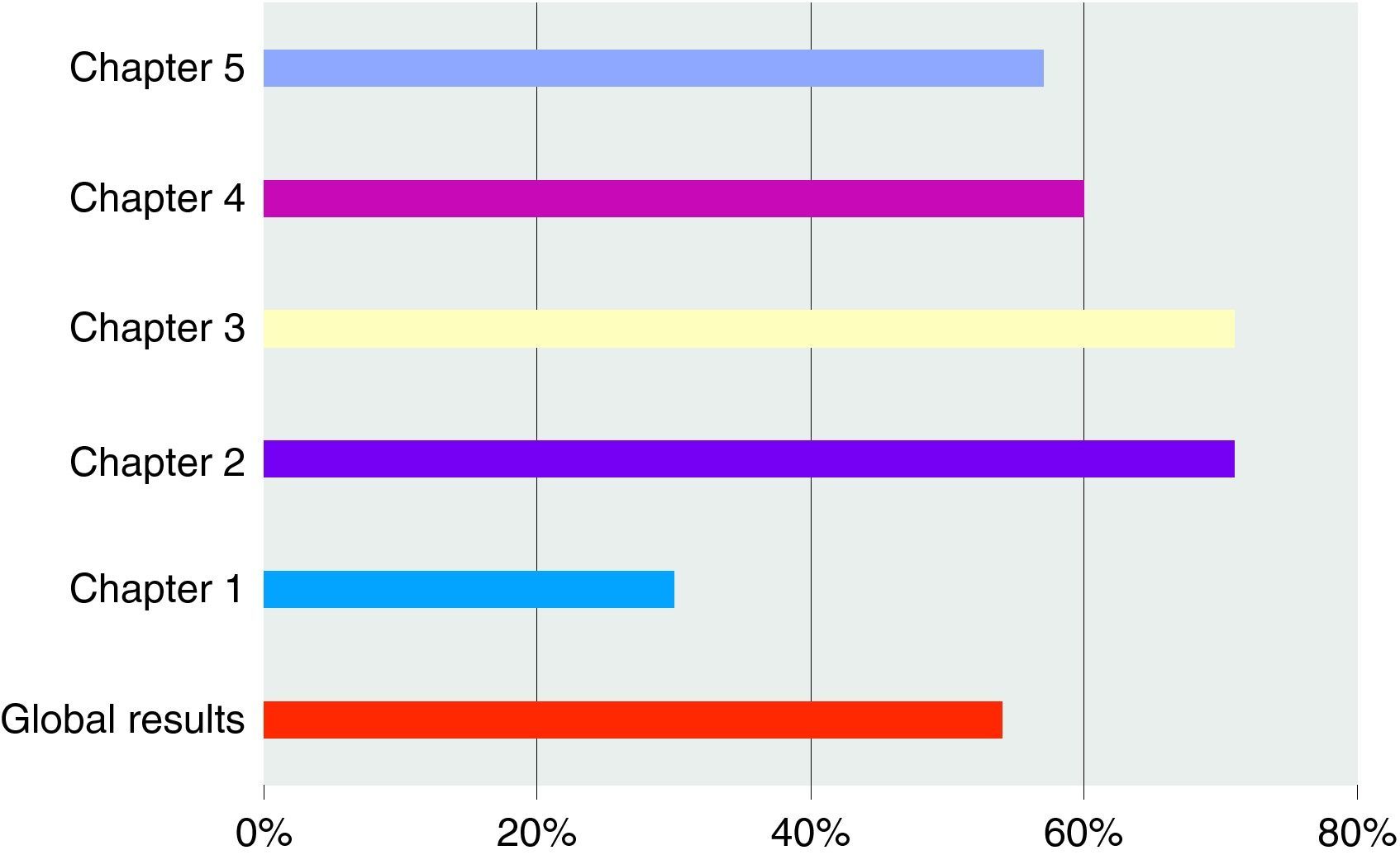
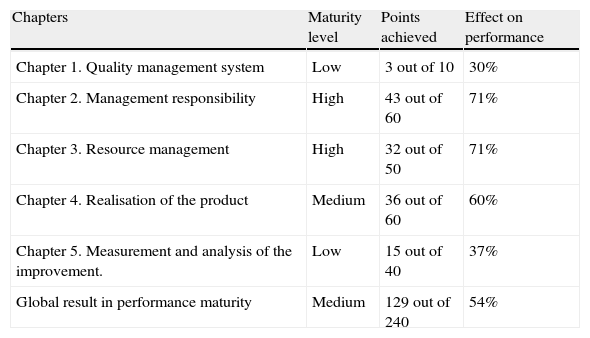
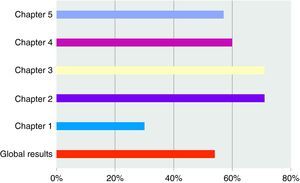
The overall result determines a mean position of OSTD (54%) with respect to the maturity attained in performance within a benchmark quality system ISO 9004:2000. By chapters, we find the following observations:
- I.
Chapter 1: quality management is found to have a low performance level (37%), because there is no approach based on processes. To overcome this, we should design an OSTD process map, as well as document management and operational processes.
- II.
Chapter 2: OSTD management responsibility shows a high maturity level (71%). This chapter's strong points lie in: (a) the department heads’ commitment and involvement in improving quality; (b) the identification and reasonable handling of the interested parties’ requirements; (c) proper determination of the mission and vision of this department; (d) efficient transmission of organisational directives to the team, although some channels of communication should be improved; and (e) proper department assessment of the support received from hospital management.
- III.
Chapter 3: resource management also presents a high performance maturity level (71%). As strong points, we should emphasise the following: (a) good facilitation of resources by the hospital management; (b) good infrastructure for work development; (c) high staff motivation; and (d) a good relationship and partnership with suppliers and other benchmark services, even though we must research coordination sources. A line to be improved in this chapter is that related with the definition of staff competencies and more trained and auxiliary staff.
- IV.
Chapter 4: product realisation shows a medium maturity level. As strong points we find: (a) support by hospital management in carrying out activities and the hospital management's focus on processes for clinical services; (b) planning, replacement, processing and management of nonconformities by acquiring specific products to develop departmental activity; and (c) control and monitoring of production through a balanced scorecard. As lines to improve we identify the following: (a) process design and development, and (b) the description of the department's own protocols: clinical guides and organisation guidelines.
- V.
Chapter 5: measurement and analysis of the improvement presents a low performance level (37%). This is the obvious consequence of already having a process approach, which has its own nonconformity assessment and control system. As this approach is not well established, it is practically impossible for the continuous improvement system for quality to be currently developed under the criteria set out in the Standard.
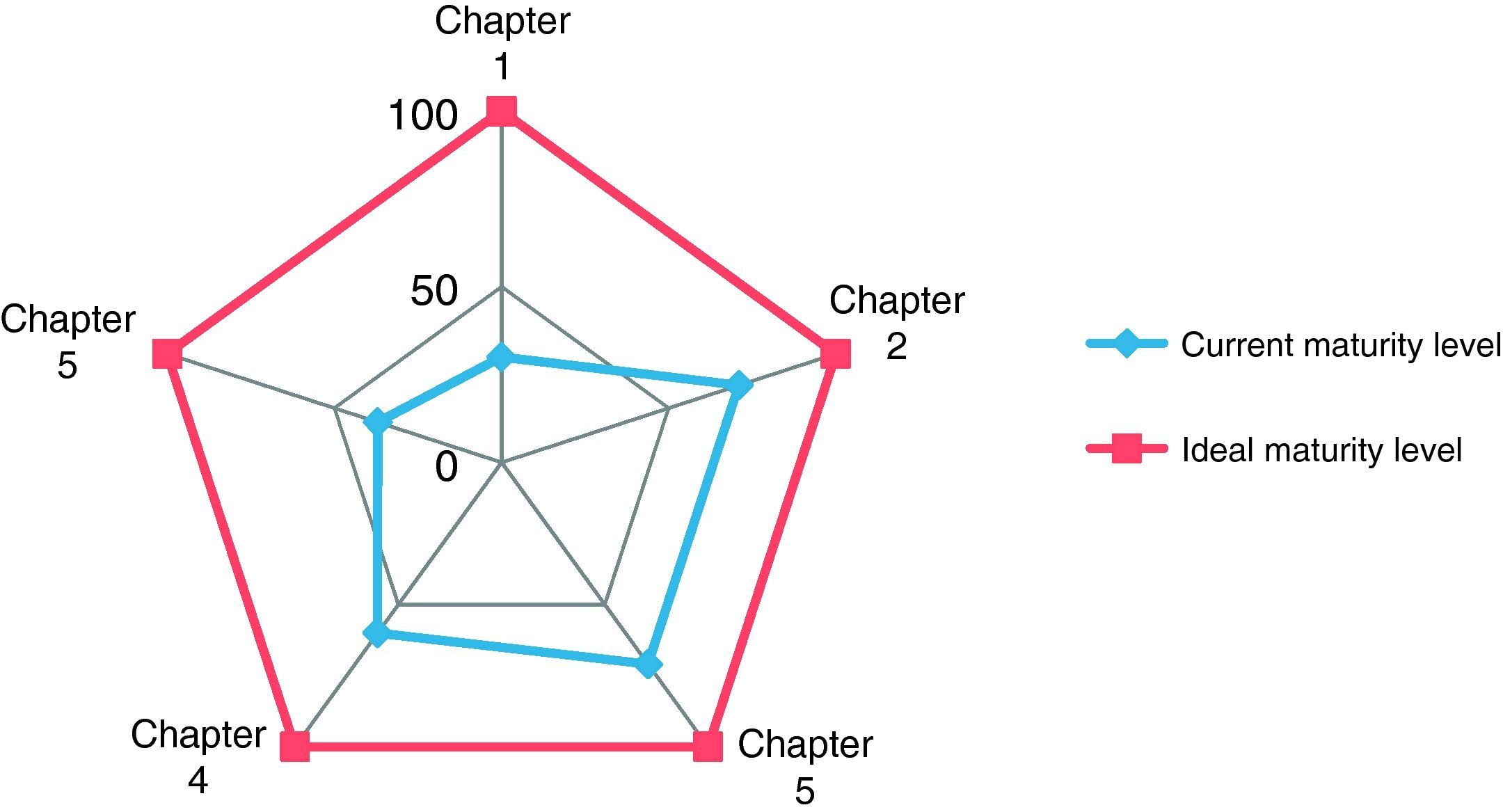
Table 1 and Figs. 2 and 3 present the results obtained in the OSTD self-assessment both comprehensively and by the different chapters proposed by the Standard.
Results of the performance level.
| Chapters | Maturity level | Points achieved | Effect on performance |
| Chapter 1. Quality management system | Low | 3 out of 10 | 30% |
| Chapter 2. Management responsibility | High | 43 out of 60 | 71% |
| Chapter 3. Resource management | High | 32 out of 50 | 71% |
| Chapter 4. Realisation of the product | Medium | 36 out of 60 | 60% |
| Chapter 5. Measurement and analysis of the improvement. | Low | 15 out of 40 | 37% |
| Global result in performance maturity | Medium | 129 out of 240 | 54% |
From the results obtained through self-assessment by the Standard, we have designed a Quality Control Plan for the Department based on processes, which has the following characteristics:
- I.
Reason for improvement. Once the weak quality points have been identified in the self-assessment, we should consider the appropriateness of setting them up or not.
- II.
Current position and analysis. All improvement needs prior critical analysis of the starting point. We should identify the causes and the root of the problem.
- III.
Formulate an improvement target. The target should be the expected result. To measure the effectiveness of achieving the target, it should be formulated properly with the following characteristics: change indicator, problem; quantity or quality indicator and time to achieve it.
- IV.
Manager. The person who follows up the improvement.
- V.
Procedure. How the change is going to be undertaken.
- VI.
Assessment. We should confirm that the problem has been resolved and the expected result has been attained through a second self-assessment on a specified date.
We have identified 2 different routes to improve quality according to the specifications of the ISO 9004:2000 Standard.
- I.
Projects with significant progress. The improvement target is aimed at achieving focused standards: department approach to processes and procedure book. These approaches will be undertaken by presenting a specific project for each one and project management techniques will be applied.
- II.
Improvement activities for quality defects. The improvement targets will be based on resolving quality defects in existing projects and processes. They will be managed through documented tasks following management and quality control techniques.
In this paper we focus on describing the applied clinical management model by processes by means of 2 sections:
- •
Methodological planning of the management base by processes collecting the conceptual framework of the method.
- •
Description of 2 types of sample processes: a management process that ensures organisational quality and an operative or clinical process that assures technical quality.
A process is nothing more that a set of decisions, activities and tasks that should be carried out in a coordinated fashion with the aim of satisfying patients’ needs and expectations, as well as those of other parties interested in the results.
All the activities by processes in the health sector should have an added value. This quality consists of carrying out the tasks with organisational quality (in time and manner and assigned resources coherent with rational decision-making) and scientific and technical quality (scientific evidence or agreed best practices in clinical procedures). That is, the result of the products obtained should try to obtain the “clients”’ satisfaction in terms of health: operating or clinical processes and/or performance facilitation: management and support processes.
The process maps show us the work structure and organisation in a Centre or Operating Unit by identifying and modelling the processes, so as to provide information on where the activity is located, how to establish relationships and to what end they are aimed.
A process map is therefore no more than a diagram, which visually shows the types of processes in the environment being considered, as well as in the relationships that are established between them. These diagrams are structured by levels or degree of functions with their corresponding links, thus offering the opportunity to improve coordination between the interfaces of the organisational activity. Likewise, they also offer clues to distinguish the typology of processes the organisation has. In a health company, we find practically all types of processes: key, strategic, management and operational, making this the first step to choose the processes in which to act as a supplier.
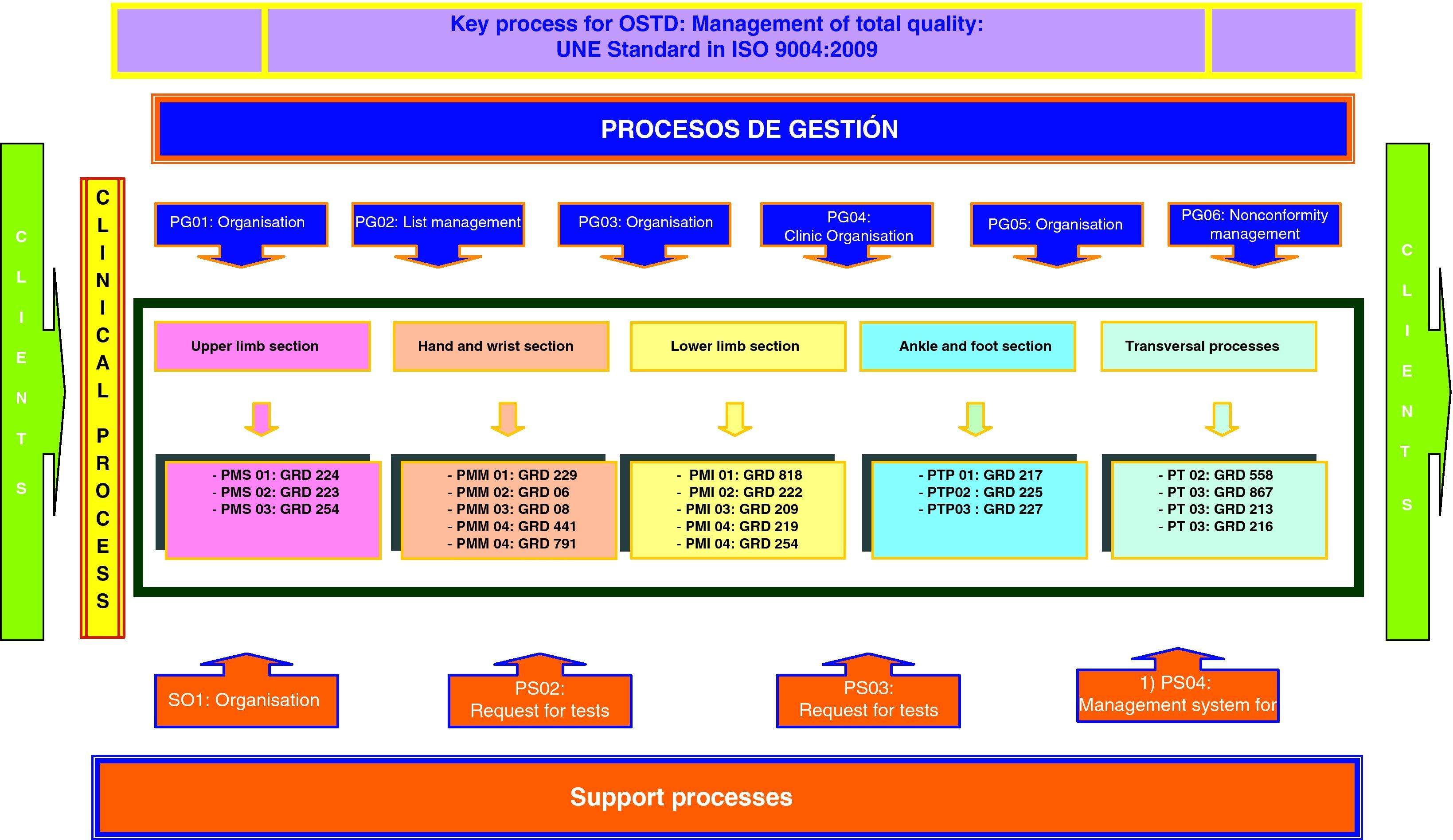
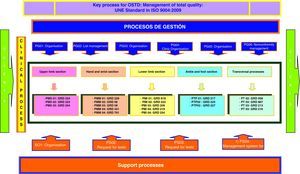
In our case, the process map for the OSTD (Fig. 4) has been designed following the activity block methodology by Integration Definition Function Model (IDEF) boxes. These boxes provide process input and output flows: client requirements, regulations and guidelines for actions, resources and their suppliers, and product output definitions. The types of processes that we have recognised for our map are the following:
- •
Key process: set of managerial decisions aimed at the management of projects and activities that guarantee the quality of the intermediate and final products of the OSTD according to the international ISO 9004:2000 Standard.
- •
Management processes: aimed at planning and organisation of activities in the different areas in which OSTD acts, helping in the tasks and responding to the nonconformities.
- •
Clinical or operative processes: clinical procedures aimed at recovering the health of the users (patients) classified by the diagnosis-related group (DRG) information system. These processes are grouped according to the different sections in which the OSTD activity is organised.
- •
Support processes: management of training activities and requests for diagnostic tests that help in decision-making and professional skills in carrying out the clinical processes.
The methodology that we set out to develop management by processes generally consists of the systemic deployment of 4 successive and coordinated phases with their corresponding stages.
Phase 0: Mobilisation of the organisationThis phase aims for the head of department to recruit people who want to get involved in improving quality in the operation of OSTD and the processes it provides its users.
The phase starts by training functional groups; it is important that when you do not have experience in this field, the people comprising these teams should receive a training programme in clinical management by processes methodology. The mission of the work teams consists of planning a relevant project to help the organisation to steer itself towards best practices and satisfy the requirements of the interested parties. The stages of this phase are dealt with gradually in the following way:
- I.
Create a team and plan a project.
- II.
Identify the organisation's processes and carry out a process map.
- III.
Prioritise the processes to be documented.
- IV.
Designate a process coordinator or process “packages”.
In this phase we determine the requirements needed by the team, suppliers and (if applicable) the clients of this process to get to know about the process. The aim is to place the process under control, so that it is well documented and understood. A process is correctly documented when we have stated in writing its design attributes:
- I.
Mission of the process.
- II.
Initial and final limit.
- III.
Clients’ needs and expectations.
- IV.
Input and output flows.
- V.
Regulations and guidelines by way of procedures or clinical trajectories.
- VI.
Estimate of direct costs.
- VII.
Metrics: criteria, indicators and standards.
- VIII.
Diagram of the process.
In this phase we hope to establish, either during the pilot stage or once the process has been standardised, a procedure based on the assessment of the performance measures: the operation of its structural elements and the results being obtained, so as to find their level of benefits and set up corrective measures if necessary.
The following should be monitored and assessed: users/patients (to see if they are properly identified and if the quality they perceive is correct); structural elements (referring to the availability and maintenance of resources, logistical organisation, working guidelines and information system); activities that are carried out in the processes (if they are performed, how they are done and by whom); results obtained (improvement of health care data and later management of the stabilisation) together with the effects achieved (results of the key indicators for productive performance and satisfaction for internal and external clients). The 2 stages are:
- I.
Monitoring of indicators and scorecard.
- II.
Assessment of processes.
Improvement of the processes is already implied by the development of the previous phases themselves. However, advanced training in best practices (or, in other words, aiming for excellence) can be obtained by 2 non-exclusive means: gradual improvement or radical improvement.
Gradual or permanent improvement is used to rectify certain defects in existing processes. That is, we seek to improve activities or some of the tasks present in the operation of the process.
Radical improvement covers the root process; it is used to create or totally change the process. It is said that re-engineering is “picking up a pencil and designing a new process or completely redesigning an existing process,” so as to reach a new vision and new goals or to generate dramatic improvements in time, service, quality and process costs.
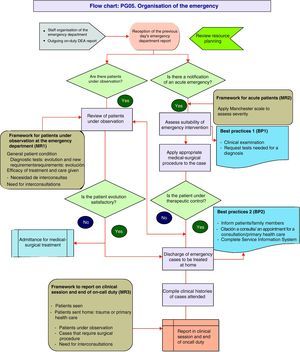
Examples of documented processesTo complete this paper, we attach 2 documented processes. The first one is a management process aimed at managing people and users who come to the emergency department. The process is coded as PG05: “Organisation of the emergency.” The second example is an operative or clinical process that corresponds to the section of a wrist and hand. This is coded as PMM03. DRG 08: “Procedures on cranial and peripheral nerves and other surgical procedures without complications.”
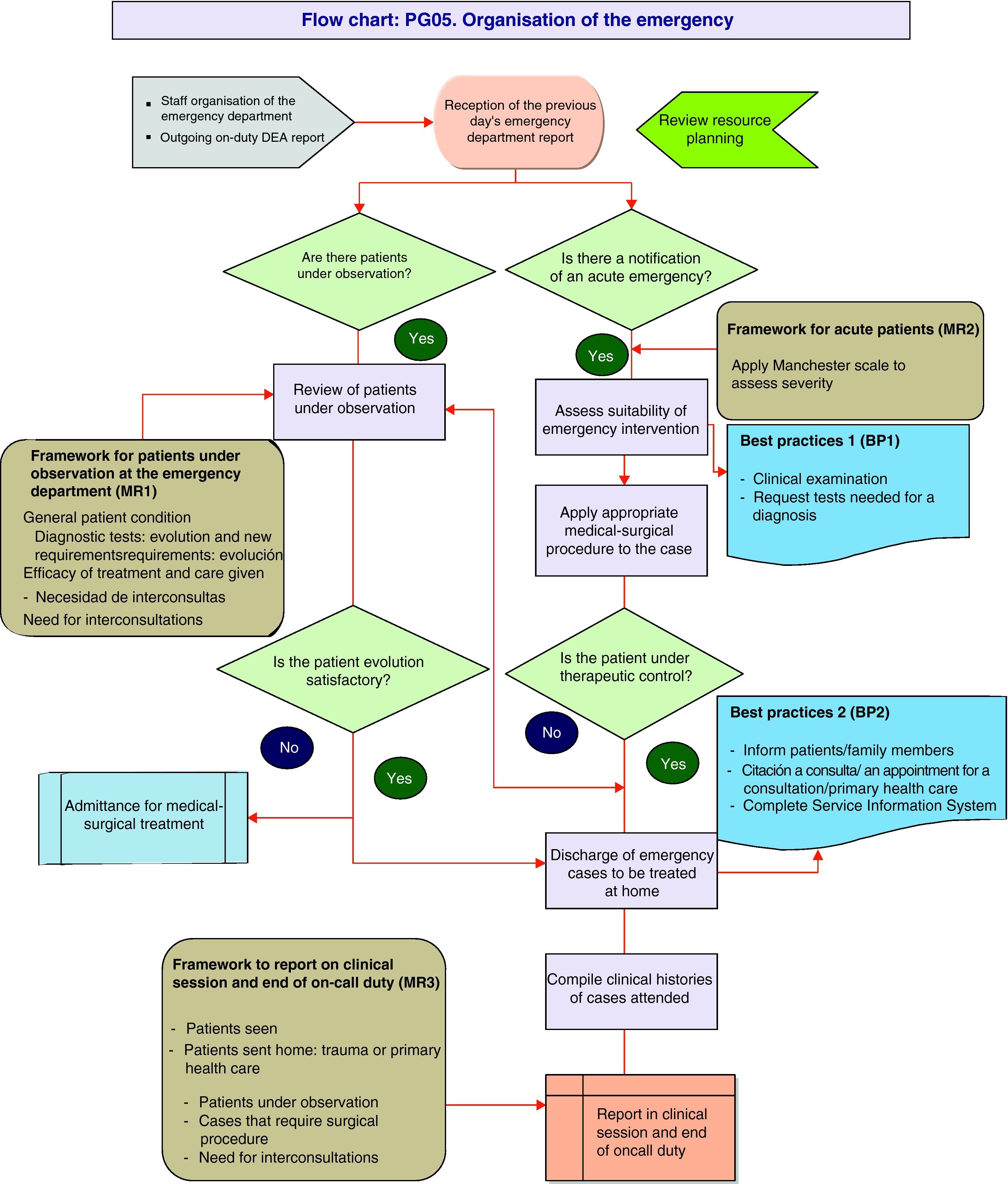
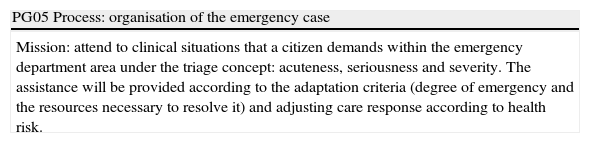
PG05 process: Organisation of emergency care in the OSTDThe process plans the distribution of medical tasks and decision guidelines to improve the efficiency in flow and control of patients in the traumatology emergency department. The process currently faces problems of space in this particular speciality, as well as the availability of operating theatres to deal with emergency surgery, which is why we propose measures based on adapting resources to needs and demand (Table 2 and Fig. 5).
PG05 process: organisation of the emergency case.
| PG05 Process: organisation of the emergency case |
| Mission: attend to clinical situations that a citizen demands within the emergency department area under the triage concept: acuteness, seriousness and severity. The assistance will be provided according to the adaptation criteria (degree of emergency and the resources necessary to resolve it) and adjusting care response according to health risk. |
| Initial limit | Entry/position of the area specialist physician (ASP) at 8.30 in a clinical session defined in the monthly chart for on call schedules. | Time |
| Final limit | End of duty report, collecting the clinical histories of patients seen: not admitted, admitted and under observation. | 24h/day |
| Clients | |
| Main | Secondary |
| OSTD Medical staff | Patients |
| Suppliers | |
| Head of Department: work organisation template | |
| Area Specialist Physician (ASP): putting into practice operating procedure in the emergency department area, on the ward (public holidays, afternoons and working nights) and operating theatre if there is a surgical emergency | |
| Client needs and expectations |
| 1. Know beforehand about the on-duty roster for on-site and located duties |
| 2. Know about the specifications that regulate technical quality in organising work in the emergency department |
| 3. Have the necessary technical resources to develop the activities |
| Inputs | |
| Resources | Documents |
| 1 on-site ASP (24h) | |
| 1 located ASP (17 working hours, 24 public holidays) | |
| 1 support doctor (7h on working days, 14h on public holidays). Note 1 | On-duty template for OSTD |
| Plaster room, trauma box, treatment room Computer support (Selene and Manchester) | Operative procedure for the process |
| Output |
| Patient discharged with correctly completed care report. |
| Patient admitted to the hospital because of need for medical surgical monitoring. |
| Metrics. |
| Criteria: there are requisites for the process and these are apt for both suppliers and clients. |
| Indicators: medical turnover rate in the emergency department. Standard: 1 on-call/12 days, with seasonal variation. |
| - Emergencies attended to: monthly/annual monitoring |
| - Emergency discharges |
| - Discharges due to admittances |
| - Reviews (in 48h) |
| - Patients admitted (percentage of emergency admissions). |
| - Emergencies operated on during the on-duty |
| - Mortality index |
| - Time of response from the trauma or support ASP according to priority on the Manchester scale: |
| • 240min (blue); |
| • 120min (green); |
| • 60min (yellow); |
| • 10min (orange); |
| • Extreme emergency (red). |
| Frequency of the process: | Monthly | 30–31 | |||
| Yearly | 365 | ||||
| Those in charge | Dr Fernando Delgado.Dr Gustavo Aparicio. | Revision | Once a month |
| Notes |
| Note 1: From our point of view, emergency care would improve with 2 ASP who were physically present for only on-call duties, independently of the ASP assigned to the ward and with a 24-h support doctor this would make good use of the morning emergency operating theatre. |
| Note 2. It is necessary to classify the emergency demand for trauma in the emergency department area, also taking into account that of adults and children. |
| Note 3: The triage of trauma patients should be undertaken by an expert in the field. |
| PG05 procedure |
| People in charge of the process: |
| – Draw up an organisation template for the emergency department in the OSTD once a month, within work organisation template of the OSTD. |
| – Put the template on the intranet of the OSTD/ communicate by email to the department doctors. |
| ASP assigned to the emergency department: |
| – Reception and reading of the relevant information relating to the previous days’ on-call duty. |
| – Review the number and characteristics of patients in the emergency department observation area: patient's general condition and vital signs, diagnostic tests, interconsultations, medical treatment. |
| – Take care of the medical-surgical problems that arise in those patients that have already been assessed in the emergency department area (boxes and observation) or admitted to a ward. |
| – Reception of the new emergency trauma demands by applying standards according to the Manchester scale: clinical examination and request for additional tests for diagnosis. |
| – Provide therapeutic care measures required by the patient according to the diagnosis undertaken. |
| – Create a discharge report according to the evolution and type of patient. |
| – Complete the additional necessary documentation per patient attended to in the emergency department (report or notes from ED, appointment for consultations, prescription, report on injuries, etc.). |
| – Carry out urgent interconsultations requested by other clinical departments. |
| – Complete the clinical information in the Service Information System (SIS), to which the ASP assigned to the emergency case is in charge. |
| – Assess the relevant incidences and information, if applicable to those in charge of the on-call duty (head of the emergency department, hospital chief, department head). |
| – Manage collection of clinical histories of patients attended at the thematic morning clinic. |
| – Report at the clinic of the cases seen: number of emergencies attended, types of emergencies, clinical cases, incidences, patients admitted, patients in the emergency department who are pending resolution, emergency surgeries pending, etc. |
| – Hand over the on-call duty to the incoming ASP according to the organisation template of OSTD. |
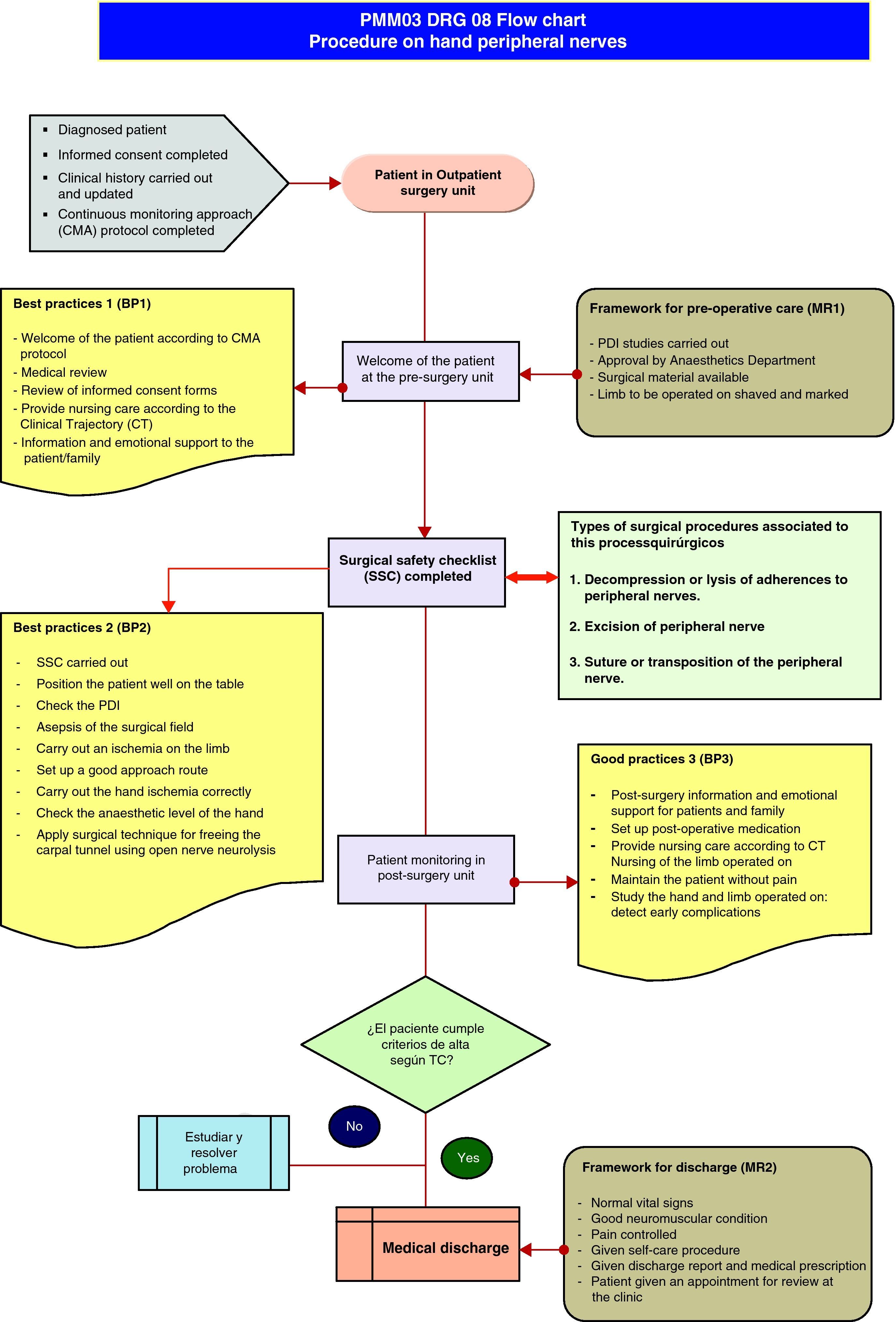
The process seeks a surgical solution to neuropathic pain and loss of the ability to move limbs, and sleep quality in patients with peripheral nerve lesions due to compression, wounds, tumours or complications from previous surgeries. This is carried out by Outpatient Surgery, which means there is no hospital stay after the surgical procedure and the subsequent follow-up in outpatients lasts approximately 3 months.
PMM03 process: DRG 08The process covers procedures on cranial and peripheral nerves and other surgical procedures without complications (Fig. 6).
Definition of the processIt is a surgical DRG that groups together patients admitted because of a nervous system disease and whose cranial or peripheral nerves have been operated on (except freeing the carpal tunnel) or who have had stereotaxic surgery or had a pace-maker fitted. The most frequent interventions are: excision of the cranial or peripheral nerve, decompression or lysis of adherences to peripheral nerves or ganglia, suture or transposition of a nerve or spinal neurostimulator implantation.
Type of careOutpatient surgery.
Types of procedures associated to this process:
- I.
Decompression or lysis of adherences to peripheral nerves.
- II.
Excision of the peripheral nerve.
- III.
Suture or transposition of the peripheral nerve.
- I.
Upper control limit for discharge (UCL): 1 day.
- II.
Lower control limit for discharge (LCL): 0 days.
- III.
Mean time for discharge (MTD): 1 day (Tables 3 and 4).
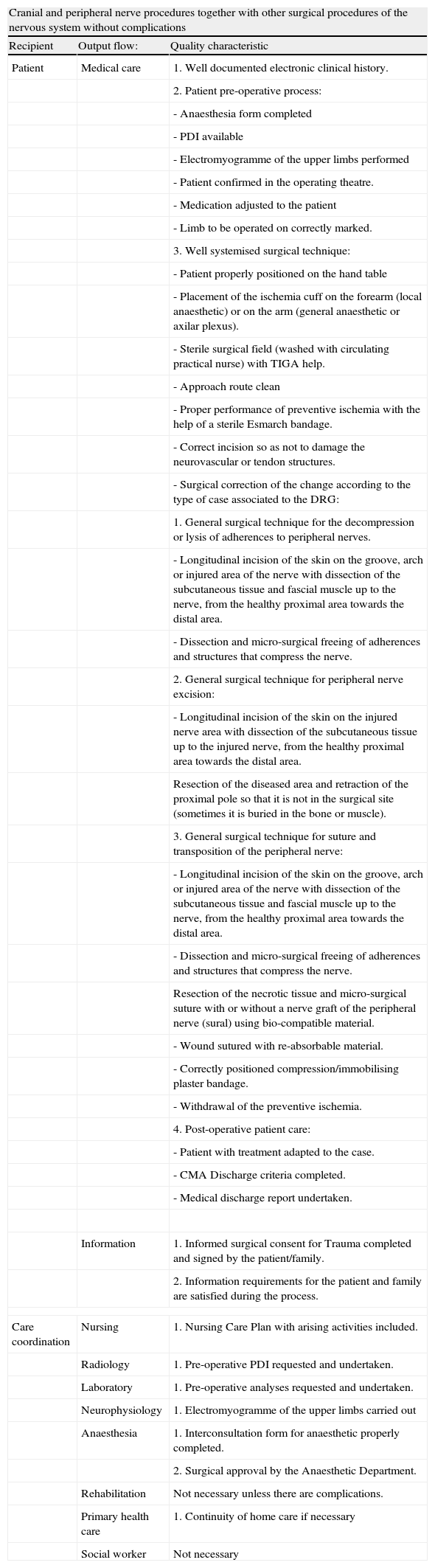
Table 3.Quality and safety attributes in the output process flows. Cranial and peripheral nerve procedures, together with other surgical procedures of the nervous system without complications.
Cranial and peripheral nerve procedures together with other surgical procedures of the nervous system without complications Recipient Output flow: Quality characteristic Patient Medical care 1. Well documented electronic clinical history. 2. Patient pre-operative process: - Anaesthesia form completed - PDI available - Electromyogramme of the upper limbs performed - Patient confirmed in the operating theatre. - Medication adjusted to the patient - Limb to be operated on correctly marked. 3. Well systemised surgical technique: - Patient properly positioned on the hand table - Placement of the ischemia cuff on the forearm (local anaesthetic) or on the arm (general anaesthetic or axilar plexus). - Sterile surgical field (washed with circulating practical nurse) with TIGA help. - Approach route clean - Proper performance of preventive ischemia with the help of a sterile Esmarch bandage. - Correct incision so as not to damage the neurovascular or tendon structures. - Surgical correction of the change according to the type of case associated to the DRG: 1. General surgical technique for the decompression or lysis of adherences to peripheral nerves. - Longitudinal incision of the skin on the groove, arch or injured area of the nerve with dissection of the subcutaneous tissue and fascial muscle up to the nerve, from the healthy proximal area towards the distal area. - Dissection and micro-surgical freeing of adherences and structures that compress the nerve. 2. General surgical technique for peripheral nerve excision: - Longitudinal incision of the skin on the injured nerve area with dissection of the subcutaneous tissue up to the injured nerve, from the healthy proximal area towards the distal area. Resection of the diseased area and retraction of the proximal pole so that it is not in the surgical site (sometimes it is buried in the bone or muscle). 3. General surgical technique for suture and transposition of the peripheral nerve: - Longitudinal incision of the skin on the groove, arch or injured area of the nerve with dissection of the subcutaneous tissue and fascial muscle up to the nerve, from the healthy proximal area towards the distal area. - Dissection and micro-surgical freeing of adherences and structures that compress the nerve. Resection of the necrotic tissue and micro-surgical suture with or without a nerve graft of the peripheral nerve (sural) using bio-compatible material. - Wound sutured with re-absorbable material. - Correctly positioned compression/immobilising plaster bandage. - Withdrawal of the preventive ischemia. 4. Post-operative patient care: - Patient with treatment adapted to the case. - CMA Discharge criteria completed. - Medical discharge report undertaken. Information 1. Informed surgical consent for Trauma completed and signed by the patient/family. 2. Information requirements for the patient and family are satisfied during the process. Care coordination Nursing 1. Nursing Care Plan with arising activities included. Radiology 1. Pre-operative PDI requested and undertaken. Laboratory 1. Pre-operative analyses requested and undertaken. Neurophysiology 1. Electromyogramme of the upper limbs carried out Anaesthesia 1. Interconsultation form for anaesthetic properly completed. 2. Surgical approval by the Anaesthetic Department. Rehabilitation Not necessary unless there are complications. Primary health care 1. Continuity of home care if necessary Social worker Not necessary PMM 03 process: DRG 08: cranial and peripheral nerve procedures and other surgical procedures of the nervous system without complications Mission: to provide a surgical medical service to all patients who present pain, loss of mobility, paresthesias and emotional changes due to compression, section or peripheral nerve disease in the limbs, to recover the ability to move them and have appropriate night time sleep quality. Initial limit Admittance of the patient to the Outpatient Surgery Unit. Average time Final limit Hospital discharge (review of Nursing and Trauma external cons). 1 day Clients Main Secondary Diagnosed patient Patient's family: Suppliers Doctors of the Orthopaedic Surgery and Trauma Department Doctors of the Anaesthetics and Reanimation Department. Doctors and Technicians of the Diagnostic Imaging Department. Laboratory Doctors and Technicians. Doctors of the Neurophysiology Department. Nursing Staff: Practical nurses and Auxiliaries. TIGA Staff. Rehabilitation doctors and physiotherapists (if required). Clients needs and expectations Follow observations of the requirements and expectations for all the operating processes. Input Special resources Documents Magnifying Glasses or micro-surgery microscope. Clinical history. Sterile ischemia: sterile Esmarch bandage, sterile silicone ischemic cuff. Electronic documents of tests requested. Biological agents to impede post-surgical fibrosis and stimulate neural growth. Operating theatre incident report. Auto-graft of the peripheral nerve. Clinical trajectory. Drugs. Hand surgery box. Output Continue observations of quality attributes and safety process. Metrics Criteria: there are requisites for the process and they are apt for both suppliers and clients. Indicators: Number of ASA I patients (do not need pre-anaesthesia). Number of process discharges. Mean stay of the process Frequency of the process: Monthly 5 Yearly 50 Cost Manager Person in charge of Hand and wrist section Review 6 months Notes: Classification of the surgical risk in American Society of Anaesthesiology (ASA) levels:
ASA I: healthy patient.
ASA II: mild systemic disease with no functional limitations.
ASA III: serious systemic disease with serious functional limitation.
ASA IV: serious systemic disease which is life threatening.
ASA V: patient not expected to survive more than hours with or without surgery.
ASA E: patient requires an emergency operation. An E is added (to the previous 5 classifications) when an emergency operation has to be carried out.
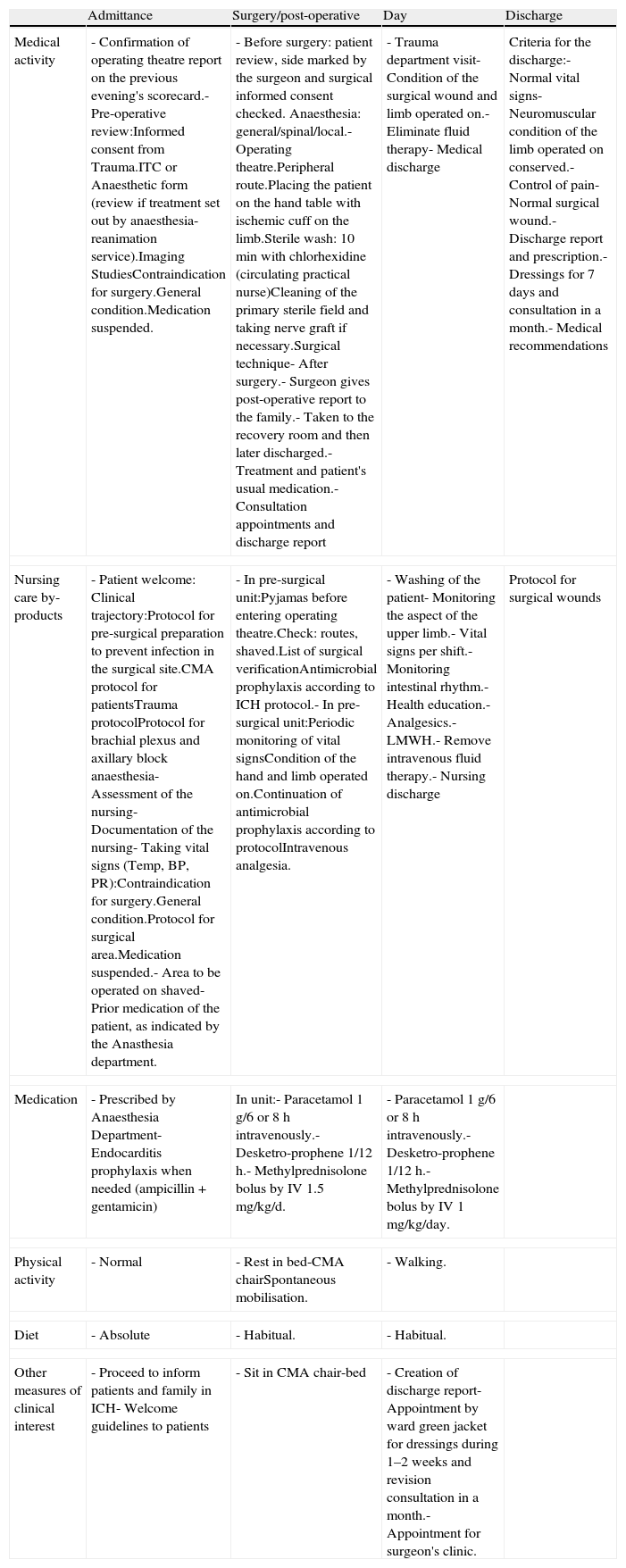
Table 4.PMM 03 process. DRG 08: cranial and peripheral nerve procedures and other surgical procedures of the nervous system without complications. Clinical trajectory (CT).
Admittance Surgery/post-operative Day Discharge Medical activity - Confirmation of operating theatre report on the previous evening's scorecard.- Pre-operative review:Informed consent from Trauma.ITC or Anaesthetic form (review if treatment set out by anaesthesia-reanimation service).Imaging StudiesContraindication for surgery.General condition.Medication suspended. - Before surgery: patient review, side marked by the surgeon and surgical informed consent checked. Anaesthesia: general/spinal/local.- Operating theatre.Peripheral route.Placing the patient on the hand table with ischemic cuff on the limb.Sterile wash: 10min with chlorhexidine (circulating practical nurse)Cleaning of the primary sterile field and taking nerve graft if necessary.Surgical technique- After surgery.- Surgeon gives post-operative report to the family.- Taken to the recovery room and then later discharged.- Treatment and patient's usual medication.- Consultation appointments and discharge report - Trauma department visit- Condition of the surgical wound and limb operated on.- Eliminate fluid therapy- Medical discharge Criteria for the discharge:- Normal vital signs- Neuromuscular condition of the limb operated on conserved.- Control of pain- Normal surgical wound.- Discharge report and prescription.- Dressings for 7 days and consultation in a month.- Medical recommendations Nursing care by-products - Patient welcome: Clinical trajectory:Protocol for pre-surgical preparation to prevent infection in the surgical site.CMA protocol for patientsTrauma protocolProtocol for brachial plexus and axillary block anaesthesia- Assessment of the nursing- Documentation of the nursing- Taking vital signs (Temp, BP, PR):Contraindication for surgery.General condition.Protocol for surgical area.Medication suspended.- Area to be operated on shaved- Prior medication of the patient, as indicated by the Anasthesia department. - In pre-surgical unit:Pyjamas before entering operating theatre.Check: routes, shaved.List of surgical verificationAntimicrobial prophylaxis according to ICH protocol.- In pre-surgical unit:Periodic monitoring of vital signsCondition of the hand and limb operated on.Continuation of antimicrobial prophylaxis according to protocolIntravenous analgesia. - Washing of the patient- Monitoring the aspect of the upper limb.- Vital signs per shift.- Monitoring intestinal rhythm.- Health education.- Analgesics.- LMWH.- Remove intravenous fluid therapy.- Nursing discharge Protocol for surgical wounds Medication - Prescribed by Anaesthesia Department- Endocarditis prophylaxis when needed (ampicillin+gentamicin) In unit:- Paracetamol 1g/6 or 8h intravenously.- Desketro-prophene 1/12h.- Methylprednisolone bolus by IV 1.5mg/kg/d. - Paracetamol 1g/6 or 8h intravenously.- Desketro-prophene 1/12h.- Methylprednisolone bolus by IV 1mg/kg/day. Physical activity - Normal - Rest in bed-CMA chairSpontaneous mobilisation. - Walking. Diet - Absolute - Habitual. - Habitual. Other measures of clinical interest - Proceed to inform patients and family in ICH- Welcome guidelines to patients - Sit in CMA chair-bed - Creation of discharge report- Appointment by ward green jacket for dressings during 1–2 weeks and revision consultation in a month.- Appointment for surgeon's clinic.
The authors declare that no experiments were carried out on human beings or animals for this research.
Data confidentialityThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Please cite this article as: Delgado Velilla F, Mora Martínez JR. Implantación de un modelo de calidad basado en la ges-tión clínica por procesos en un Servicio de Cirugía Ortopédica y Traumatología. Rev Esp Cir Ortop Traumatol. 2012;56(1):80-93.