To determine the efficacy of growing rods in the treatment of early onset scoliosis.
Materials and methodsA total of 32 patients were treated using fusion techniques that included double growing rods and Vertical Expandable Prosthetic Titanium Ribs (VEPTR), in our Early Onset Scoliosis Centre between 2004 and 2011. After analyzing the clinical histories and X-rays, 20 patients were included due to meeting the inclusion criteria. All patients had previously received conservative treatment with cranial traction and a series of plasters/corsets.
The deformity was analyzed before and after the initial surgery, and in successive tightenings, using the X-rays of the coronal and sagittal planes by means of the Cobb angle, as well as the longitudinal and coronal growth of the thorax, and the growth of the spinal column. A series of 188 X-rays of 53 patients with cystic fibrosis were studied in order to perform a comparative analysis with the patients with early-onset scoliosis.
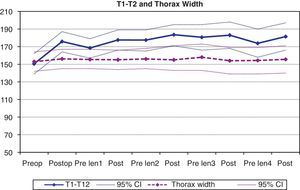
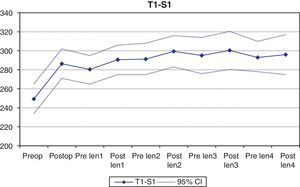
ResultsThere was significant improvement in the angle (Cobb and kyphosis) and linear parameters (T1-S1 distance, T1-T12 distance, and coronal width of the thorax) after the initial surgery, but the successive tightenings had a minimal beneficial effect, losing effectiveness over a period of time. The patients with early-onset scoliosis showed a lower growth of the thorax compared to the patients with cystic fibrosis.
DiscussionTreatment of early-onset scoliosis with expandable devices is mainly beneficial with the initial procedure and the first tightenings, but shows a loss of efficacy over a period time.
Determinar la eficacia de las barras de crecimiento en el tratamiento de la escoliosis de inicio precoz.
Material y métodoEntre 2004 y 2011, un total de 32 pacientes fueron intervenidos en nuestro centro de escoliosis de inicio precoz mediante técnicas sin fusión (barras de crecimiento dobles y VEPTR). De ellos, analizamos prospectivamente la historia clínica y las radiografías de 20 pacientes que cumplen los criterios de inclusión. Todos los pacientes habían recibido previamente tratamiento conservador con tracción craneal y yesos/corsés seriados.
En cada radiografía (preoperatoria y postoperatoria de la cirugía inicial y de los sucesivos retensados) analizamos la deformidad en los planos coronal y sagital mediante el ángulo de Cobb, el crecimiento longitudinal y coronal del tórax, y el crecimiento de la columna vertebral. Se estudian 188 radiografías de tórax seriadas de 53 pacientes con fibrosis quística para hacer un análisis comparativo con los pacientes con escoliosis de inicio precoz.
ResultadosLa mejora de los parámetros angulares (Cobb y cifosis) y lineales (distancia T1-S1, distancia T1-T12 y anchura coronal del tórax) fue significativa con la cirugía inicial, pero los sucesivos retensados tuvieron mínimo efecto beneficioso, perdiendo eficacia a lo largo del tiempo. Comparativamente con los pacientes con fibrosis quística, el crecimiento del tórax es menor en los pacientes con escoliosis de inicio precoz.
DiscusiónEl tratamiento de la escoliosis de inicio precoz con sistemas expansibles resulta beneficioso fundamentalmente en el procedimiento inicial y primeros retensados, demostrando una pérdida de eficacia a lo largo del tiempo.
Progressive spinal deformity at early ages represents a serious problem for the health of the patients and a challenge for the surgeon who is going to treat them. There are many causes of early-onset scoliosis: infantile and juvenile idiopathic scoliosis, congenital spinal deformities, neuromuscular problems or a heterogeneous group of syndromes.1
There is a group of curves in very young patients that do not progress or do so very slowly, or even resolve spontaneously. However, there is another group of patients in whom, despite series of orthotic/plaster treatments, the deformity can progress rapidly, making early surgical intervention necessary.
The progression of the deformity puts the life of the patient at risk.2 The lungs primarily develop during the first 8 years of a patient's life, so thoracic deformity secondary to scoliosis can affect pulmonary maturation negatively.3 The main effect of scoliosis on lung development is to inhibit growth of the alveoli and lung arterioles; this in turn causes the respiratory insufficiency observed in patients with early-onset scoliosis. In fact, a T1-T12 distance of less than 18cm in adults is associated with respiratory function less than 45% of the theoretical value.4,5
Spinal column growth is irregular throughout the growth period. The longitudinal growth of the spine peaks during the first 5 years of life, the T1-S1 distance increasing approximately 2cm a year; when the child is 5, the lumbar and thoracic spines have reached two-thirds of their total adult height. During the period from 5 to 10 years old, longitudinal growth is less, while the speed of growth again increases from 10 years old on. The scoliotic segments grow abnormally; fusionless techniques based on distraction will consequently allow the spine to continue growing, which is essential for respiratory and visceral development.6
Traditional techniques of non-surgical treatment for early-onset scoliosis include plasters, corsets, or a combination of both. Halo skull traction can be useful as a step prior to surgery or to plasters/corsets. This treatment with plasters and corset involves a great many complications such as skin ulcers or rib cage changes from pressure.7 In addition, it is often inefficient, given that as the rib cage is immature, it deforms before transmitting the corrective forces to the spinal column.4
The indications for surgical treatment in early-onset scoliosis are: progression of the spinal deformity despite orthopedic treatment, rib cage development/growth failure or worsening of respiratory insufficiency.4 There are 2 treatment options: techniques with or without fusion.
Spinal column fusion at early ages has serious repercussions on the adult patient, limiting patient stature and thoracic and pulmonary development.5
Non-fusion techniques include growing rods and the vertical expandable prosthetic titanium rib (VEPTR). The VEPTR is based on cephalic anchoring to the ribs and a distal one to a rib, spinal column or pelvis. It is indicated in cases of thoracic insufficiency syndrome.8 For growing rod mounting, conventional instrument systems are used, creating a double telescopic bar system using transversal or longitudinal connectors. These rods are directly anchored to the spinal column by pedicle screws or hooks, with an implant pull-out rate lower than that for the VEPTR.1 All the growing bars used with the patients included in our study were dual and were implanted following the technique described by Akbarnia et al.1 We used pedicle hooks and/or screws at both the caudal and cephalic levels and, at times, a transversal connector at the ends, with decortication and placement of local allograft at only the cephalic and caudal anchor points.
The objective of this study was to evaluate the efficacy of dual growing rods in controlling the deformity and allowing thorax and spinal column growth in early-onset scoliosis.
Materials and methodsBetween 2004 and 2011, a total of 32 consecutive patients were operated on for early-onset scoliosis using techniques without fusion (dual growing rods or VEPTR) in our center. From these patients, we prospectively analyzed the clinical histories, surgical protocols successive X-rays of 20 of them that fulfilled the inclusion criteria. Among these criteria were the following:
- •
Patients with early-onset scoliosis treated with non-fusion dual growing rods.
- •
Have 3 or more operations (initial surgery and at least 2 tightenings).
- •
Absence of systemic complications to eliminate them from the non-fusion rod program: late implant infections, problems related to the base disease, etc.
- •
Absence of diffuse complex congenital anomalies in the spine.
In the review of the case history, we gathered information on the diagnosis, sex, age at commencement of treatment with expansible systems, total number of lengthening procedures and interval between them.
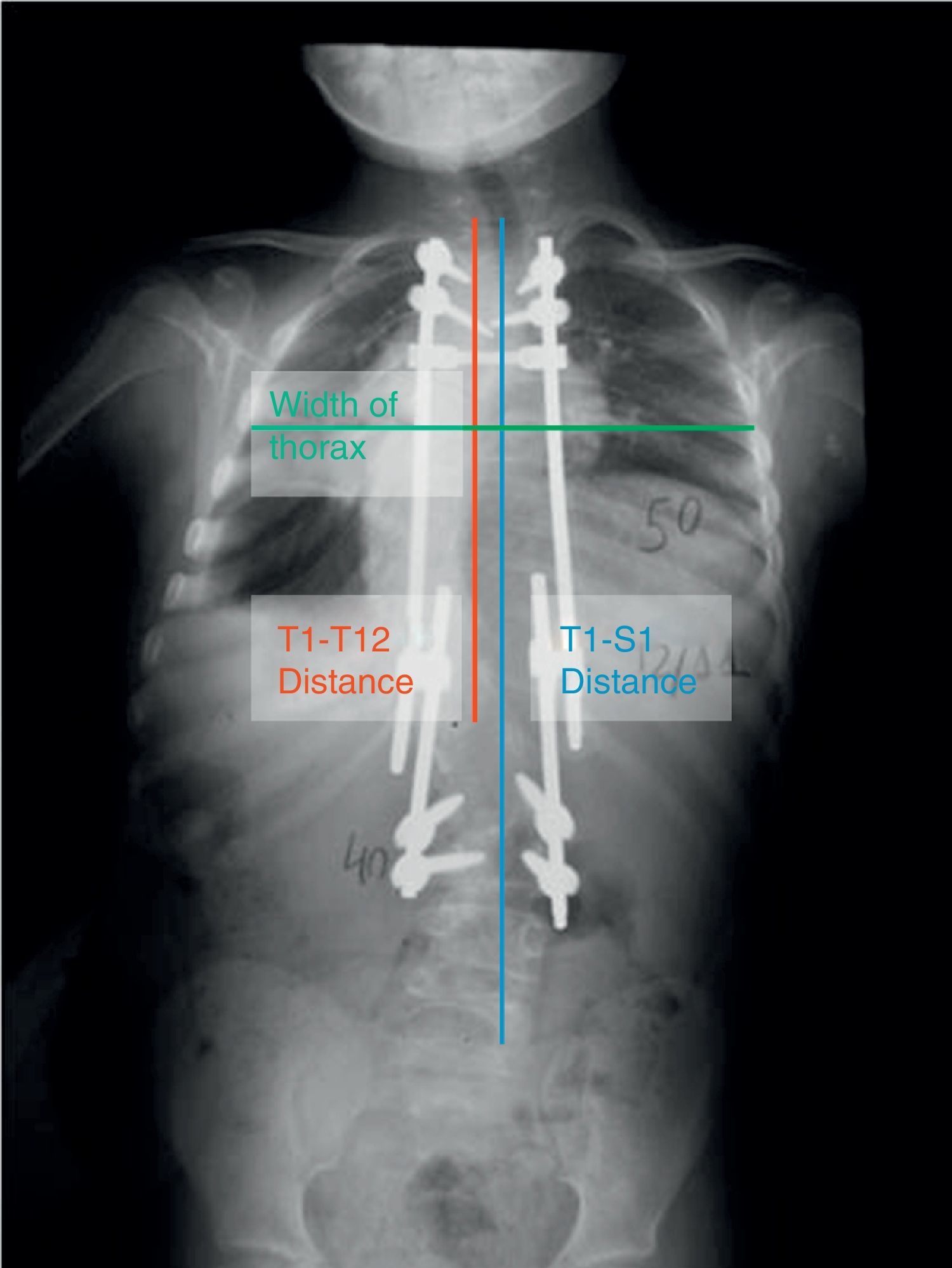
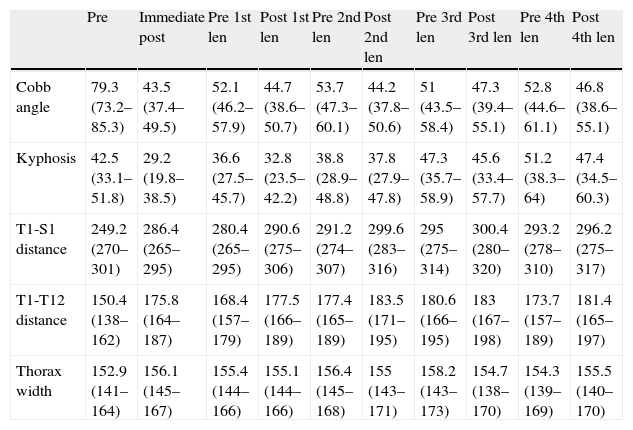
We carried out a prospective analysis of the patient X-rays (teleradiography images of the entire spine in standing position in the anterior–posterior and lateral planes) in the preoperative and immediate postoperative periods, along with before and after each tightening procedure. In each X-ray, we analyzed the T1-T12 distance and the coronal thorax width at T6 to study the growth of the chest; we registered the T1-S1 distance (Fig. 1) to evaluate the growth of the spinal column; and, to analyze the correction of the deformity, we recorded the angle of the main curve using the Cobb technique in the coronal plane and the overall T2-T12 kyphosis in the sagittal plane. All the X-rays were calibrated. In addition, we performed a comparative analysis of longitudinal chest growth in the patients with early-onset scoliosis who underwent growing rod treatment with respect to a control group. To establish the control group, we retrospectively analyzed 188 serial verification X-rays from 53 patients diagnosed with cystic fibrosis, on whom the T1-T12 distance was recorded. These patients, a priori, lacked any specific disorder in the growth of the spinal column/thorax, and underwent regular serial X-ray controls of the thorax by the pediatric pulmonology service.
Anterior–posterior teleradiography of a patient with early-onset scoliosis in treatment with dual growing rods. You can see the T1-T12 distance (the vertical line that joins the upper endplate of T1 with the lower endplate of T12), the T1-S1 distance (the vertical line that joins the upper endplate of T1 with the upper border of S1), and the coronal anchor of the thorax at the level of T6.
We performed the statistical analysis with the statistical SAS package for mixed models, using the Friedman test for analyzing repeated measures of nonparametric continuous data. Statistical significance was set to a P value less than 0.05.
ResultsA total of 20 patients fulfilled the criteria for inclusion. From among the patients operated on in our center, 8 failed to fulfill the criteria for inclusion. These 8 included 2 patients with neuromuscular scoliosis from myelomeningocele that presented late implant infection, which forced us to retire the implants, 1 patient that died as a result of the base disease (neurofibromatosis), and 5 patients that failed to reach a minimum follow-up of at least 3 operations (initial surgery and a minimum of 2 tightening procedures). Patients with fewer than 2 tightening procedures were excluded from the study, given that its objective was to analyze the efficacy of the growing rods in controlling the deformity and permitting vertebral and thoracic growth over time.
The diagnoses included infantile idiopathic scoliosis in 10 patients, neuromuscular scoliosis in 6 cases, and congenital or thoracogenic scoliosis in 4. All the patients had previously received conservative treatment with cranial traction and serial plasters/corsets. We lack a specific guideline for establishing the indication for surgical treatment, but the program with growing rods is generally initiated when it is impossible to control the deformity with the orthopedic treatment or when complications associated with the treatment with plasters/corsets appear (skin ulcers or modeling of the chest wall).
All patients had been diagnosed with scoliosis before they were 5 years old; 13 were girls and 7 were boys. The mean age at the moment of the initial surgery was 6.8 years (range: 45–118 months).
Mean follow-up was 44 months (range: 23–107), with an average of 4 tightening procedures (range: 2–7) per patient. The mean interval between tightening procedures was 9.1 months. The interval between tightening periods was not standardized and varied depending on the progression of the deformity during follow-up. There were no significant differences in the number of tightenings in the different groups diagnosed.
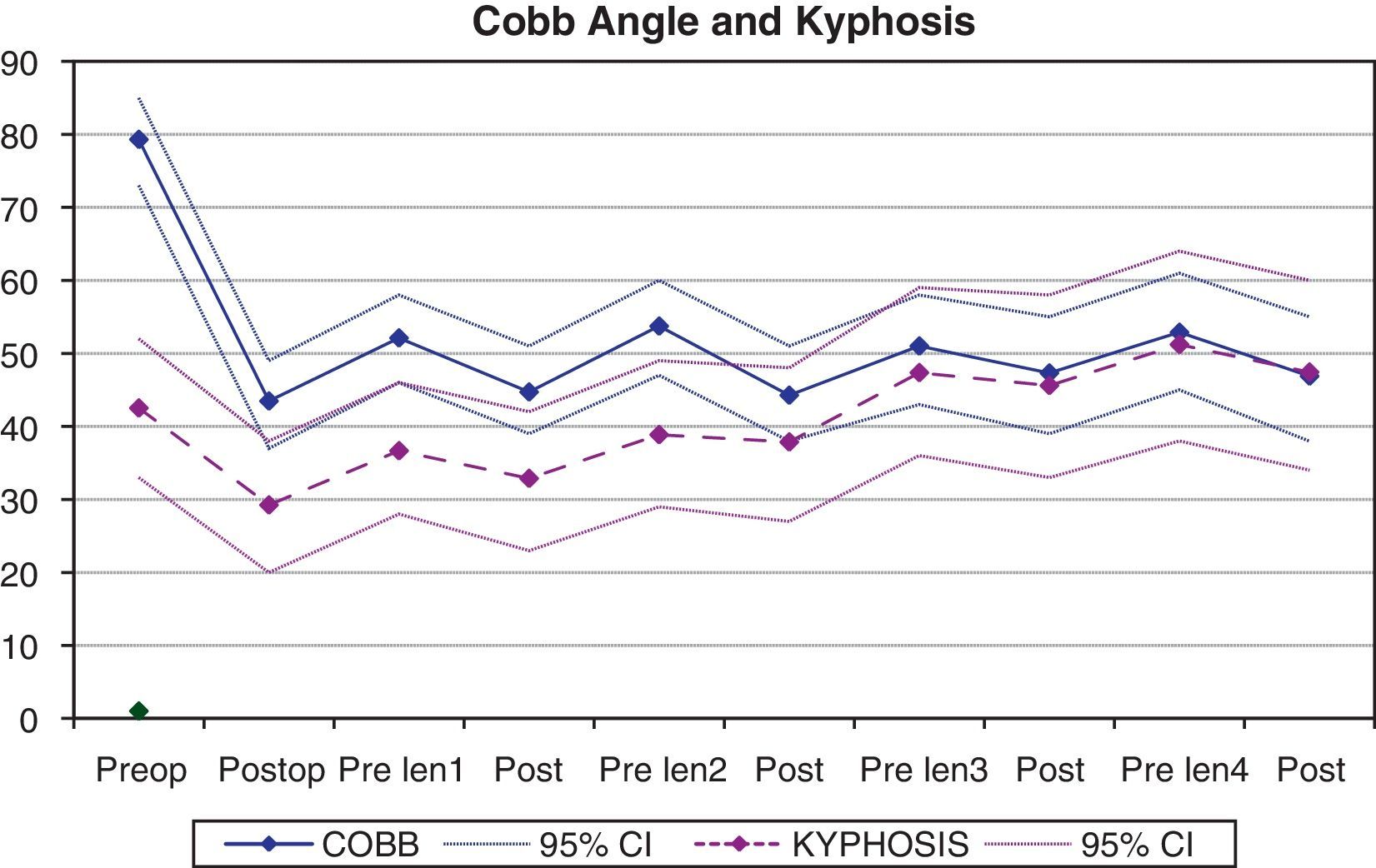
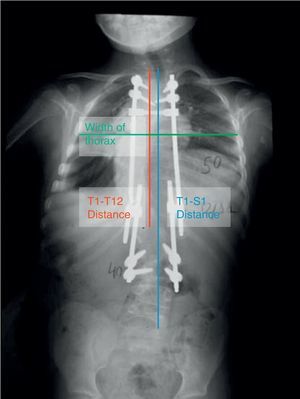
Correction of the deformityThe angular value of the scoliosis measured using the Cobb angle improved from a mean value of 79.3° (IC 95%: 73.2–85.3) in the preoperative measurement to 43.2° (IC 95%: 37.4–49.5) in the immediate postoperative period, which represented a 45% correction (P=.0001) (Table 1). During follow-up we could see a worsening of the deformity between the successive tightening procedures, which the lengthening surgery partially corrected, although the statistical analysis showed that the Cobb angle failed to change significantly with the tightening procedures. It is noteworthy that the successive tightening procedures became less and less efficient, and that the angle of deformity increased slightly each time (Fig. 2), showing a mean Cobb angle value of 46.8° (38.6–55.1°) after the 4th tightening procedure.
Mean values and 95% intervals of confidence for the Cobb angle, overall kyphosis, T1-S1 distance, T1-T12 distance, and coronal thorax width at the initial preoperative and immediate postoperative moments, as well as before and after each lengthening procedure.
| Pre | Immediate post | Pre 1st len | Post 1st len | Pre 2nd len | Post 2nd len | Pre 3rd len | Post 3rd len | Pre 4th len | Post 4th len | |
| Cobb angle | 79.3 (73.2–85.3) | 43.5 (37.4–49.5) | 52.1 (46.2–57.9) | 44.7 (38.6–50.7) | 53.7 (47.3–60.1) | 44.2 (37.8–50.6) | 51 (43.5–58.4) | 47.3 (39.4–55.1) | 52.8 (44.6–61.1) | 46.8 (38.6–55.1) |
| Kyphosis | 42.5 (33.1–51.8) | 29.2 (19.8–38.5) | 36.6 (27.5–45.7) | 32.8 (23.5–42.2) | 38.8 (28.9–48.8) | 37.8 (27.9–47.8) | 47.3 (35.7–58.9) | 45.6 (33.4–57.7) | 51.2 (38.3–64) | 47.4 (34.5–60.3) |
| T1-S1 distance | 249.2 (270–301) | 286.4 (265–295) | 280.4 (265–295) | 290.6 (275–306) | 291.2 (274–307) | 299.6 (283–316) | 295 (275–314) | 300.4 (280–320) | 293.2 (278–310) | 296.2 (275–317) |
| T1-T12 distance | 150.4 (138–162) | 175.8 (164–187) | 168.4 (157–179) | 177.5 (166–189) | 177.4 (165–189) | 183.5 (171–195) | 180.6 (166–195) | 183 (167–198) | 173.7 (157–189) | 181.4 (165–197) |
| Thorax width | 152.9 (141–164) | 156.1 (145–167) | 155.4 (144–166) | 155.1 (144–166) | 156.4 (145–168) | 155 (143–171) | 158.2 (143–173) | 154.7 (138–170) | 154.3 (139–169) | 155.5 (140–170) |
Values are shown through the fourth lengthening procedure. Angle values are expressed in degrees and lineal values in millimeters.
Post: postoperative; Pre: preoperative; len: lengthening.
The angle of overall T2-T12 kyphosis showed a mean correction of 31.3% with the initial surgery (mean overall preoperative kyphosis: 42.5°; mean overall postoperative kyphosis: 29.2°) (P=.001). During follow-up we observed a progressive increase in kyphosis, which was especially significant after the 2nd tightening procedure (Fig. 2), reaching a mean overall kyphosis value of 47.4° just before the 4th tightening procedure. In addition, the ability to correct the kyphosis with the successive tightening procedures gradually decreased during treatment.
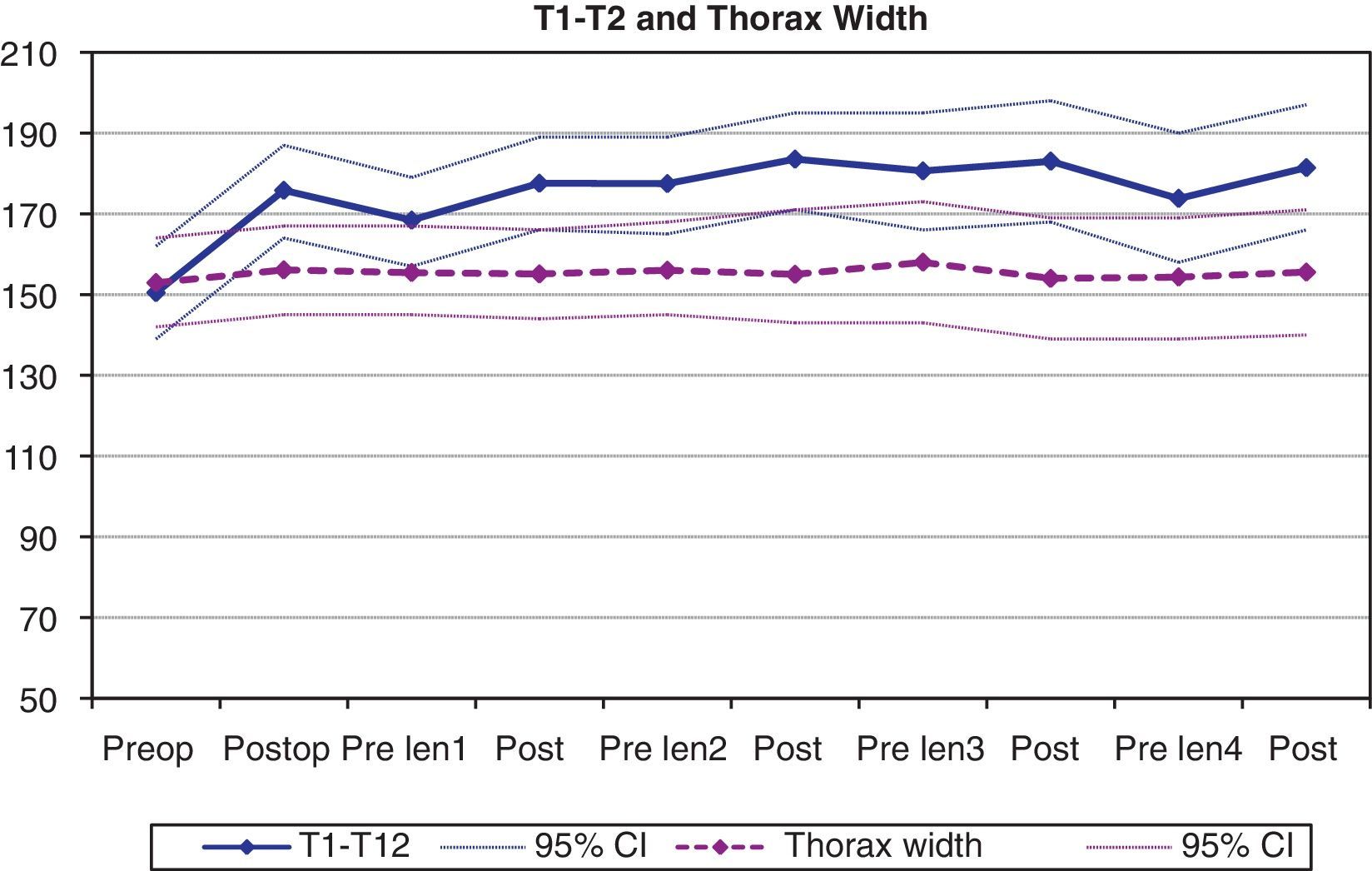
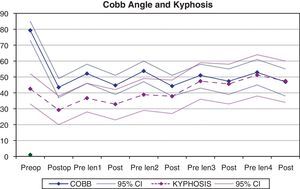
Chest growthThe longitudinal growth of the thorax, analyzed using the T1-T12 distance, showed a mean increase of 25.4mm from the initial surgery (from a mean preoperative value of 150.4mm to 175.8mm after the initial operation) (P<.01). During the treatment period, a gradual increase in this distance was observed, reaching a mean value of 181.4mm following the 4th tightening procedure (Fig. 3). Consequently, the mean longitudinal growth of the chest after 4 tightening procedures was 31mm. This translates to an annual increase in the T1-T12 distance of 8.6mm. The growth of the thorax in the coronal plane showed a mean increase of 3.2mm from the initial surgery; this remained constant during the follow-up, so the chest width after the 4th tightening procedure was similar to that observed in the initial postoperative exam. There were no statistically significant differences in the values of the coronal width of the thorax throughout the follow-up.
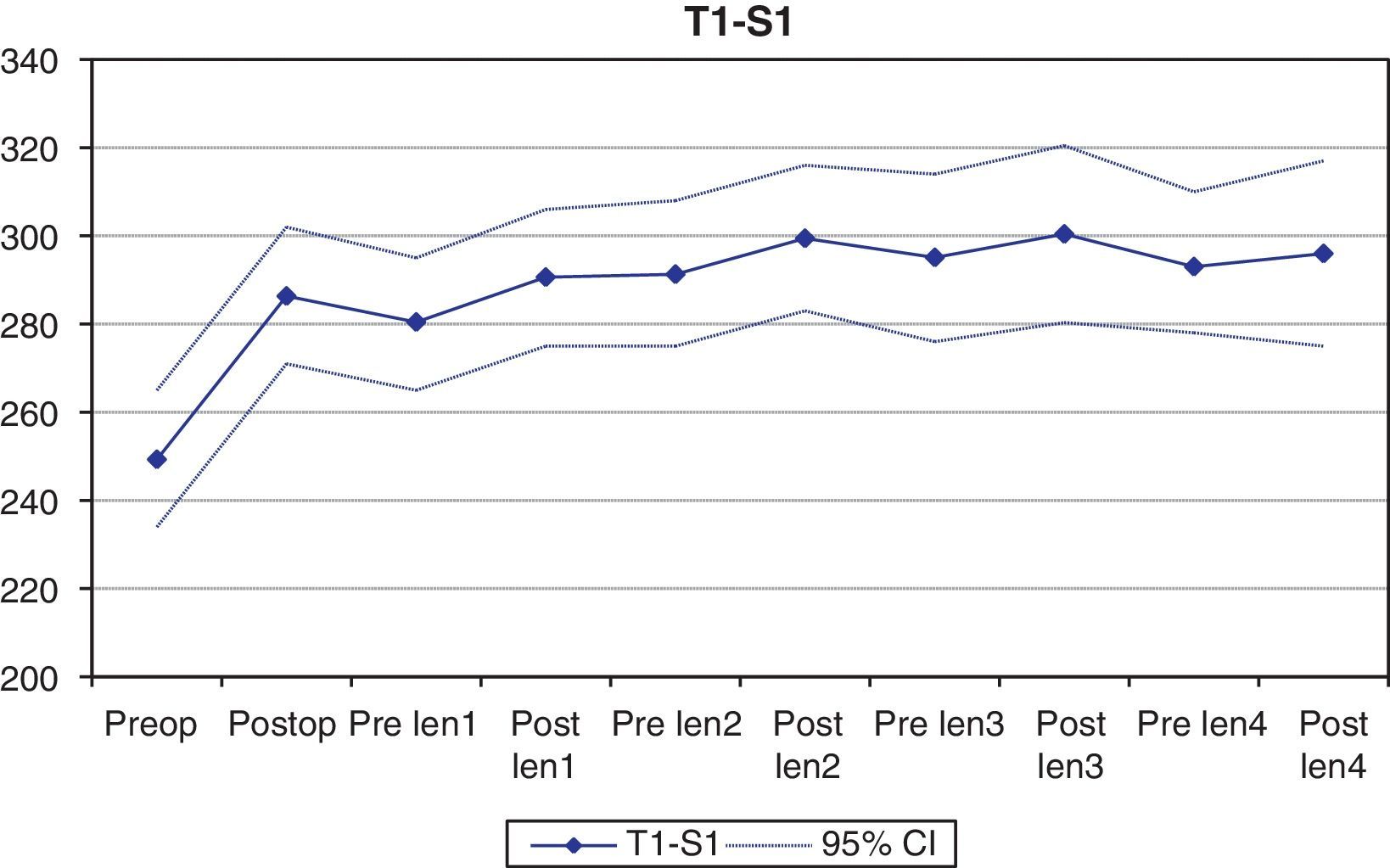
Spinal column growthSpinal column length, calculated using the T1-S1 distance in the coronal plane, increased a mean of 37.2mm from the initial surgery (from a mean preoperative value of 249.2mm to 286.4mm following the placement of the growing rods) (P<.001), in direct relation with the correction of the deformity. During follow-up, the spinal column increased only 9.8mm, reaching a mean value of 296.2mm after the 4th tightening procedure (Fig. 4).
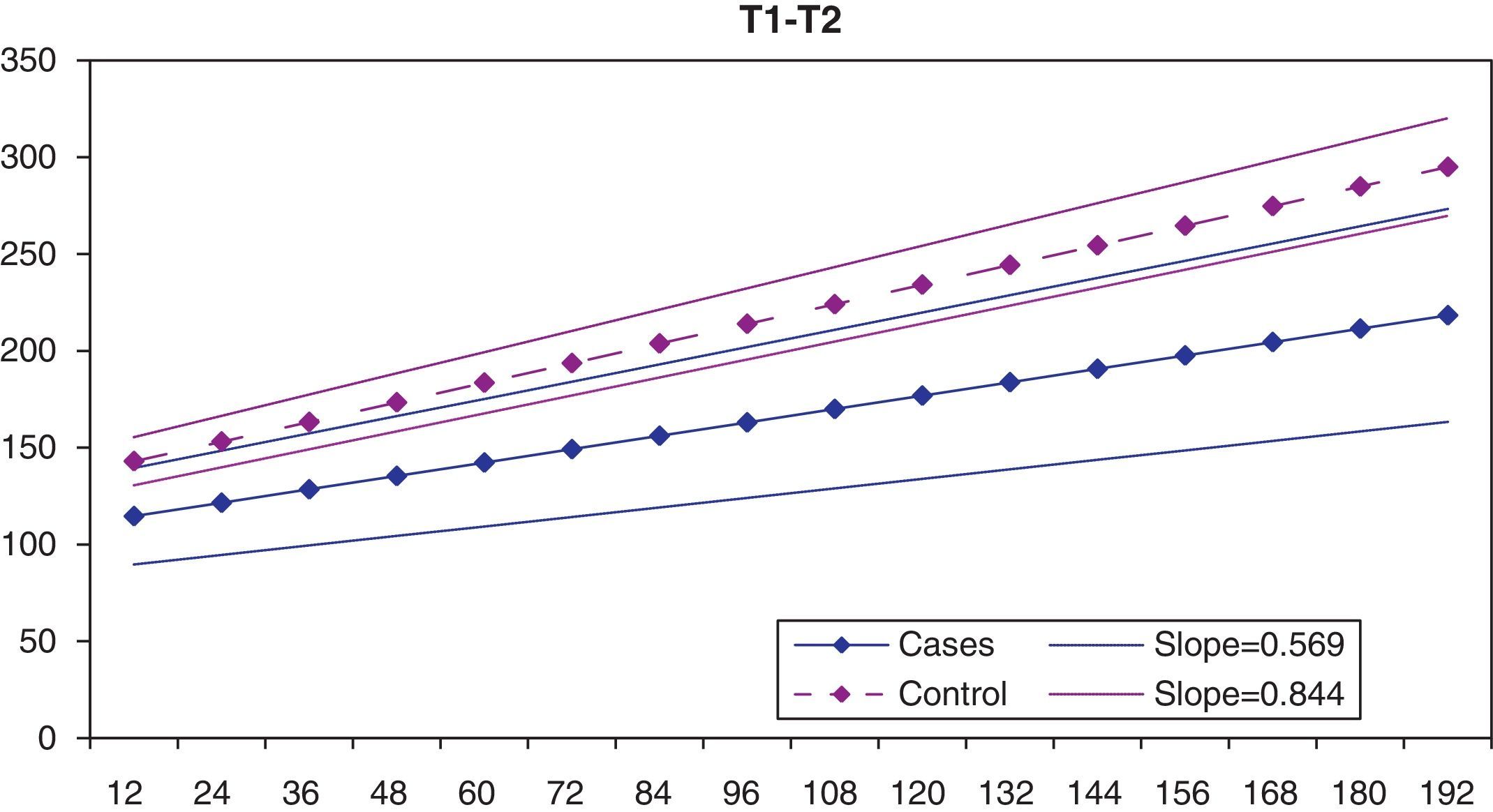
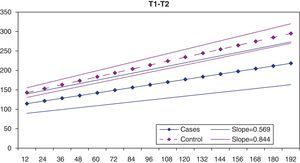
Comparative analysis with the control groupGiven that we cannot perform serial chest X-rays on healthy children because of the harmful effects of X-rays,9,10 we turned to the records of patients with cystic fibrosis in the Pediatric Pulmonology Service at the Hospital La Paz. Patients with cystic fibrosis, a priori, have no disorders in the growth of the spinal column or thorax. In our institution, there is no protocol establishing X-rays at specific ages in patients with cystic fibrosis; X-rays are taken based on each patient's clinical picture. This prevents us from obtaining serial X-rays for all the patients at the same age. Consequently, we estimated the T1-T12 distance in our statistical analysis depending on the age, both for the control group of patients with cystic fibrosis and for the patients with early-onset scoliosis included in this study.
In the graph of the statistical estimate for T1-T12 distance based on age, it can be seen that the speed of the longitudinal chest growth is significantly greater in the control group (patients with cystic fibrosis) than in the group of patients with early-onset scoliosis (Fig. 5). The slope of the lineal representation of chest dimensions based on age is 0.844 in the control group and only 0.569 in the group with scoliosis. This difference in slope is shown in that the difference in T1-T12 distance between the two groups is greater the older the patients are.
DiscussionFusionless instrumentation for the treatment of early-onset scoliosis has been used since the introduction of Harrington instrumentation in the 1960s.11 Initially, set-ups with a single rod were used; dual set-ups became more popular later, improving the results in comparison with single-rod assemblies.1,12 Various studies have shown that dual growing rods are effective in controlling the vertebral deformity and in promoting the growth of the immature spinal column. In one of these studies, Thompson et al.12 observed an increase in the T1-S1 distance of 1.1cm a year from the initial instrumentation to the final fusion; the Cobb angle improved from 92° to 39° with the initial surgery but improvement of the angular value was modest during the successive lengthening procedures.
Akbarnia et al.1 published results with dual growing rods in 23 patients with early-onset scoliosis having at least 2 years of follow-up. They observed an initial-surgery correction of the Cobb angle to 44° (from 82° preoperatively to 38° in the immediate postoperative period); however, during follow-up the value of the Cobb angle remained stable, with a mean of 36° after the final fusion. The T1-S1 distance increased 50mm with the initial surgery (from 230mm to 280mm), while at the end of follow-up it was a mean of 326mm, with an annual increase of 10mm.
In our series, the initial correction of the Cobb angle was a mean of 36.1°, significantly less than that observed in the 2 prior studies. An explanation for these poorer results is that our group carries out a prior period of treatment with cranial traction using distraction halo and corsets that is more aggressive than that used in the previous groups; for that reason, we achieved a large part of the correction during this stage of orthopedic treatment. Proof of this is the fact that the mean value of the preoperative Cobb angle in our series is significantly smaller (mean of 79.3°) than in the Thompson (mean of 92°)12 and Akbarnia (mean of 82°)1 studies. In contrast, the value of the Cobb angle after the initial rod placement surgery is similar in the 3 studies (43°, 39°, and 38°, respectively).
An aspect of our study we would like to emphasize is the analysis of the sagittal plane, which has not been studied in the earlier works of Thompson and Akbarnia. The tendency of the spinal column treated with growing rods toward progressive kyphosis is significant. In our series, the mean angle of preoperative kyphosis is 42.5°, which corrects up to a mean of 29.2° with the initial surgery. However, a progressive increase in kyphosis occurs during follow-up, reaching a mean of 47.4° after the 4th tightening procedure. This kyphosis might be associated with complications, such as the implants in the cephalic area pulling out and the suprainstrumentation kyphosis that often makes unplanned operations necessary.
The longitudinal growth of the thorax (T1-T12 distance) and of the spinal column (T1-S1 distance) follows a similar tendency. In the case of the T1-T12 distance, the initial surgery achieves a mean increase of 25.4mm. The T1-S1 distance undergoes a mean increase of 37.2mm with the implantation of the growing rods, and of 9.6mm during the successive lengthening procedures. The limited gain in T1-S1 distance during the posterior tightening procedures is notable. One explanation for this finding might be that the increase in overall kyphosis during follow-up would cause a smaller measurement of the T1-S1 distance in the anterior–posterior X-ray.
To compare the growth of the thorax with respect to a control group, we turned to a group of patients who receive serial chest X-rays due to their underlying disease, patients with cystic fibrosis. These patients do not, a priori, present alterations in spinal column development. We cannot consider these patients as a healthy control group, but it would be unethical to give a healthy population periodic serial X-rays to establish a control group, due to the damaging effects of the X-rays.9,10 Even with the limitation represented by using these patients with cystic fibrosis as our control group, it is striking that chest growth is significantly smaller in the patients with early-onset scoliosis, which affects respiratory function: Karol5 observed that an excessively short thorax with a T1-T12 distance less than 18cm was associated with a lung function less than 45% of the theoretical function expected. Given that not all the X-rays were taken at the same age in all the patients, we statistically estimated the curve of the longitudinal thorax growth depending on age in the early-onset scoliosis group and in the control group, based on the specific T1-T12 distance values obtained at different ages.
Our results are significant for various reasons. On the one hand, they serve to warn the orthopedic community that we should not expect great correction of the deformity with successive lengthening procedures, especially in patients who have received multiple tightening procedures; and that applying excessive force during the distraction procedure could lead to implant breakage or dislodgement. In the second place, knowing that successive tightening procedures gradually lose their effectiveness over time leads us to consider delaying commencement of instrumentation as long as possible. Reviewing patients included in the Growing Spine Study Group database, Bess et al.13 showed that the risk of complications from treatment with growing rods dropped 13% for each additional year of patient age at the moment of beginning with surgical treatment; and that the risk of complications rose 24% with each additional surgical procedure performed. The results of the Bess et al. study13 taken together with the results from our study can help convince surgeons to delay the moment of initiating treatment with growing rods as much as possible (achieving a balance between deformity and age; that is, trying to implant the growing rods at the oldest possible age, as long as the deformity remains controlled). It might even convince them to stop after a few tightening procedures when the gains would be minimal.
A possible reason why successive tightening procedures lose efficacy is the increase in the rigidity or even the self-fusion of the immature spinal column during treatment with expendable systems. In fact, it is normal for a surgeon who is going to perform the final vertebral arthrodesis after a period of growing rods to observe that the segment of the previously instrumented column is extremely rigid, with areas of vertebral fusion. Although attempts have been made to prevent autofusion of the column (such as placing the rods subperiostically to avoid having to widely dissect the spine), these have been insufficient. It is also possible that the long period of immobilization of the spinal column in the instrumented segment plays a part in favoring increased rigidity.
As in previous studies, in our series we have found that the improvement in the deformity is produced fundamentally with the initial surgery. After the growing rods are implanted, no significant change in the Cobb angle is seen. In addition, if we analyze the sagittal plane, we see that an important reduction in kyphosis is achieved with the primary surgery, but that the spinal kyphosis gradually increases throughout follow-up.
There are several limitations in our study: first of all, the patient sample was heterogeneous (10 cases of idiopathic scoliosis, 6 of neuromuscular scoliosis and 4 of congenital/thoracogenic scoliosis); however, this is an infrequent disorder and our center is one of those with greatest national experience in the treatment of this type of patients. Another study limitation is that it was retrospective.
One study disadvantage is that we used only direct measurement on the X-rays to evaluate the distances. As has been seen in our study, the spinal column kyphosis gradually becomes more and more throughout follow-up, which produces error in the true measurement of the T1-S1 and T1-T12 distances (their measurement is standardized on the anterior–posterior X-ray). It is possible that determining such distances in the lateral X-ray or using diagnostic tests that provide a three-dimensional view would make this error smaller.
In conclusion, we can say that the moment at which the spines of patients with early-onset scoliosis submitted to expandable techniques are in the best condition is precisely after the primary surgery. The main correction of the angular values of the deformity, along with the greatest increase in the dimensions of the thorax and the spinal column, are reached after the initial surgery. The successive tightening procedures gradually lose efficacy over time. Comparing against patients with cystic fibrosis, patients with early-onset scoliosis have less longitudinal growth in the thorax.
Level of evidenceLevel of evidence 3.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments on human beings or on animals took place in this research.
Data confidentialityThe authors declare that they followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participating in this study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflicts of interests to declare.
Please cite this article as: Sánchez Márquez JM, et al. Barras de crecimiento en escoliosis de inicio precoz ¿Permiten realmente el control de la deformidad y el crecimiento vertebral y torácico? Rev Esp Cir Ortop Traumatol. 2013;57:178–85.