The objective is to establish the duration of our interventions, intermediate times and surgical performance. This will create a virtual waiting list to apply a mathematical programme that performs programming with maximum performance.
Material and methodsRetrospective review of 49 surgical sessions obtaining the delay in start time, intermediate time and surgical performance. Retrospective review of 4045 interventions performed in the last 3 years to obtain the average duration of each type of surgery. Creation of a virtual waiting list of 700 patients in order to perform virtual programming through the MIQCP-P until achieving optimal performance.
ResultsOur surgical performance with manual programming was 75.9%, ending 22.4% later than 3pm. The performance in the days without suspensions was 78.4%. The delay at start time was 9.7min.
The optimum performance was 77.5% with a confidence of finishing before 15h of 80.6%. The waiting list has been scheduled in 254 sessions.
DiscussionOur manual surgical performance without suspensions (78.4%) was superior to the optimal (77.5%), generating days finished later than 3pm and suspensions. The possibilities for improvement are to achieve punctuality at the start time and adjust the schedule to the ideal performance.
The virtual programming has allowed us to obtain our ideal performance and to establish the number of operating rooms necessary to solve the waiting list created.
ConclusionsThe data obtained in virtual mathematical programming are reliable enough to implement this model with guarantees.
El objetivo es conocer la duración de nuestras intervenciones, tiempos intermedios y rendimiento quirúrgico. Con ello elaborar una lista de espera virtual para aplicar un programa matemático que realice la programación con rendimiento idóneo máximo.
Material y métodosRevisión retrospectiva de 49 sesiones quirúrgicas obteniendo el retraso en la hora de comienzo, el tiempo intermedio y el rendimiento quirúrgico. Revisión retrospectiva de 4.045 intervenciones realizadas en los 3 últimos años para obtener la duración media de cada tipo de cirugía. Elaboración de una lista de espera virtual de 700 pacientes para realizar programaciones virtuales mediante el MIQCP-P hasta obtener el rendimiento óptimo.
ResultadosNuestro rendimiento quirúrgico con programación manual es del 75,9%, finalizando el 22,4% más tarde de las 15h. El rendimiento en las jornadas sin suspensiones es del 78,4%. El retraso en la hora de comienzo es de 9,7min.
El rendimiento óptimo es del 77,5%, con una confianza de terminar antes de las 15h del 80,6%. La lista de espera se ha programado en 254 sesiones.
DiscusiónNuestro rendimiento quirúrgico manual sin suspensiones (78,4%) es superior al idóneo (77,5%) generando jornadas finalizadas más tarde de las 15h y suspensiones. Las posibilidades de mejora son lograr la puntualidad en la hora de comienzo y ajustar la programación al rendimiento idóneo.
La programación virtual nos ha permitido obtener nuestro rendimiento idóneo y conocer el número de quirófanos necesarios para resolver la lista de espera creada.
ConclusionesLos datos obtenidos en la programación matemática virtual son lo suficientemente fiables como para implantar este modelo con garantías.
The progressive ageing of the general population will inexorably entail an increase in pathologies derived from this ageing, and the fact our health system must adapt to this increase. Orthopaedic and trauma surgery, our speciality, is possibly one of the most affected. Over recent years there has been an exponential increase in the number of fractures derived from ageing and degenerative joint pathology, especially of the lower limb. This factor, together with progress and medical technology advances offering further surgical options with good outcomes has led to an enormous demand for surgery in our speciality, both emergency and scheduled. Waiting lists are difficult to resolve due to high health costs and obtaining the proportional increases of necessary resources to resolve this problem of today.1 Appropriate management of waiting lists is crucial, not just from a patient's health point of view, but also regarding other socio sanitary aspects, since this underlines a misalignment between the social sanitary demand and the offer which the state provides. The resolution of the waiting lists depends more than the number itself of patients included, of the assignation of resources and not so much their direct increase but correct and appropriate management.1,2
Operating rooms are the most costly of all resources, and are the most limited, as they become the bottle-neck in the process,3,4 which is why it is essential to obtain maximum performance from them. A reduction in costs per process also forms part of appropriate management and planning, as does a reduction in patients on the waiting list for operations.4 At present the programming of each day in surgery is carried out manually, empirically and subjectively, with time in surgery being presupposed based on the experience of the service, which carries out the programming and hospital habits and characteristics.
The performance or use of an operating room is measured by its rate of occupation, which is the ratio between the time available and the real time in which it is occupied by a patient. However, ideal performance of an operating room has not been defined, on the understanding that the higher its occupation rate, the better the management as this indicates more patients have been operated on that day and the resource has been maintained active for longer. However, this may mean a prolongation of the working day which may lead to friction, conflicts and a problem in compensating for the activity outside working hours.5
The performance of an operating room depends on the time the operations begin and their duration. Time in surgery has to include the time of anaesthesia, surgery and the time between operations, i.e. cleaning and preparing the operating room between one operation and the next. Many factors need to be taken into consideration when programming surgery, some of which are difficult to control and also little known or studied, which explains why they are difficult. Appropriate occupation rates from 75% to 90% have been published, both very different, using often ill-defined methodologies for the purpose which vary from one hospital to another.1,5 Surgical performance figures are a constant bone of contention between managers and surgeons. Excessive pressure may lead to a reduction in healthcare quality and even in patient safety.5
There were several objectives involved in this study: to determine our time in surgery for each process, time between interventions and current performance of our operating theatres. With this data and using a mathematical programme, we created a virtual waiting list which took into account variables such as intervention and duration time between interventions. As a result we were able to undertake a simulation of programming of the most appropriate patients in our operating rooms so as to determine what the ideal performance or occupation rate was, with the final objective being for this created virtual model to be exportable for surgical programming usage in any hospital and speciality.
Material and methodsRetrospective reviewOur service is located in a tertiary university hospital and it is a service with teaching credentials, autonomy, a benchmark for other hospitals which treats all types of orthopaedic and trauma pathologies included in the locomotor system. We retrospectively reviewed surgical activity during the month of October 2016 (49 sessions) in daily operating theatres during the morning in orthopaedic surgery, obtaining the data from the Management Department of our hospital and also from the obligatory surgery register. We did not include trauma pathology surgery in this study, because of it being urgent and not being included on a waiting list, which leads to different problems. We evaluated the functioning of each operating theatre from 8.30am to 3h pm, i.e. 390min in each day, except Fridays where we began at 9.00h and because the clinical sessions were longer in the surgical services.
Using this data we studied the delay in starting time from that programmed, the time between operations from when one patient came out to when the next went in, the time when the programme ended when the last patient programmed came out, and the number of suspended operations. We studied two rates of occupation or surgical performance in each session. The Q1, which considers the occupation of the operating theatre by exclusive evaluation the duration of interventions without taking into consideration time between them, which is how the occupation rate of the operating theatre is assessed in our hospital and Q2, which evaluates the occupation of the operating theatre from when the first patient enters until the last exits. We also studied the days when operations ran over time after 3h pm and those which would have finished later than 3h pm discounting the time of delay in when they began.
Virtual waiting listWe also retrospectively reviewed 4045 orthopaedic operations performed consecutively in our service during the last 3 years to obtain the mean duration of each type of surgical intervention, considering the duration from when the patient entered the operating theatre until he exited from it. This data was considered in 146 types of different operations as the variable with a mean value and standard deviation, not considering differences between the different surgeons and surgeons and anaesthesiologists.
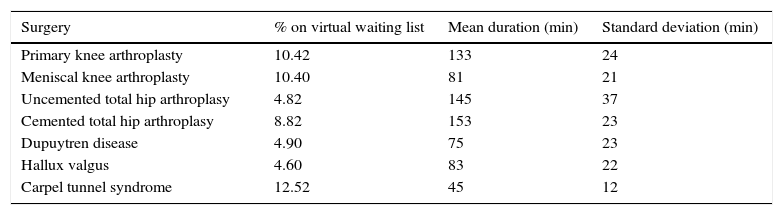
Once these data were obtained we created a virtual waiting list of 700 patients by calculating the probability of each pathology appearing on the list depending on its frequency in the 4045 reviewed orthopaedic surgical interventions. The most prevalent operations on the list are those included in Table 1. These 7 interventions are by their frequency 56.48% of the list. Oncology surgery was excluded due to its variability in time in surgery and its infrequent inclusion on waiting lists, since it is governed by different criteria marked by the tumour committees. The virtual patients were included on the list randomly with 3 types of priority [maximum (3), mean (2) and minimum (1)] and a specific age. Using the MIQCP-P (Mixed Integer Quadratic Constrain Programming) mathematical programme, we performed several surgical programming processes from the list created with different operating theatre occupation rates (Q1). These ranged from 70% to 85%, seeking optimum performance, i.e. maximum occupation of the day with a minimum confidence level of 75% and a mean always above 80% of terminating the surgical programme before 3h pm. This confidence level was calculated in accordance with statistical concepts based on normal distribution, since all variables studied (duration of operating, delay in starting and time between operations) were considered as normal distribution. The programming was carried out using a mathematical programme taking the following into consideration: age, priority, duration of operations, mean delay in start time and dead time between operations. This programming was designed by giving the oldest patient 10 points and the most recent 0 points, with the other patients having a percentage score in accordance with this. With respect to priory, minimal priority (1) was 0 points, intermediate priority (2) 5 points and maximum priority (3) 10 points. With these scores and a weight of 70% given to age, and 30% to priority, all the patients on the waiting list were ordered according to scores.
Most common surgical interventions included in the created virtual waiting list.
| Surgery | % on virtual waiting list | Mean duration (min) | Standard deviation (min) |
|---|---|---|---|
| Primary knee arthroplasty | 10.42 | 133 | 24 |
| Meniscal knee arthroplasty | 10.40 | 81 | 21 |
| Uncemented total hip arthroplasy | 4.82 | 145 | 37 |
| Cemented total hip arthroplasy | 8.82 | 153 | 23 |
| Dupuytren disease | 4.90 | 75 | 23 |
| Hallux valgus | 4.60 | 83 | 22 |
| Carpel tunnel syndrome | 12.52 | 45 | 12 |
With these programming criteria we determined the optimum performance of surgical sessions, i.e. their maximum occupation with a guarantee at terminating the programming before 3h pm and with this optimum performance, the number of surgical sessions necessary for operating on the 700 patients on the virtual waiting list.
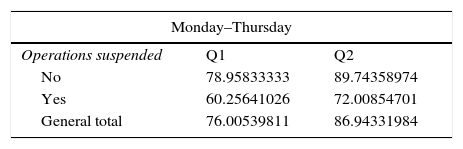
ResultsRetrospective review153153 operations were programmed for the 49 surgical sessions carried out in the month of October 2016. Performance or occupation of time in surgery was Monday to Thursday at 76.0% in Q1 and 86.9% in Q2, highlighting that when the suspension of a surgical intervention occurred, performance dropped to 60% and 72%, respectively, since the patient was not replaced. On Fridays, surgical performance was 75.9% in Q1 and 87.7% in Q2. Globally, without differentiating between different days of the week, our surgical performance was 75.98% in Q1 and 87.12% in Q2 (Table 2). The remainder of the time in Q1 is the time of delay in starting the intervention, the time between interventions and the time from when the last patient exited up to 15.00h, which is the end of the available operating theatre time. If the suspended interventions were not accounted for, and only those sessions where no operation was suspended are reviewed, our overall performance of Q1 was 78.4% (Table 2).
Surgical performance.
| Monday–Thursday | ||
|---|---|---|
| Operations suspended | Q1 | Q2 |
| No | 78.95833333 | 89.74358974 |
| Yes | 60.25641026 | 72.00854701 |
| General total | 76.00539811 | 86.94331984 |
| Friday | ||
|---|---|---|
| Operations suspended | Q1 | Q2 |
| No | 76.0493827 | 87.96296296 |
| Yes | 72.91666667 | 86.80555556 |
| General total | 75.93434343 | 87.75252525 |
| General | ||
|---|---|---|
| Operations suspended | Q1 | Q2 |
| No | 78.44173442 | 89.35272045 |
| Yes | 63.42147436 | 75.70779915 |
| General total | 75.98944706 | 87.1249782 |
With regard to suspensions of an operation, there were 8 over the month, which indicates that in 16.3% of surgical working days some type of suspension occurs, 7 of which presuppose will finish later than 3h pm. It comes to our attention that the suspension occurred every day of the week except Mondays, when no operations were suspended, but this was not a significant event, due to the low number of suspended interventions each day.
In our current situation start time stands out as having a 9.79min delay on average and a standard deviation of 12.41min, with no significant differences between the different days of the week. The time between interventions is between 19 and 20min, without differences between the first and second and between the second and third intervention except for Fridays where the time between the first and second intervention is quite low, dropping to 30%.
With regards to the finishing time, in 22.45% of programmed operations the last patient went out of the operating theatre after 3h pm, always with a prolongation of less than 15min, except one day in which the prolongation was almost 60min. Without taking into consideration the delay at the beginning, i.e. if all the programmes had begun punctually at the correct time (8:30am or 9:00am), this percentage would drop to 10.20%.
Activity during the last 2h of the operating theatre working is altered when surgery is delayed, with all the activities of the operating theatre being accelerated up to 10% of the regular time of these processes.
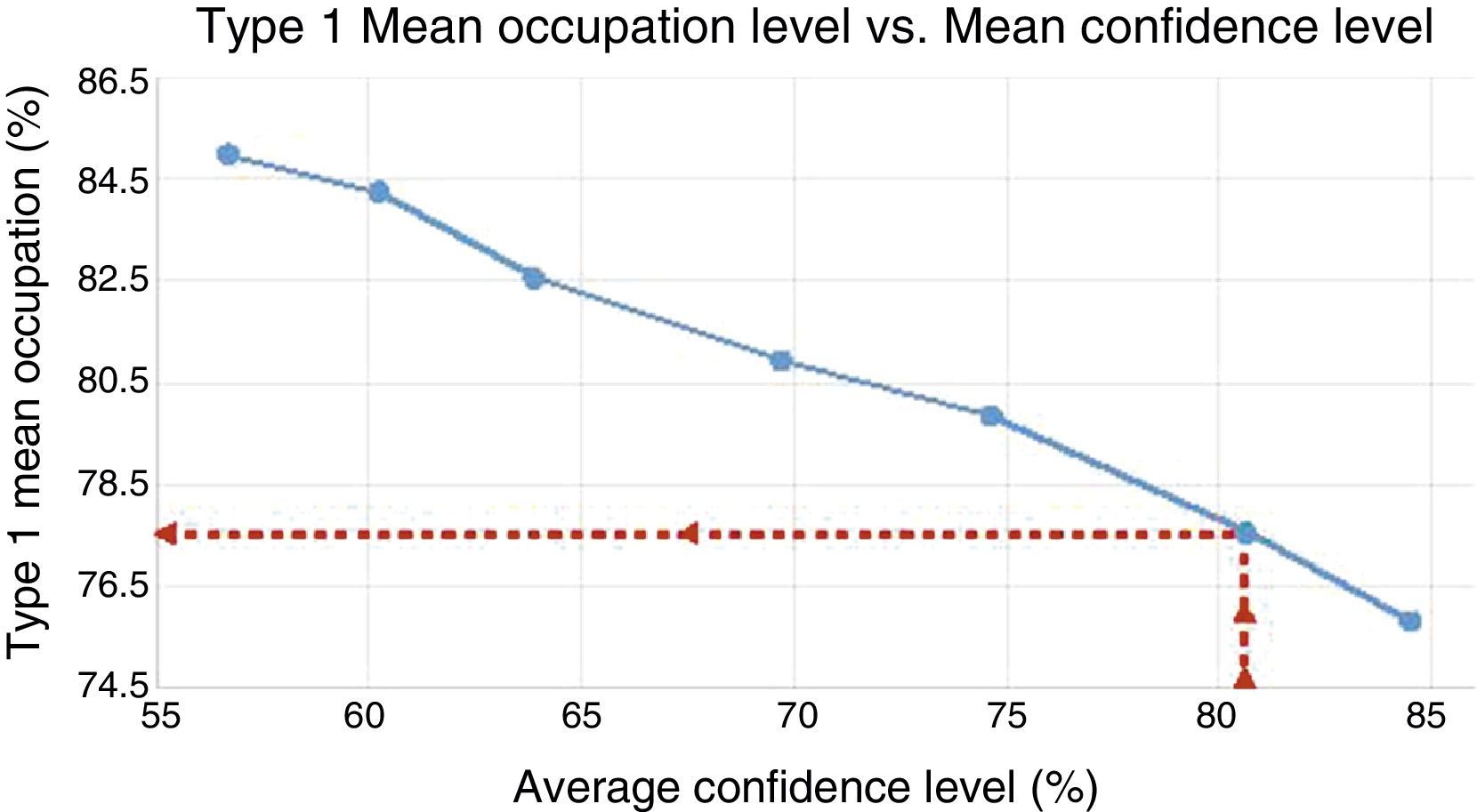
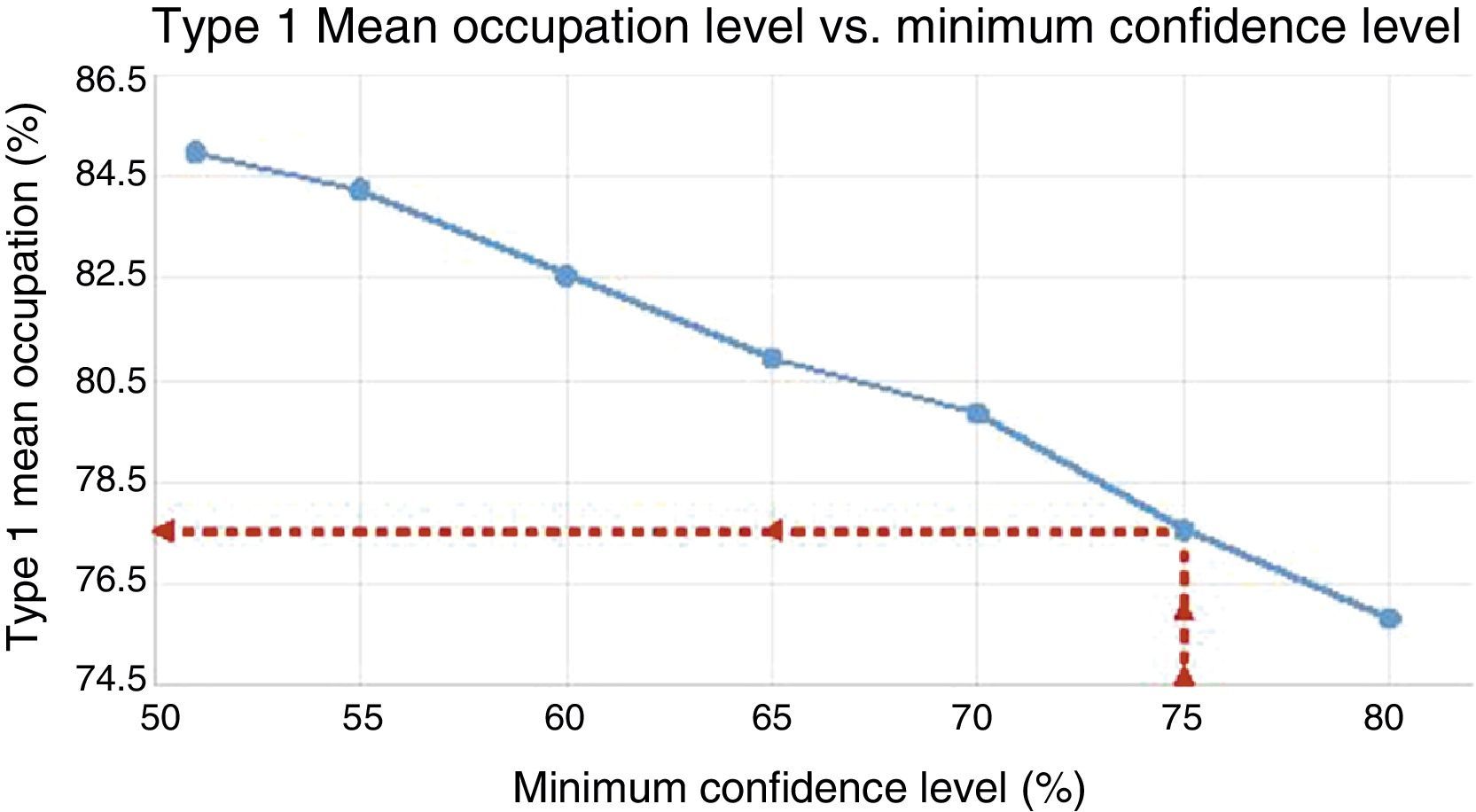
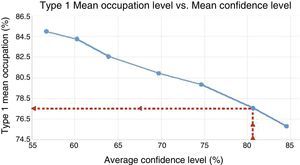
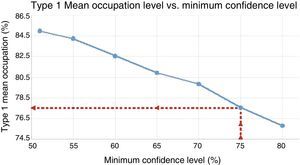
Virtual waiting listAfter carrying out several programmes with different surgical performance (Q1) from the virtual waiting list created, we found that ideal Q1 performance of an operating theatre is 77.5%, with a mean confidence level of 80.61% (Fig. 1) and minimum is 75% (Fig. 2) not going past 3h pm in its termination. Programming of the 700 patients with this ideal performance was carried out in 254 surgical sessions which entailed 1663.7h, as necessary for resolution.
DiscussionThe assignation of operating theatres to a certain service is made by the hospital management and should match the healthcare demand of this service.6 The correct use, i.e. the performance of this expensive resource,4 is studied in a specific department of each hospital formed by people who do not work with the resources, i.e. people who are not closely involved with the these resources. The data sent from these departments to the different services on the use of these resources is limited to a global or final numerical figure from which it is difficult to draw conclusions which could then be made into solutions for improvement. They are not proposed or it is difficult to extract conclusions on improvable points. The necessary monthly information which should reach a surgical service on how it functions in the surgical block is the number of interventions programmed, the number of emergency interventions, the number of interventions suspended, the rate of occupation of the operating theatres, the mean delay in commencement of surgery, the mean time between interventions and the delay in finalisation.5 If this information is not sent we ourselves are responsible for obtaining it, since these data are necessary to attempt to obtain the best management and use of available resources.
The operating theatre is the most expensive resource4 in a hospital. Its functioning may mean up to 40% of the financial cost of all hospital resources3,7 and 70% of the patients who stay there.3 For this reason an essential objective has always been that of obtaining the maximum performance from the operating theatre by reducing costs without detriment to healthcare quality, which is priority. To carry out programming with maximum use of the operating theatre we cannot base our ideas on suppositions, subjectivities, etc., on the duration of certain interventions.5 We need to know what our real times are, corresponding to historical data of our hospital and services, as we did in this study and not basing our evidence on that of other hospitals and centres where great variability exists. Knowing the actual times of our hospital, or our surgical block and our service is essential for a programming with maximum use of the operating theatres.5 Corella and Albarracín1 proposed a system of surgical pathology classification based on complexity, duration of surgery and even defining intermediate times with applicable figures but with the need to adapt to the reality of each hospital and surgical block.
Our monthly global surgical performance was that of 75.9% and 87% in Q1 and Q2, respectively, which are figures that are difficult to surpass with regards to the occupation of the operating theatre, but without a doubt are improvable, since 22.45% of sessions finished after 3h pm, which should not happen and surgical suspension is also a problem for patients and family members, creates tension between theatre personnel and problems in compensating for the extra time in the working day. The optimum performance found, i.e. that of maximum operating theatre occupation without finishing after 15.00h was 77.5% in Q1. This may be interpreted as 1.6% more than that programmed by us, equal to 6.24min. However, we should not interpret our performance as slightly lower than the ideal obtained, since if we examine the performance we have in our theatres when no intervention has been suspended, it is 78.4%. This is higher than the ideal and it may be that this high performance also leads to a delay in start time, which in over 20% of our days begins later than the scheduled time, leading to the majority of surgical suspension. In reality we programme the working days without suspension of any process, 0.9% more ideal time, which corresponds to 5.51min. This figure is eliminated by the mean delay of 9min at the start time of the first operation. If we were punctual at the start of surgery, ideal performance could change, as the delay was taken into account in the virtual programming.
With regard to our possibilities of improving programming, we cannot reduce anaesthesia or surgery time as this could entail a risk to the patient. We have to work to reduce the time between interventions, improve the punctuality at the start and even put the time of starting forward. Reducing time between interventions is complex, and could be approximately 20min. This time could be reduced but only by very little, since cleaning and preparation of the operating theatre for the next intervention necessarily takes time and its drastic reduction could lead to an increase in infections. For this reason, we have only calculated our performance in Q1, since Q2 is considered invariable regarding time between interventions. Although it is difficult, time should be taken into consideration as it is a variable we should try to improve. To sum up, our opportunity for improvement stems from improving punctuality at the beginning of surgery, a fact that has already been reported by Gómez-Arnau and González,5 since apart from the time gained, this provides an atmosphere of “seriousness and compliance” to the surgical block. We will improve if we manage to start earlier and adjust our programming to our ideal performance, thereby avoiding finishing later than the scheduled time and cancelling operations.
Surgical planning is extremely complex and tedious, and we do not normally have useful data at our disposal to help us. In the majority of hospitals this is normally carried out manually.8 Programming involves many factors, some of which are difficult to control and involve contrary interests on occasions. The variety of operations, the duration of each operation, priorities of certain pathologies, the capacity of the hospital, the time of hospital stay, doctor's timetable and patient's age all play a role.9 Good or bad surgical programming has a direct impact on the number of patients treated, waiting times and performance of the system.9 We are pursuing its maximum occupancy, the highest level of patient satisfaction, the lower financial cost, the greatest quality in surgery performed and all taking into account the enormous variability of operations carried out4,7 and of the people who daily participate in the surgical activity with very different tasks, surgeons, anaesthetists, operating theatre nurses, clinical assistants, ancillary staff, cleaners, etc., who have to synchronise their work.7 Bearing in mind these parameters, Barbagallo et al.7 carried out surgical programming using a mathematical model applied to the waiting list, obtaining an improvement in performance of operating theatres between 10% and 20%, and this was an exportable model to other specialities and hospitals like our own. In these same terms, Wolff et al.9 applied a mathematical programme and achieved an improvement in surgical performance between 10% and 15% compared with manual programming. The application of a mathematical model to health practice, i.e. the numerical quantification of the problem to be resolved,3,4,9–11 should always be taken with reserve due to the unpredictable variables that may arise, especially in carrying out surgical interventions where a whole range of factors, many of them material and human, are involved and are difficult to control. However, these reservations apart, we should know how to obtain, the maximum benefit of the enormous mathematical possibilities. Velásquez et al.10 carried out a review of the literature where the majority of solutions given in the improvement of surgical programming was based on mathematical models with heuristic methodology to simplify the complex problems of simulation, as we have seen, and considerably reduce the programme variability.4 The mathematical programming always offers better results than the manual of all the models but they are all theoretical, and have not yet been applied to a real programme.6 Whomever finds a theoretical solution to a problem will be close to its resolution.10
The programming of surgery has always been carried out by surgeons, and it is therefore surprising that all the attempts to improve it are always published by people who are theoretically removed from the surgical programming, like engineers, mathematicians, economists, etc.,3,4,6,9–12 with texts and programming that is almost always difficult for a surgeon to understand. Within the medical sector, there are anaesthesiologists and doctors of preventative medicine who have studied it.1,5 Cardoen et al.,12 in a review of the systems used in the majority of surgical programming, state that many definitions and proposals in improvement have not been negotiated or explained between researchers and those who do the programming, and they are therefore difficult to understand and apply. It has even been proposed that some of the planning models share an operating theatre in the same day for different services,6 which could lead to problems and complications due to the different characteristics of the inventions made. Due to this lack of comprehension and co-operation, we continue to do the programming manually. We are attempting to improve our programming by doing this work jointly between engineers and surgeons,13 as has been previously attempted, so that we can easily comprehend and apply medical practice.
Why is this programme interesting? There are several reasons for this. Firstly, to be able to programme optimum performance of each surgical session, i.e. its maximum occupation with minimum risk of prolonging the session over the time available. When we know the duration of interventions and intermediate times we can detect with greater precision at which point specifically problems have arisen or may arise, and therefore prevent and avoid them in the future.14 As we are able to programme the whole waiting list, we can inform the patient of the next approximate date of surgery as soon as they arrive. We can also know at all times what the surgical resources are that we need to resolve on our waiting list within a certain period and send them to the control body of the surgical block of our hospital.5 This does normally not occur as surgical resources are assigned to each service in a loose and inflexible manner. This system allows us to quantify the surgical waiting list in time, which has already been proposed for similar somewhat more complex systems.1 This system would allow us to periodically demand the appropriate division of surgical resources to the different services with specific data, depending on their needs.5 By using this system we could even report the cost which its resolution would involve.
This mathematical programme helps us to avoid the existing human subjectivity in the surgical programming, by extensively reducing variability and time dedicated to its execution, as well as increasing transparency, efficacy and equity.9 Another advantage of this mathematical programme is that with knowledge of the necessary data, the duration of interventions, intermediate times and the time when operations began are exportable to any specialty and hospital.
There is a problem with this system which progressively improves but is difficult to resolve. Not all anaesthetists or surgeons spend the same amount of times resolving a certain pathology, but we understand that all times are included in the standard deviation of each procedure. The same occurs with the teaching services with residents who perform surgery under supervision.1 For these reasons, all types of mathematical programming must be permanently open and at the same time offer feed-back with the duration of each intervention made, that is the most important data of programming.8 In this way the different types of intervention could be continuously regulated, a future objective of the programme could even be to know the individual surgical times of the anaesthesiologists and surgeons so that programming could be made according to who was to participate in the intervention.
After this study we could confirm that our surgical performance with the manual programming was difficult to improve, but it was a good learning curve to find out precise and in-depth details, problems and faults of programming and execution of surgical programmes, improving the reports sent today from the administrative bodies to the clinical services. These data were obtained by simply reviewing one month of surgical performance and making use of the historic data of our service. The results obtained from this virtual programming are preliminary but would always be necessary to introduce a new strategy, and are reliable and promising enough to introduce this type of programming with a sufficient guarantee of obtaining the expected outcome.
Level of evidenceEvidence level V.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestNo financing or economic aid was received for conducting this study. None of the authors have any conflict of interests to declare.
Please cite this article as: Albareda J, Clavel D, Mahulea C, Blanco N, Ezquerra L, Gómez J, et al. ¿Realizamos bien la programación quirúrgica? ¿Cómo podemos mejorarla? Rev Esp Cir Ortop Traumatol. 2017;61:375–382.