Scheuermann kyphosis is a structural deformity of the thoracic or thoracolumbar spine that develops prior to puberty and deteriorates during adolescence. There is limited information on its natural history but many patients are expected to have a benign course. Severe kyphosis can progress into adult life and cause significant deformity and debilitating back pain. Conservative treatment includes bracing and physical therapy, but although widely prescribed they have not been scientifically validated. Surgical treatment may be considered in the presence of a progressive kyphosis producing severe pain resistant to conservative measures, neurological compromise, or unacceptable deformity. This is associated with significant risks of major complications that should be discussed with the patients and their families. Modern techniques allow better correction of the deformity through posterior-only surgery with lower complication rates. Simultaneous shortening of the posterior vertebral column across the apical levels, along with spinal cord monitoring, reduces the risk of neurological deficits.
La cifosis de Scheuermann es una deformidad estructural de la columna torácica o toracolumbar, que aparece antes de la pubertad y empeora durante la adolescencia. Aunque generalmente de curso benigno, la información disponible acerca de su historia natural es muy escasa. En casos de enfermedad grave, la cifosis puede progresar durante la etapa adulta y ser causa de deformidad significativa y dolor incapacitante. El tratamiento conservador mediante rehabilitación y ortesis carece de evidencia científica. Se debe considerar el tratamiento quirúrgico ante la presencia de una cifosis progresiva y dolorosa, la aparición de compromiso neurológico, o deformidad inaceptable. Este conlleva un elevado riesgo de complicaciones graves que deben ser discutidas con el paciente y sus familiares. Hoy en día, gracias al desarrollo de modernas técnicas de instrumentación, la corrección de la deformidad es posible mediante un abordaje posterior único con menor incidencia de complicaciones. El acortamiento simultáneo de la columna posterior en los niveles apicales, y la monitorización espinal intraoperatoria reducen los riesgos de lesión neurológica.
In 1920, after examining the back of a 16-year-old farmer, Holger Scheuermann described the presence of a stiff and painful kyphosis of the thoracic spine which was clinically and radiologically distinguishable from postural kyphosis. He called it “juvenile kyphosis dorsalis” and only much later would this entity come to be known as “Scheuermann's disease”.1,2 Since then, this disease has been the subject of great orthopaedic interest as the cause of pain and, more importantly, significant deformity, which in some cases can be progressive.3 In 1964, Sorensen established the radiographic diagnosis of Scheuermann's kyphosis by the presence of anterior wedging greater than or equal to 5° in at least 3 consecutive vertebrae.4,5 Other characteristic findings include increased thoracic kyphosis, disc impingement and irregularities in the vertebral end plates with formation of intraspongious hernias (Schmorl nodes).3,4,6
Scheuermann's disease or kyphosis is the most common cause of painful and progressive, structural, angular hyperkyphosis of the thoracic or thoracolumbar spine in adolescents7 and the second most common cause of back pain in children and adolescents following spondylolysis/spondylolisthesis.8,9 The age of onset is around 10 or 12 years, although in some cases it can appear up to adult age.10 Its incidence has been reported in between 0.4% and 8.3% of the population,8,10,11 without a clear gender predominance.6,12–14
Two different types of deformities have described, according to their location. The classic, thoracic type (type I), is the most frequent and usually associates the presence of non-structural, lumbar and cervical compensatory hyperlordosis. The thoracolumbar type (type II) is rare, but has a higher risk of progression into adulthood and becoming a source of chronic pain.2,3,11,12,15,16 Although Scheuermann's disease has been well-described in terms of clinical presentation and radiographic findings, its aetiology remains uncertain and its treatment indications are a source of controversy.
AetiologyThe origin of Scheuermann's disease remains uncertain, although numerous theories have been proposed.15 Early theories advocated an origin related to avascular necrosis of the vertebral plates, inhibition of endochondral ossification in relation to the appearance of spongy hernias and plate perforations and the persistence of anterior vascular channels.1,9,17,18 Further studies have failed to demonstrate the consistency of these theories.3
Scheuermann's disease is considered to be “hereditary”, although its transmission pattern has not yet been defined.15 Recent studies based on twin populations indicate a multifactorial hereditary origin. Damborg et al.19 reviewed the 35,000 twins registered in the Danish population registry between 1931 and 1982, and found a significantly higher concordance by pairs and probands in monozygotic twins than in dizygotic twins, thus indicating a considerable genetic contribution to the aetiology of the disease. Halal et al. published the discovery of 5 families with an autosomal dominant inheritance pattern with high penetration but variable expression.20 Findlay et al. described the existence of a family where Scheuermann's kyphosis was present in 3 successive generations, with a male-to-male transmission pattern.21
Histopathological studiesHistopathological studies of collagen present in the vertebral plates of patients with Scheuermann's disease have shown an alteration in endochondral ossification similar to that observed in Blount's disease. This finding may represent a primary phenomenon interfering with normal, vertical, vertebral growth or may be secondary to an asymmetric axial load on the kyphotic thoracic segments of an immature spine.8,10,22
Biomechanical factorsThere are various “biomechanical factors” that could also play an important role in the aetiology of Scheuermann's disease.3 Hamstring contracture is a common finding among patients with Scheuermann's kyphosis and represents an impediment for normal pelvic inclination during trunk flexion. A concentration of repeated flexion forces through the thoracic spine as a result of chronic hamstring contracture, would cause a progressive, anterior wedging of the thoracic vertebrae.8,10 According to research by Ogden et al., the appearance of an asymmetric biomechanical stress on the vertebral bodies results in an alteration of the remodelling response. The appearance of kyphosis would then result from an imbalance of the load supported between the anterior and posterior elements of the spine.23 It has been postulated that treatment by thoracolumbar orthosis in patients with thoracic hyperkyphosis would produce a posterior displacement of the centre of gravity and load axis, leading to the disappearance of anterior vertebral wedging. This would reinforce the biomechanical theory of the origin of Scheuermann's disease.3,7,17,24,25
Other aetiological factorsOther factors which have also been implicated in the development of Scheuermann's disease are elevated growth hormone levels, idiopathic juvenile osteoporosis, vitamin D deficiency, dural cysts, spondylolysis, infections, spinal deformities and other diseases.8,12,15 It is also possible that Scheuermann's disease is a result of the simultaneous action of various factors.11
Clinical presentationThe reported incidence of Scheuermann's disease varies among the different publications between 0.4% and 8.3%, depending on the inclusion criteria employed. However, its true incidence is probably underestimated, since often its onset is attributed to altered postural habits.8,10,11,14 Recent studies have found no gender predominance.7,14
Scheuermann's kyphosis is a structural deformity of the thoracic or thoracolumbar spine which appears just before puberty, after ossification of the vertebral plates,11 and which worsens during growth in the adolescent stage until skeletal maturity. The deformity may be progressive and, therefore, become symptomatic during growth.8,14
Patients usually attend consultation towards the end of the juvenile stage, between 8 and 12 years of age. Those who attend between 12 and 16 years usually present more rigid and severe deformities. Adolescents with classical, type I Scheuermann's disease usually refer pain around the apex of the kyphosis, but often attend due to cosmetic reasons or for alleged postural habit disorders. Parents and physicians sometimes attribute the appearance of the deformity to bad postures, resulting in a delay in diagnosis and treatment.3,5,12,14 In adults, the primary symptom is usually pain.5,10
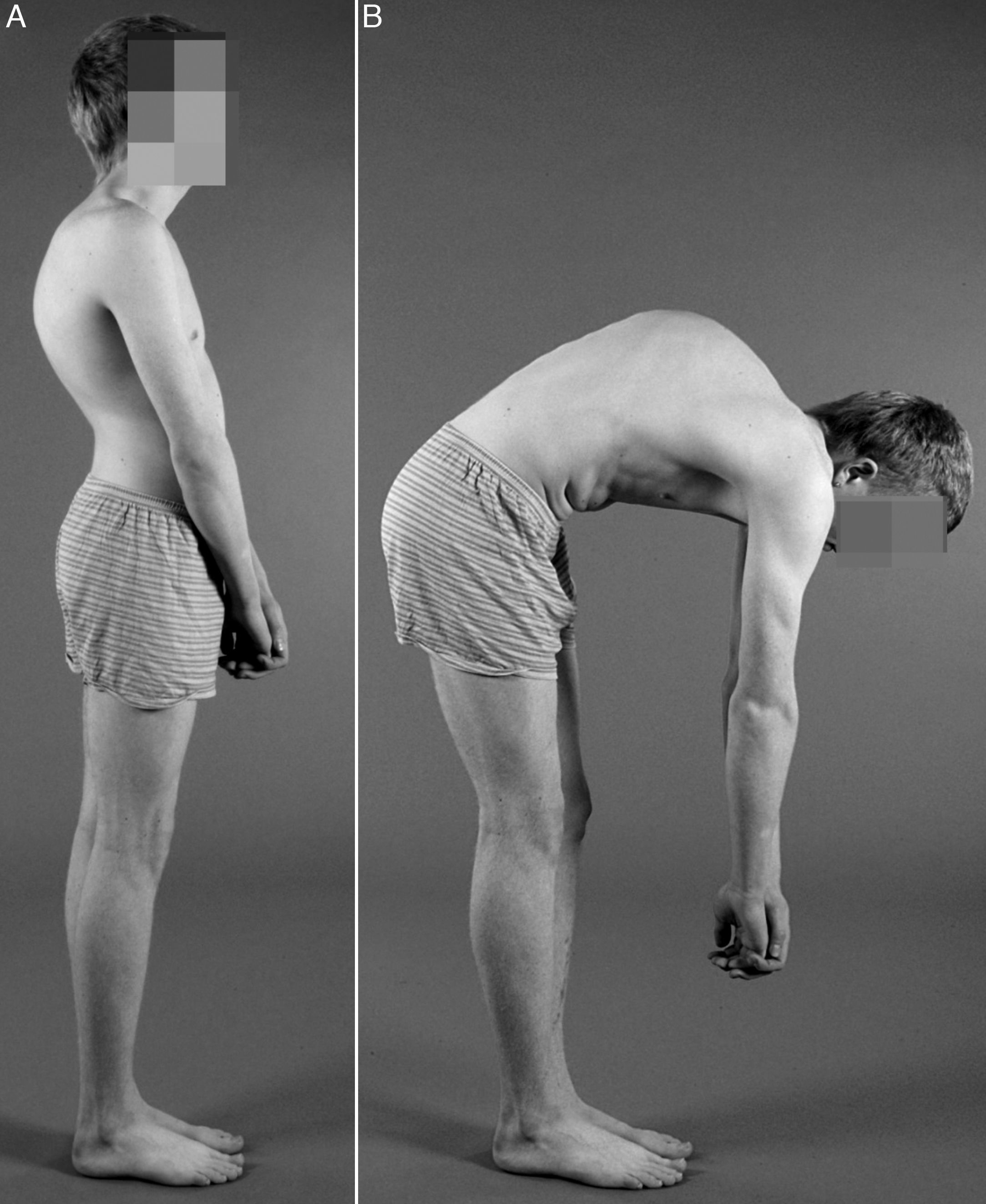
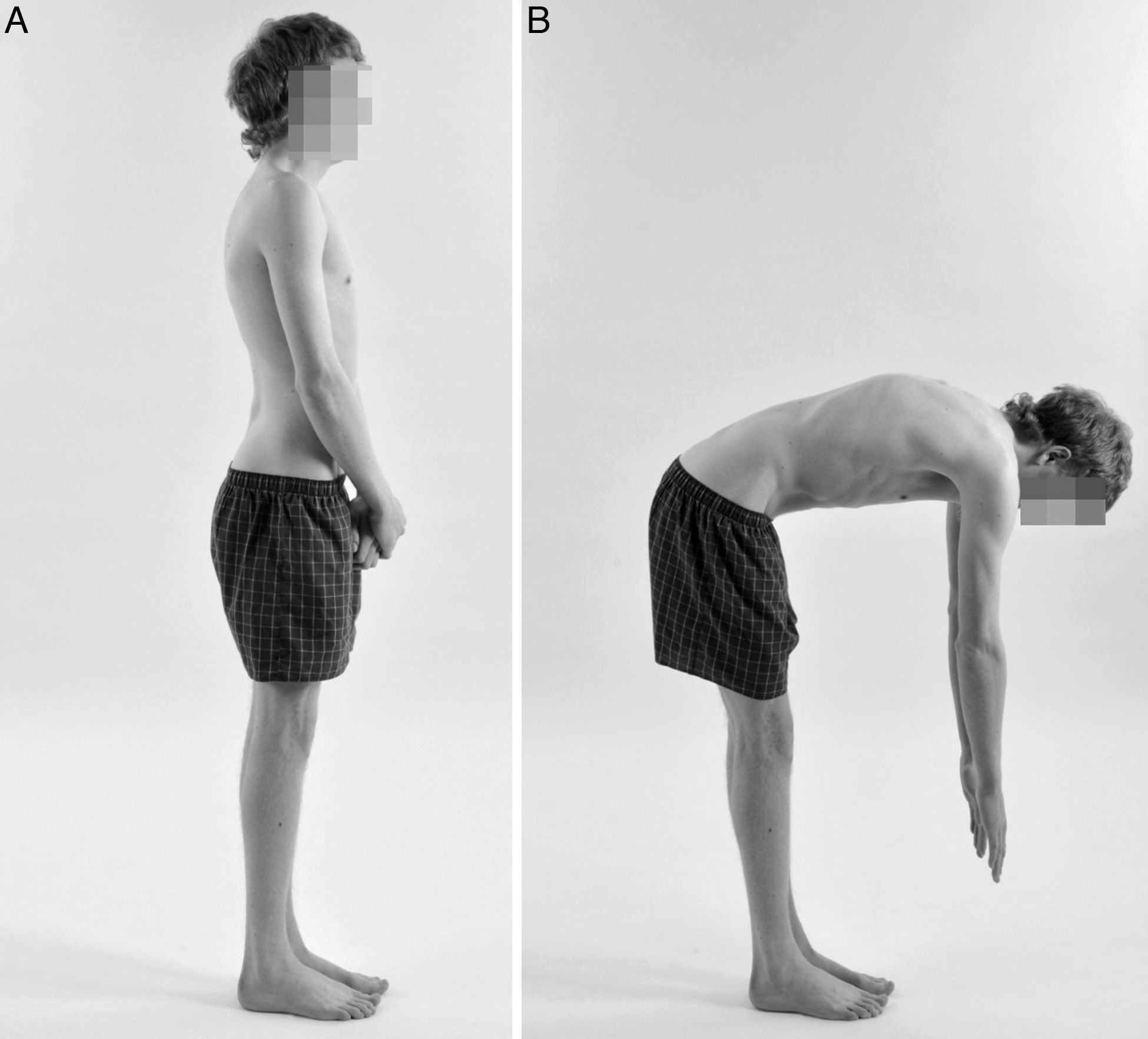
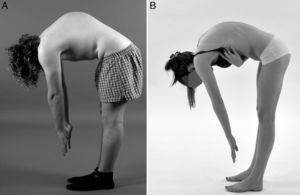
Patients with Scheuermann's kyphosis present a well-defined, angular, thoracic hyperkyphosis, which is usually associated to the presence of compensatory cervical and lumbar hyperlordosis. This increase in cervical and lumbar lordosis is the result of balancing attempts by the column, which ultimately result in the development of negative sagittal balance (Fig. 1). Moreover, on some occasions these compensatory curves can also become a source of pain.7,8,10,12,14 Lumbar hyperlordosis causes added stress on the pars interarticularis. This could explain the increased incidence of spondylolysis, which is present in up to 11% of patients and represents an added cause of lumbar pain. The head and neck adopt an anterior position which seems like a forward protrusion (“gooseneck deformity”), and sometimes the shoulders also adopt the same anterior protrusion. This characteristic position entails aesthetic disorders and dissatisfaction with body image for patients.7 Trunk flexion accentuates deformity and gives the appearance of an angular and sharp hump on the thoracic or thoracolumbar region (Fig. 1). The deformity is relatively fixed and is not corrected with spinal hyperextension.8,14 Other findings upon examination are the presence of contractures in the pectoral muscles, hamstrings and hip flexors.3,8,10,14 Nearly one third of patients also present mild or moderate scoliosis.3,6–8,12–14,18
The presence of “pain” is common, and this symptom can be exacerbated by standing, sitting or physical work.8,12,14 In a study with 103 patients, Sorensen reported the presence of pain as the main symptom in about 50% of patients.4 Other authors have reported the presence of pain in 20–60% of patients.5 Adults with progressive Scheuermann's disease who reach adulthood without treatment may report the presence of disabling pain, especially if the deformity is severe.14 Pain is usually located in the paravertebral region, just caudal to the apex of the kyphosis,5 and may even affect hyperlordotic areas above and below the deformity.10,12 The presence of pain in the lumbosacral region should lead to suspicion of an association with spondylolysis/spondylolisthesis.8,10
Neurological symptoms are not a common finding in patients with Scheuermann's disease, but they may appear in the form of radicular pain with progressive weakness of the lower limbs, even spastic paraparesis.5,10,14,15 There have been reports of neurological symptoms secondary to the onset of thoracic disc herniation, dural cysts or by spinal traction and compression mechanisms in the apex of the kyphosis in cases of severe deformity.5,7,8,26,27 Patients with short and sharp kyphosis are considered to be most at risk of developing neurological complications.7 A study published by Lonstein et al. showed that mean kyphosis was 95° among patients with neurological symptoms.28 On the other hand, Ryan and Taylor published a mean kyphosis of 54° in 3 patients with acute spinal cord compression at the apex of the kyphosis.29 Kapetanos et al. described the case of a 14-year old boy who presented spastic paraparesis due to the presence of a herniated disc in the apex of a thoracic kyphosis.26 At least another 20 cases of spinal involvement secondary to disc protrusion have been described in patients with Scheuermann's disease.
Cardiopulmonary symptoms are uncommon among patients with Scheuermann's disease.5,10 Sorensen stated that the thoracic deformities secondary to hyperkyphosis caused no impact on cardiopulmonary function.4 Nevertheless, Murray et al. documented a significant decrease in total lung capacity and forced vital capacity among cases of kyphosis above 85° with the apex of the deformity in the high thoracic region.13
Type II Scheuermann's disease is much less common. In these cases, the deformity is located in the lumbar or thoracolumbar spine and patients generally refer more pain and greater restriction to perform physical tasks, compared to type I patients. Also, the thoracolumbar cosmetic deformity is not as evident, due to the more caudal location of the apex of the kyphosis.5,12,15 Nevertheless, thoracolumbar hyperkyphosis has a greater risk of progression during the adult stage.3,11
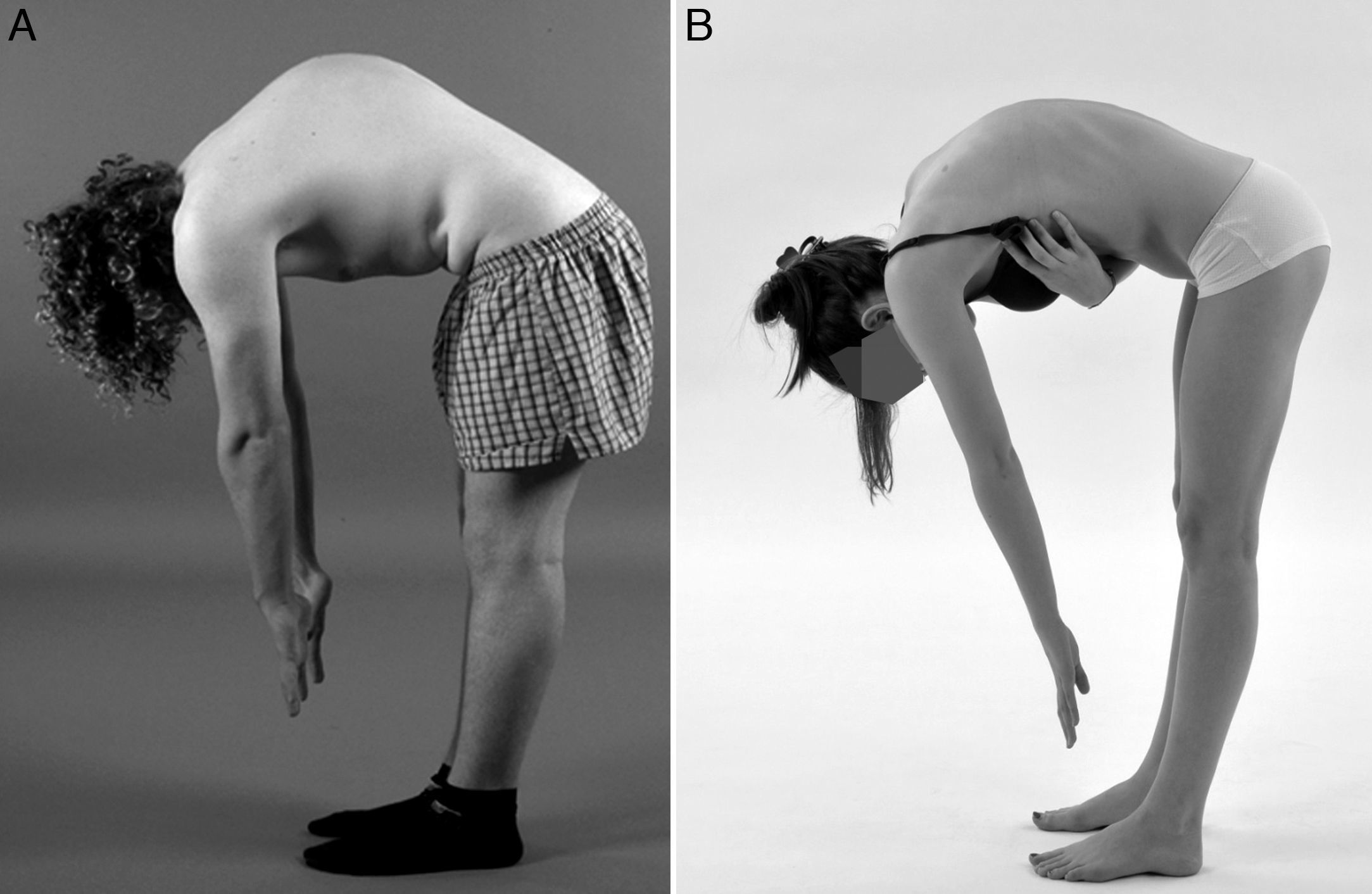
Differential diagnosisIt is vital to differentiate Scheuermann's disease from curved back or postural kyphosis (Fig. 2). The latter is benign and can be voluntarily corrected through trunk extension. Postural kyphosis is flexible and has a less angular and more rounded shape, generally below 60°. In addition, it does not present the characteristic radiological images of Scheuermann's disease. Moreover, postural kyphosis presents a smoother, more flexible and symmetrical contour of the spine upon trunk flexion.5,7,8,12 The differential diagnosis of Scheuermann's disease should also take into account other conditions such as osteochondral dystrophy and spondyloepiphyseal dysplasia, congenital kyphosis, spondylodiscitis, sequelae from vertebral compression fractures, ankylosing spondylitis, kyphosis postlaminectomy and neoplasms.5,10,15
Differential diagnosis. Clinical photographs of a male patient with Scheuermann's disease in lateral lumbar flexion (A), and of a female patient with curved back or postural kyphosis (B). The latter presents a smoother and more symmetrical contour, with a less angular and more rounded thoracic spine.
The Scoliosis Research Society has established normal thoracic kyphosis values between 20° and 40° (measured between T5 and T12). However, the relevant literature reflects the existence of a wide variability for what could be considered normal sagittal balance in asymptomatic individuals.12 In a study of 316 asymptomatic subjects, Fon et al. established an upper limit of 45° for normal thoracic kyphosis, also adding that this value increased with age.30
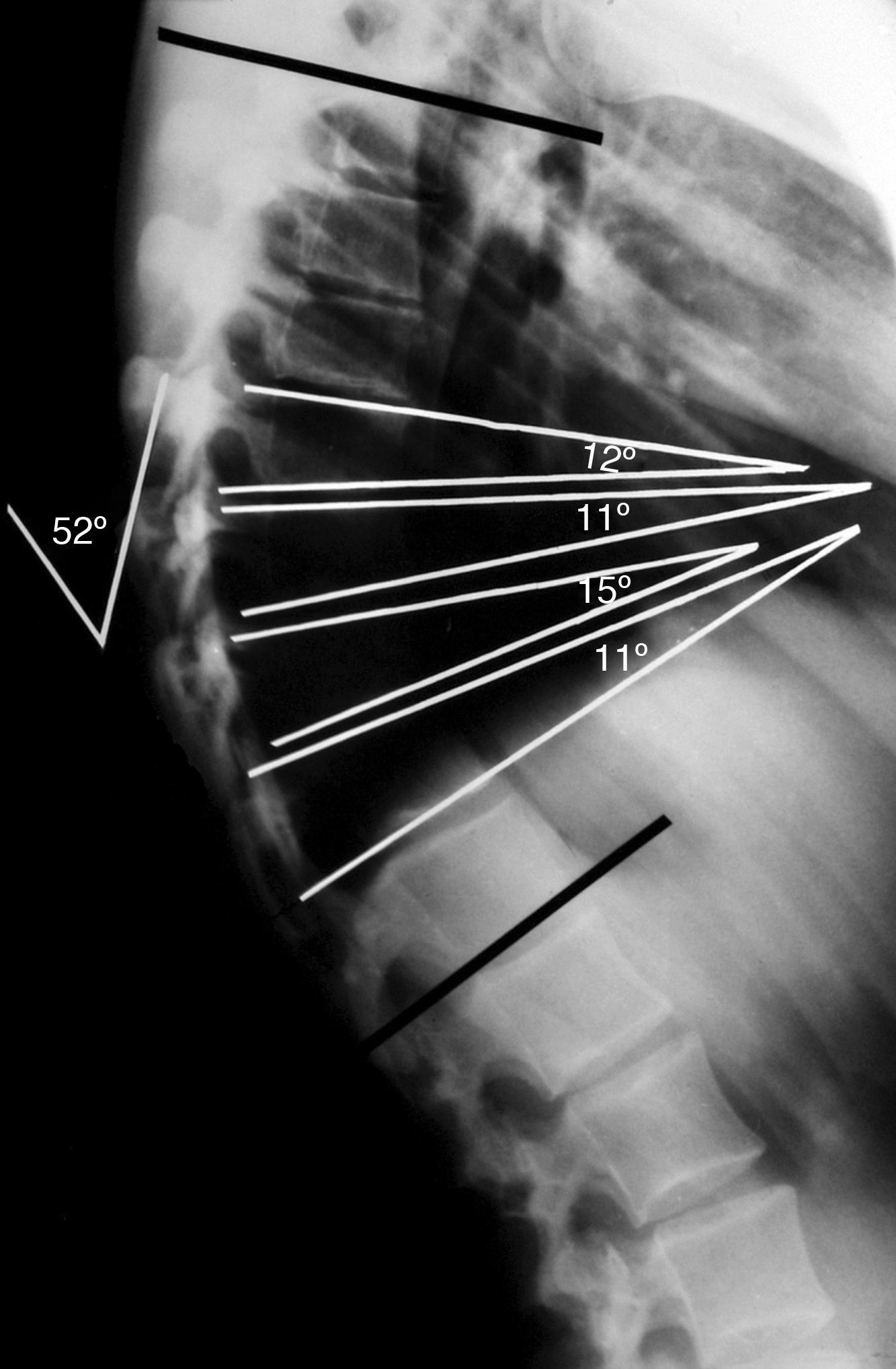
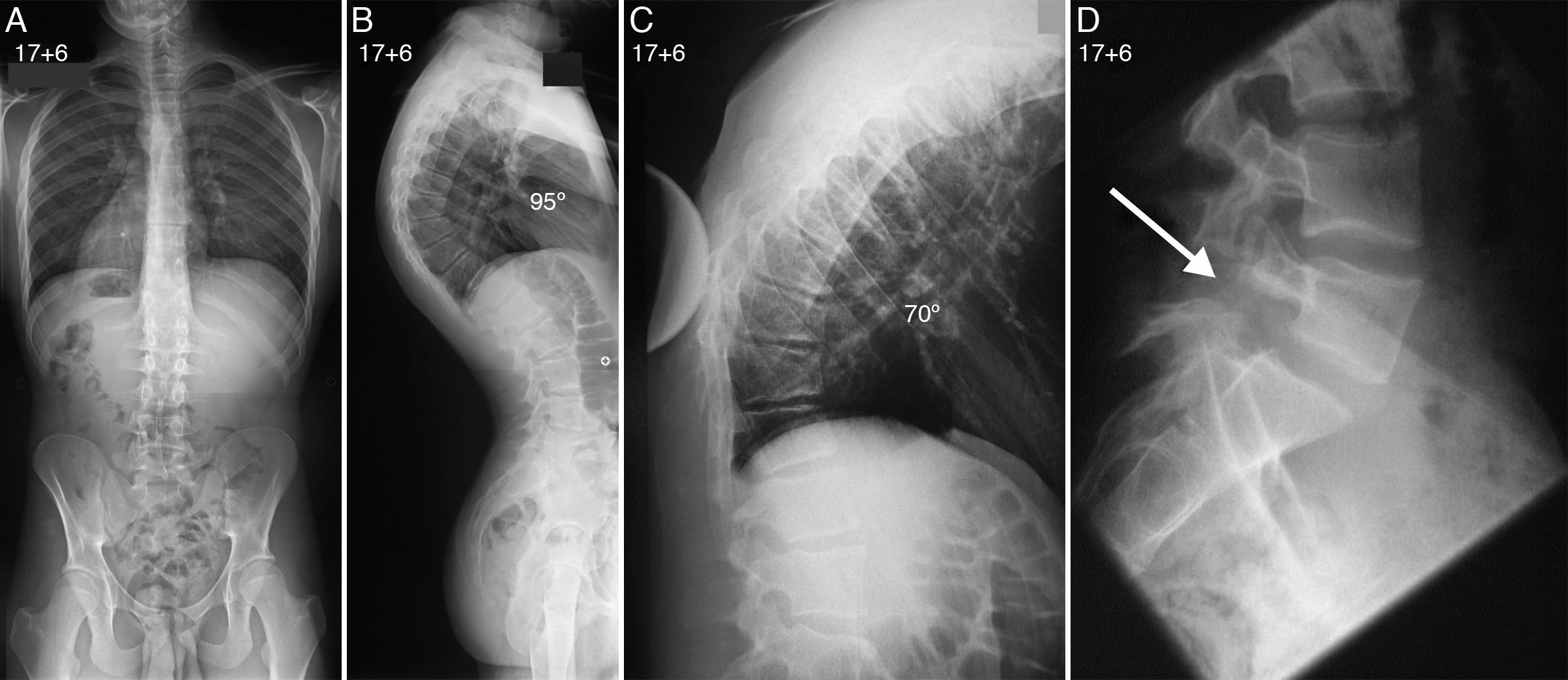
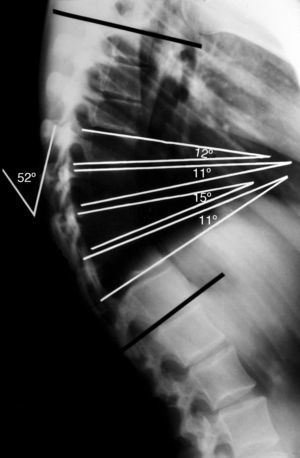
The diagnosis of Scheuermann's disease is obtained by lateral spine radiography with the patient standing and with both shoulders and arms at 90° or on the ipsilateral clavicle (clavicular position).7,31 In order to measure the angle of kyphosis, the final cranial and caudal vertebrae included in the deformity must be selected.5 The measurement of the wedging degree is obtained from the angle of intersection of the tangents on the upper and lower plates of each vertebral body.8,10,12,15 The diagnostic criterion establishes a level of wedging over 5° in at least 3 consecutive vertebrae in the apex of kyphosis (Fig. 3). Other common findings in radiology include the presence of Schmorl hernias, irregularity and thinning of the vertebral plates and discal space impingement.4,6 The degree of flexibility of hyperkyphosis is measured in the lateral projection, with the patient in hyperextension on a wedge or pivot (Fig. 4).5,8,10,12,15 In the classical type I disease, the apex of kyphosis is located between T6 and T9.10,15 In type II, the apex of kyphosis is located in the thoracolumbar junction.2,10,12,15
Simple lateral radiograph of an adolescent patient with Scheuermann's disease, showing a thoracic kyphosis of 52°. The measurement of the segmental wedging degree is obtained from the angle of intersection of the tangents on the superior and inferior plates of each vertebral body. The diagnostic criterion establishes a wedging greater than 5° in at least 3 consecutive vertebrae at the apex of the kyphosis.
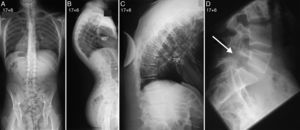
Spinal radiographs of a patient with Scheuermann's disease at 17 years and 6 months of age (Fig. 1). The posteroanterior projection (A) rules out the presence of associated scoliosis, whereas the lateral projection (B) shows the presence of a thoracic kyphosis of 95°. A lateral radiograph of the thoracic spine in the supine position (C) with the patient in hyperextension on a wedge or pivot shows a correction of the thoracic kyphosis up to 70°. The lateral projection of the lumbosacral spine (D) reveals the presence of an associated isthmic spondylolysis.
Patients with Scheuermann's disease tend to present a negative overall sagittal balance, which is evidenced by following the plumb line from the centre of the C7 body to the sacral plate in the lateral spinal radiograph. With a negative sagittal balance, the plumb line lies behind the posterosuperior corner of the sacral plate.10
There are different radiographic variants of classical Scheuermann's disease. Summers et al. reviewed 50 radiography reports with the diagnosis of “Scheuermann's disease” and found that only 20% could be considered as classical Scheuermann's disease. Thus, the radiological diagnosis of Scheuermann's disease should be restricted only to those patients in whom the presence of radiographic irregularities in the end plates, discal space impingement and Schmorl hernias are demonstrated, associated to an increase of thoracic spinal kyphosis.2
In order to rule out the presence of disc herniation or spinal traction or compression at the apex of the deformity, a complementary magnetic resonance imaging (MRI) study should be performed in cases presenting motor or sensory deficits, hyperreflexia or other abnormalities during the neurological examination. In addition, it should be used as an aid for surgical planning.8,15
Natural historyThe information available about the long-term prognosis of patients with Scheuermann's disease is very scarce, regarding both treated and untreated patients. Although the disease typically follows a benign course,7,8 the presence of a severe hyperkyphosis (above 80° Cobb) may associate the appearance of a progressive and painful deformity in adult age.8,12,17 Murray et al. published the results of the long-term monitoring of a group of patients with Scheuermann's thoracic kyphosis.13 These authors compared the quality of life and capacity for activities of daily living of 67 patients with a control group of similar age and gender characteristics (serial radiology, clinical examination, muscle strength and respiratory function). Mean kyphosis was 71° and the mean follow-up period was 32 years. The group of patients with Scheuermann's kyphosis presented a higher frequency of back pain, greater concern for their physical appearance and generally had less physical jobs or occupations than the control group. However, they did not present incapacitating symptoms and the aesthetic concern often decreased with age. In general, thoracolumbar deformity (type II) caused greater functional limitations than thoracic hyperkyphosis. Up to 38% of patients reported suffering a level of pain which caused a significant alteration in their activities of daily living, compared with 21% of patients in the control group. However, in this study, the authors did not address the progression of kyphosis, despite it possibly being the greatest cause for concern among adolescents seeking medical attention.11 According to Lowe and Kasten,32 adults with more severe deformities due to untreated Scheuermann's disease may present severe back pain secondary to degenerative spondylosis, which could result in severe functional limitation. Unfortunately, the limited data about Scheuermann's disease available so far, regarding both treated and untreated patients, do not provide sufficient clinical evidence to improve current treatment recommendations. Further studies would be required to assess the evolution of Scheuermann's disease according to the magnitude of deformity, especially for levels of kyphosis between 70° and 90°, as well as any potential neurological complications. Such studies would also help to establish clinical guidelines in relation to surgical or conservative treatment of Scheuermann's disease.7,11,17
TreatmentScheuermann's disease can associate a less obvious cosmetic deformity, and even be asymptomatic. In the absence of long-term studies on the outcome of surgical or conservative options, the treatment of Scheuermann's disease must be individualised and tailored to the real needs and circumstances of each patient. Any decision about the most appropriate treatment will depend on the presence of pain, severity and/or progression of kyphosis, the level of aesthetic deformity and its psychological implications and, although rare, the appearance of cardiopulmonary or neurological involvement.3,7,10,12,13,15
PhysiotherapyAdolescents with immature skeletons who present a slight increase in normal kyphosis, with values of up to 60° and no evidence of worsening of the deformity, will only require regular clinical and radiological follow-up until they reach skeletal maturity. Exercises which can help to relieve the symptoms are those aimed at improving balance and posture through progressive stretching of the thigh and chest muscles, as well as strengthening of the abdominal and dorsal muscles.8,12,15,33 Physical therapy exercises can also help during the initial development stages of hip flexion contractures and increased lumbar lordosis associated to thoracic kyphosis.3 Physical therapy can sometimes produce a noticeable improvement in the symptoms, but nevertheless it will not produce any effect on the magnitude of the deformity. Performing regular exercise is also recommended for those patients treated with thoracolumbar orthosis.8 Weiss et al. conducted a long-term study with 351 patients who presented pain secondary to Scheuermann's kyphosis treated with physiotherapy exercises.34 At the end of the treatment, patients reported a reduction in pain between 16% and 32%. Nevertheless, this study does not mention the extent of kyphosis. Platero et al. conducted a study comparing 4 different forms of conservative treatment for the treatment of juvenile kyphosis in a group of 212 patients (physiotherapy exercises, orthotic correction, plaster brace followed by maintenance orthosis and physiotherapy exercises followed by correction orthosis). The group treated by physiotherapy alone showed less improvement.35
Treatment with orthosisAt present there are few studies available on the effectiveness of treatment for Scheuermann's disease through the use of an orthosis. Most studies are retrospective, have different inclusion criteria and lack a control group. In addition, the level of kyphosis which would increase the risk of deformity progression has not yet been established. Classically, treatment through the use of orthoses has been considered effective in cases of mild Scheuermann's disease and skeletal immaturity.3,12,25,36,37 Increased flexibility of the kyphosis, early start of treatment with orthoses in patients with hyperkyphosis less than 65°, an initial correction of the deformity over 15° in the orthosis and the presence of skeletal immaturity with at least 1 year of growth remaining, are considered as good prognostic factors.33,38
Montgomery and Erwin25 reviewed the results of treatment with a modified Milwaukee brace in a group of 39 patients with Scheuermann's disease for a mean period of 18 months. Mean kyphosis before the start of treatment was 62°, and it descended to 41° at the end of treatment. A longer follow-up revealed a mean correction loss of 15°, so the final mean improvement was 6°. The mean anterior wedging of the vertebral body went from 7.9° to 6.8° after treatment.
Sachs et al. conducted a long-term study of treatment results with the Milwaukee brace in an initial group of 120 patients with Scheuermann's disease.37 The minimum follow-up period was 5 years after the end of treatment. At the end of follow-up, 63% (n=76) of patients showed improvement of kyphosis, 17% (n=10) did not experience any change and 20% (n=24) suffered a worsening of the initial kyphosis (7 of whom underwent surgical treatment). Unfortunately, the total, initial, mean improvement among the group was subsequently followed by a gradual loss of correction. When considering the level of deformity before treatment, at the end of treatment patients with deformities between 55° and 64° presented a mean improvement of 7°, patients with kyphosis between 65° and 74° presented a mean improvement of 13° and patients with kyphosis in excess of 74° presented a mean improvement of 19°. The authors noted that 30% of patients whose compliance with the treatment was verified showed a progression of kyphosis after completing it.
Riddle et al.39 published results comparable to those obtained with the Milwaukee brace by using a thoracolumbosacral orthosis (TLSO) for the correction of thoracic hyperkyphosis, adding a pressure point on the sternum as 1 of the 3 points of TLSO pressure. A total of 20 patients were included in the study and were monitored until skeletal maturity. The authors were able to demonstrate an absence of progression or even improvement of kyphosis in 73% (n=16), whilst the remaining 27% (n=6) showed a mean increase of 9° in their kyphosis at the end of the monitoring period. Riddle et al. recommend a minimum treatment period of 16 months before reaching skeletal maturity, in order to induce arrest or improvement of the deformity.
The literature does not reflect the existence of medical complications in studies on the treatment of patients with Scheuermann's disease by orthosis. However, the psychological implications of the daily use of a brace in adolescent patients should not be underestimated.3 At present, the available information does not enable physicians to make predictions about the improvement, prevention of progression or worsening of the deformity following treatment with orthoses in any patient.11
Surgical treatmentEstablishing surgical indications is an ongoing source of controversy due to the limited evidence available regarding the natural history of the disease. Nor there is sufficient information in the current literature about the long-term results of surgical treatment. Surgical treatment should be considered in the presence of severe and progressive deformity (above 70°), and especially if the patient is still in a growth phase and harbours aesthetic concerns, after failure of treatment with orthoses to control the progression of hyperkyphosis, in the presence of disabling pain resistant to conservative treatment for at least 6 months or with neurological involvement due to medullary compression at the apex of the kyphosis.5,7,15,32,40–42
The decision to opt for surgical treatment should be primarily based on the severity of symptoms, as well as the concerns harboured by patients regarding their aesthetic appearance and rejection of the deformity, and secondly on the level of hyperkyphosis. Surgery produces an aesthetic improvement and this is usually a key factor in the decisions adopted by adolescents and their families. The risks associated with surgical treatment and its possible complications should be explained and discussed in advance with patients and their families. Surgeons should also evaluate their ability to provide an optimal correction of the deformity, while at the same time avoiding complications.7
Biomechanical principles for the correction of kyphosisThroughout the development of the kyphosis curve, the anterior spine undergoes a gradual shortening in relation to the posterior spine and the spinal cord must adjust to the length difference between both columns. As the deformity progresses, the bone gradually becomes compressed at the apex of the kyphosis. The correction of hyperkyphosis produces a sudden stretching of the anterior column, involving a risk of neurological damage due to sudden stretching of the spinal cord, including the risk of paraplegia (caused by local axial compression through the formation of a loop). Therefore, it is necessary to perform a shortening of the posterior column through multiple segmental osteotomies at the apex of the hyperkyphosis, in order to achieve a balanced correction between the anterior and posterior columns and thus avoid stretching of the spinal cord.7 This simple biomechanical principle is hardly mentioned in the relevant literature despite being essential for the surgical correction of Scheuermann's disease in terms of increasing safety and decreasing neurological risk.
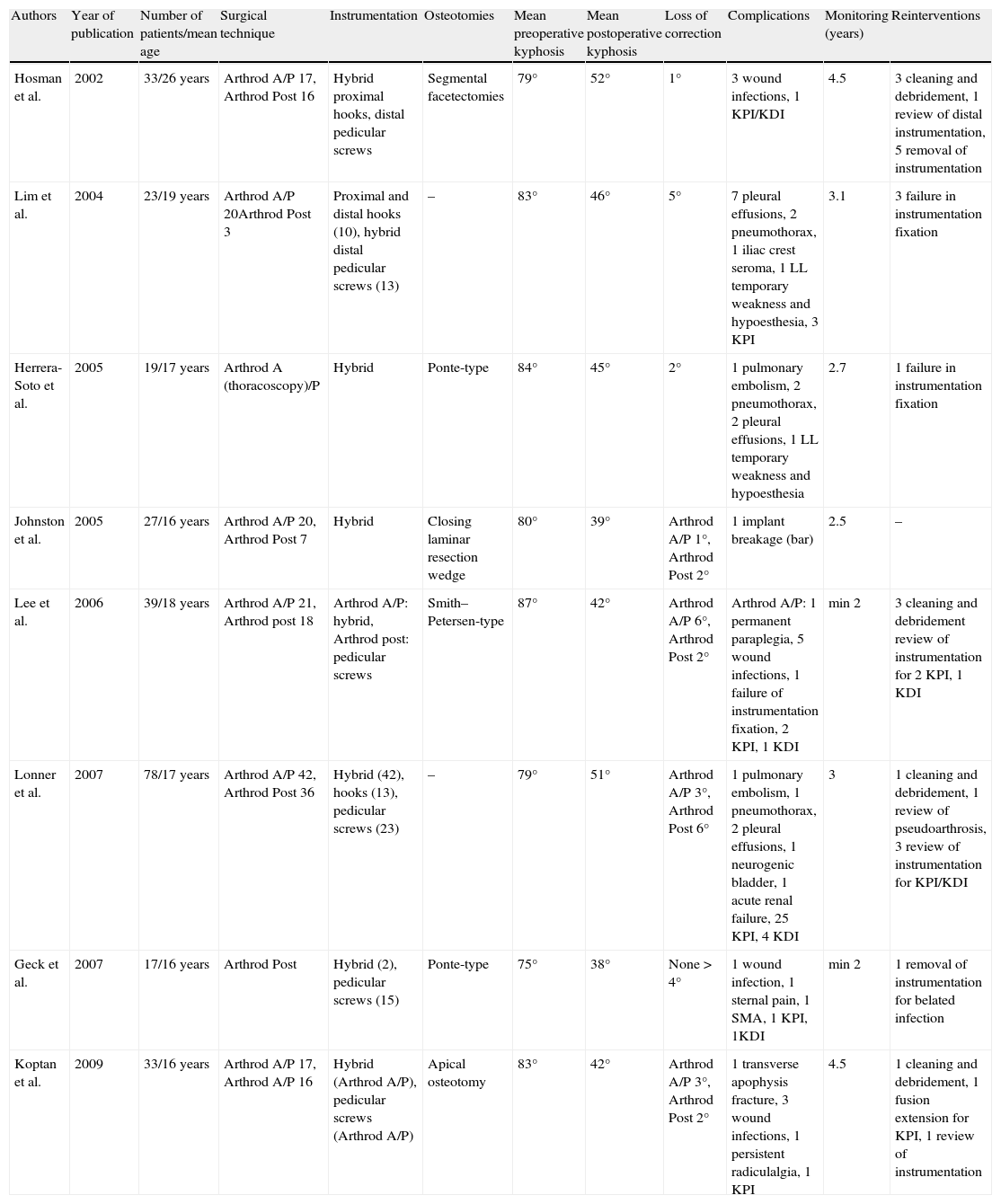
Surgical techniquesThe literature contains studies with satisfactory results through the use of both the single posterior approach (posterior instrumented arthrodesis) and the double approach with anterior release and arthrodesis plus posterior instrumented arthrodesis.17,32,43 Current controversies include the need to add an anterior release compared to the single posterior approach, the selection of optimal superior and inferior levels for instrumented arthrodesis, the use of hybrid instrumentation instead of only transpedicular screws and the type of posterior column shortening to be employed (Table 1).44–51
Summary of the published series on the surgical treatment of Scheuermann's disease.
| Authors | Year of publication | Number of patients/mean age | Surgical technique | Instrumentation | Osteotomies | Mean preoperative kyphosis | Mean postoperative kyphosis | Loss of correction | Complications | Monitoring (years) | Reinterventions |
| Hosman et al. | 2002 | 33/26 years | Arthrod A/P 17, Arthrod Post 16 | Hybrid proximal hooks, distal pedicular screws | Segmental facetectomies | 79° | 52° | 1° | 3 wound infections, 1 KPI/KDI | 4.5 | 3 cleaning and debridement, 1 review of distal instrumentation, 5 removal of instrumentation |
| Lim et al. | 2004 | 23/19 years | Arthrod A/P 20Arthrod Post 3 | Proximal and distal hooks (10), hybrid distal pedicular screws (13) | – | 83° | 46° | 5° | 7 pleural effusions, 2 pneumothorax, 1 iliac crest seroma, 1 LL temporary weakness and hypoesthesia, 3 KPI | 3.1 | 3 failure in instrumentation fixation |
| Herrera-Soto et al. | 2005 | 19/17 years | Arthrod A (thoracoscopy)/P | Hybrid | Ponte-type | 84° | 45° | 2° | 1 pulmonary embolism, 2 pneumothorax, 2 pleural effusions, 1 LL temporary weakness and hypoesthesia | 2.7 | 1 failure in instrumentation fixation |
| Johnston et al. | 2005 | 27/16 years | Arthrod A/P 20, Arthrod Post 7 | Hybrid | Closing laminar resection wedge | 80° | 39° | Arthrod A/P 1°, Arthrod Post 2° | 1 implant breakage (bar) | 2.5 | – |
| Lee et al. | 2006 | 39/18 years | Arthrod A/P 21, Arthrod post 18 | Arthrod A/P: hybrid, Arthrod post: pedicular screws | Smith–Petersen-type | 87° | 42° | Arthrod A/P 6°, Arthrod Post 2° | Arthrod A/P: 1 permanent paraplegia, 5 wound infections, 1 failure of instrumentation fixation, 2 KPI, 1 KDI | min 2 | 3 cleaning and debridement review of instrumentation for 2 KPI, 1 KDI |
| Lonner et al. | 2007 | 78/17 years | Arthrod A/P 42, Arthrod Post 36 | Hybrid (42), hooks (13), pedicular screws (23) | – | 79° | 51° | Arthrod A/P 3°, Arthrod Post 6° | 1 pulmonary embolism, 1 pneumothorax, 2 pleural effusions, 1 neurogenic bladder, 1 acute renal failure, 25 KPI, 4 KDI | 3 | 1 cleaning and debridement, 1 review of pseudoarthrosis, 3 review of instrumentation for KPI/KDI |
| Geck et al. | 2007 | 17/16 years | Arthrod Post | Hybrid (2), pedicular screws (15) | Ponte-type | 75° | 38° | None>4° | 1 wound infection, 1 sternal pain, 1 SMA, 1 KPI, 1KDI | min 2 | 1 removal of instrumentation for belated infection |
| Koptan et al. | 2009 | 33/16 years | Arthrod A/P 17, Arthrod A/P 16 | Hybrid (Arthrod A/P), pedicular screws (Arthrod A/P) | Apical osteotomy | 83° | 42° | Arthrod A/P 3°, Arthrod Post 2° | 1 transverse apophysis fracture, 3 wound infections, 1 persistent radiculalgia, 1 KPI | 4.5 | 1 cleaning and debridement, 1 fusion extension for KPI, 1 review of instrumentation |
Arthrod A/P, anterior and posterior arthrodesis; KDI, kyphosis distal to instrumentation; KPI, kyphosis proximal to instrumentation; LL, lower limbs; SMA, superior mesenteric artery syndrome.
There are several studies comparing the double approach with single posterior approaches. However, the appropriate indications for each case have not yet been established.45,46 The anterior approach enables a complete discectomy and offers the possibility of releasing the anterior longitudinal ligament (ALL), as well as placing grafts between vertebral bodies under compression conditions. Doubles approaches are usually reserved for cases of very rigid and severe deformities which are not corrected by forced trunk hyperextension, and especially in the presence of bone ankylosis of the posterior column with ossification of the ALL at the apex of the hyperkyphosis.8,10 The anterior approach can be performed either by open thoracotomy or, with better results and less surgical morbidity but with less capacity to obtain a complete discectomy, by thorascocopy.44
Lowe and Kasten32 published a retrospective study of 32 patients with a mean kyphosis of 85° who were treated by a double approach and hybrid segmental instrumentation. Mean kyphosis after surgery was 43°, with a mean loss of 4° during follow-up. The complications included 5 cases of kyphosis cranial to the arthrodesis associated with overcorrection of the deformity (>50%) or with a cranial end of the instrumentation below the final cranial vertebra of the kyphosis as measured in preoperative radiographs, as well as 2 cases of kyphosis caudal to the arthrodesis whose fusion ended cranially to the first lordotic segment.
Complications associated with the double approach in the context of surgical treatment of Scheuermann's disease include the appearance of haemothorax, pneumothorax, pleural effusion, wound infection and paraplegia.7,11,44 In addition, the double approach also produces a negative impact on pulmonary function.44 The double approach was the technique usually employed for surgical correction of Scheuermann's kyphosis until the appearance of segmental transpedicular instrumentation.10,32
In 2009, Coe et al. published the report of the Morbidity and Mortality Committee of the Scoliosis Research Society. This informed of similar complication rates obtained with single posterior procedures (14.8%) and double approaches (16.9%), suggesting that the addition of an anterior approach would not produce a substantial increase in the number of complications.52 Lee et al.45 compared a group of 18 patients undergoing Smith–Petersen osteotomy plus posterior instrumented arthrodesis with transpedicular screws, with a group of 21 patients who underwent a double approach and hybrid posterior instrumentation. Intraoperative bleeding and total operating time were both significantly lower in the group intervened by single posterior approach. In addition, patients intervened by single posterior approach did not present any surgical complications, had lower postoperative residual kyphosis and maintained a greater correction of deformity after monitoring.
The posterior approach does not interfere with anterior vascularisation of the spinal cord and has the advantages of reduced blood loss and a shorter surgical procedure.10 However, patients with highly developed and rigid deformities would not be good candidates for the correction of kyphosis by the single posterior approach. Since the ALL would remain intact, the posterior instrumentation would be subjected to a constant tension force, with subsequent increase of the risk of implant failure and appearance of pseudoarthrosis.10,53
Geck et al.54 published excellent results following correction of the deformity in 17 patients in whom they performed a simultaneous shortening of the posterior column by means of sequential segmental osteotomies (Ponte osteotomies), plus posterior instrumentation with transpedicular screws, without performing a previous anterior release. The mean preoperative kyphosis of 75° was corrected to a mean value of 38°, and no patient lost more than 4° during follow-up. Among the complications, they mentioned 1 case of cranial kyphosis and 1 case of caudal kyphosis to the instrumentation, as well as 1 belated infection, but no neurological complications. With the emergence of newer and more modern instrumentation techniques, procedures for surgical correction through a single posterior approach have become the most common surgical technique employed in the surgical treatment of Scheuermann's disease.10
Surgical technique preferred by the authorsIn our experience, most patients with Scheuermann's disease can be treated by a single posterior approach and instrumented arthrodesis, along with multiple, closing, segmental osteotomies, in order to release and mobilise the deformity. This enables its correction by a shortening of the posterior column. Shortening of the posterior column can be achieved through a complete and bilateral excision of the spinous apophyses and the superior and inferior articular facets in chevron-type, segmental osteotomies performed on the apical levels of the hyperkyphosis, between the cranial and caudal levels of the instrumentation.8 We do not believe it necessary to divide the yellow ligament and, therefore, invade the channel, unless the yellow ligament is ossified. In this case it will have to be divided in order to release and mobilise the deformity55 so as to reduce the risk of neurological lesion and epidural bleeding when the osteotomies are performed. Using this technique, we have obtained highly satisfactory results in over 40 patients with Scheuermann's disease and hyperkyphosis between 80° and 140°, as well as a flexibility measured through radiographs in forced hyperextension on a wedge or pivot up to 95°. It was necessary to add an additional anterior approach in cases of spontaneous ossification of the ALL or appearance of bridging osteophytes in the anterior part of the vertebral bodies, at the apical levels of hyperkyphosis. These could be a result of the natural history of an extreme hyperkyphosis, in an attempt to obtain stability.55
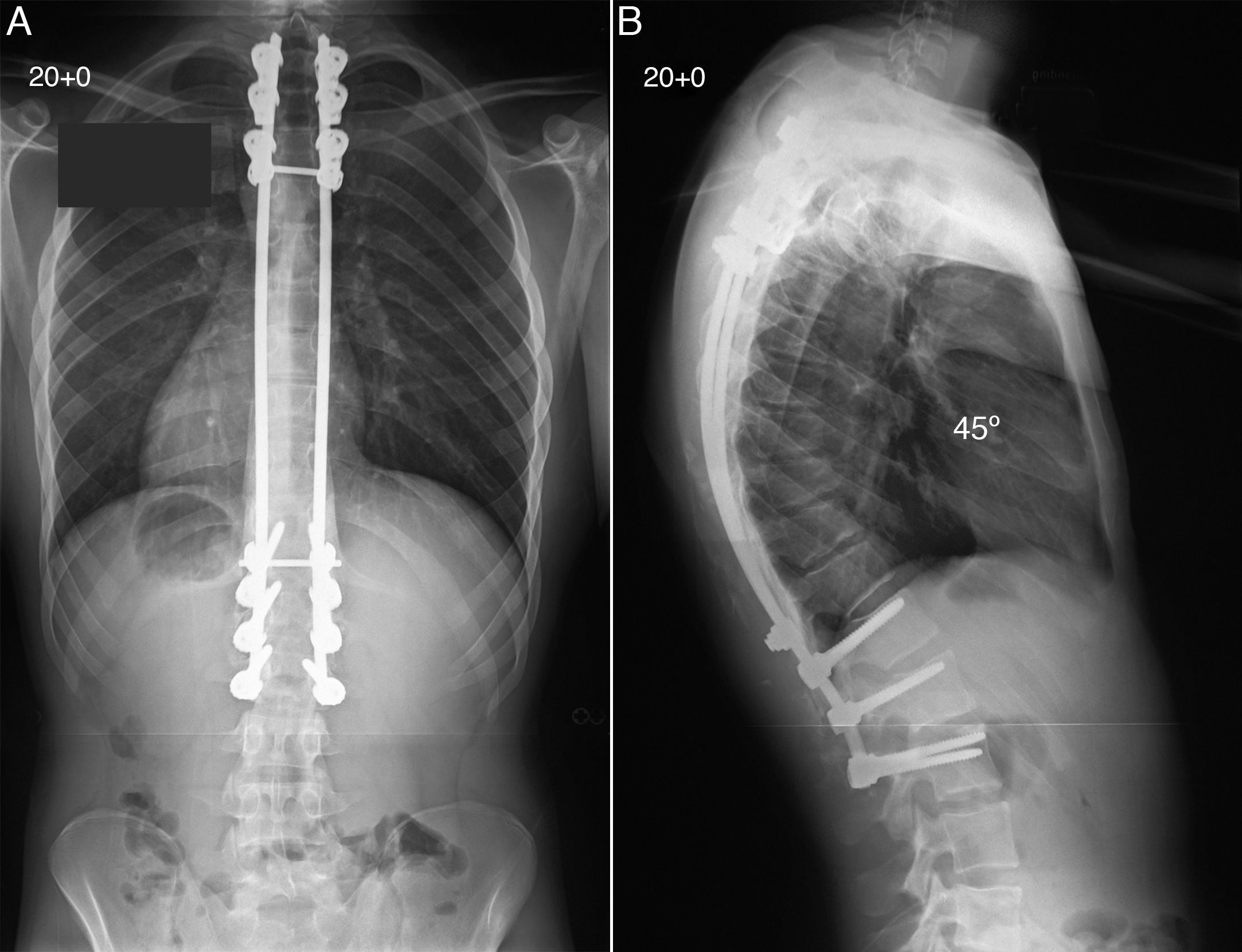
In terms of instrumentation, we employed a configuration with 2 bars, cranial fixation by pedicle hooks in 3–4 fixation levels, caudal fixation in 3–4 levels through transpedicular screws, and 2 transverse connections, 1 cranial and 1 caudal, between both bars (Fig. 5). We also performed segmental osteotomies in all levels between the cranial and caudal fixing points. The absence of vertebral instrumentation in the osteotomy levels provided a wide area in which to place abundant bone graft. Vertebral instrumentation, hooks and transpedicular screws were placed before performing the osteotomies. Next, the bars were moulded to the upper limit of kyphosis (45–50°) and normal lordosis, in order to prevent overcorrection and subsequent kyphosis, cranial or caudal to the instrumentation. The bars were secured to the cranial hooks and joined with the transverse connectors before applying corrective forces on the lever arm of both bars in a caudal direction, and reducing them on the caudal transpedicular screws. We subsequently conducted extensive decortication of the posterior spinal elements and placed the bone graft. We used autologous bone graft from the iliac crest to stimulate the formation of a solid bony arthrodesis. In the presence of hyperkyphosis, the bone graft received tension rather than compression forces, which represented an added mechanical disadvantage and an increased risk of pseudoarthrosis. During the 3 months following surgery, patients used a thoracolumbar support belt with suspenders in order to restrict spinal movements to some extent. Physical activities should also be avoided for a period of 6 months. In our experience, surgical correction of Scheuermann's disease obtains very high levels of patient satisfaction. Among the surgical procedures for the treatment of spinal deformity, this is one of the most rewarding for patients (Fig. 6).
The patient underwent posterior spine arthrodesis using pedicular hooks and transpedicular screws, as well as multiple segmental closing osteotomies, resulting in excellent correction of the thoracic kyphosis up to 45°, with an adequate balance in the coronal and sagittal spinal planes (A and B).
In order to reduce the risk of neurological complications, surgical correction of patients with Scheuermann's disease should be performed under spinal cord monitoring to collect motor evoked potentials (MEP) and somatosensory evoked potentials (SSEP). It is not infrequent for a decrease in the signal strength or even complete loss of spinal cord monitoring to occur while performing vertebral osteotomies or applying corrective forces on the lever arm for the final reduction and correction of hyperkyphosis. If irreversible neuromonitoring changes appear, surgical correction of the deformity should be released, instrumentation should be removed and the intervention should be concluded. An MRI should be obtained in the immediate postoperative period in order to rule out the presence of spinal cord compression or haematoma, even if patients do not show any evidence of neurological injury during the exploration.10,56 The procedure can be repeated after 7–10 days, once any possible spinal suffering becomes attenuated and the spine has recovered. During this time, patients should remain resting in bed. In these cases, the supine position will help to gradually and partially release the angular deformity, due to muscle relaxation and to the viscoelastic properties of the column. Cheh et al. published a retrospective study of 42 paediatric patients with hyperkyphosis who underwent surgical correction with vertebral osteotomies. The incidence of complete loss of mixed evoked potentials during surgery was 21.4%.57
ComplicationsThe analysis of complications published by the Morbidity and Mortality Committee of the Scoliosis Research Society on 683 surgical procedures for the treatment of Scheuermann's disease conducted between 2001 and 2004, reported a total incidence of complications of 14.5%. The most common complication was wound infection (3.8%), followed by implant-related complications (2.5%), acute neurological deficit (1.9%) and death (0.6%). The overall incidence of surgical complications was more common in adults (21.7%) compared with patients in their teens (11.8%). Other, less common complications were intestinal obstruction, intra/postoperative implant failure, pseudoarthrosis or nonunion, implant protrusion, progression of kyphosis, haemothorax, pneumothorax, pulmonary embolism and back pain.3,7,17,32,40,41,46,56,58–60 Performing surgery under conditions of hypotension and the use of blood salvage proved useful in reducing intraoperative blood loss and reducing the need for blood transfusion.
Selection of fixation levelsDespite it being known that a short arthrodesis will result in persistence or recurrence of the deformity,45 the correct selection of levels to include in the arthrodesis remains one of the critical points in surgical planning and correction, as there is no consensus on which are the optimal levels of fixation.3,49,60 The development of a kyphosis which is cranial or caudal to the arthrodesis has recently been investigated. Cranial kyphosis to the arthrodesis is defined as the presence of a cranial sagittal angle greater than 10° between the plate of the most cranial vertebra included in the fusion (the first vertebra included in the fusion) and that immediately superior to it. Similarly, caudal kyphosis to the arthrodesis is defined between the most caudal vertebra included in the fusion (the last vertebra included in the fusion) and that immediately inferior to it.60 In a multicentre study with 78 patients, Lonner et al.46 reported an incidence of kyphosis cranial to the arthrodesis of 32.1% in a range between 11° and 25°, and of kyphosis caudal to the arthrodesis of 28% in a range between 17° and 28°.
Patients with Scheuermann's disease often present a negative, overall, sagittal balance due to the development of an exaggerated, compensatory lumbar lordosis. The development of kyphosis cranial or caudal to arthrodesis due to incorrect selection of the levels to be included in the instrumentation may effectively worsen an already negative sagittal balance.32,46,49 This could result in the appearance of pain on cranial or caudal levels to the instrumentation or the prominence of implants, requiring review surgery. In order to maintain or achieve overall sagittal balance after correction of the hyperkyphosis, the cranial and caudal levels of the instrumentation must be located within the centre of gravity. An overcorrection of thoracic hyperkyphosis may result in the persistence of a negative, sagittal balance, which could eventually lead to the development of a cranial kyphosis to the arthrodesis. A caudal extension of the instrumentation to include the first disc in lordosis would enable better control of the lumbar lordosis, which could then prevent the development of a cranial kyphosis to the arthrodesis.
The latest recommendations about optimal levels to include in the arthrodesis advocate including the final cranial vertebra of the kyphosis within the instrumentation, along with the caudal, sagittal, stable vertebra, which is defined as the vertebra whose vertebral body is intersected by the vertical line traced from the posterosuperior corner of the sacral plate.45,46 Limiting the correction of hyperkyphosis to 50% or less of the original deformity is recommended, in order to prevent the development of kyphosis cranial to the arthrodesis.32 It is also important to maintain the integrity of the interspinous ligament and the yellow ligament between the most cranial vertebra included in the instrumentation and that immediately superior to it. Therefore, placing sublaminar hooks or wires as a method of cranial fixation could predispose to the development of kyphosis cranial to the arthrodesis, so they should be avoided.61 If cranial fixation of clamp-shaped instrumentation is being planned, this can be achieved through bilateral placement of hooks in the costotransverse apophyses, in order to preserve the integrity of the interspinous space. Current instrumentation techniques use hooks, screws and rods to obtain and maintain the desired correction.
The overall, sagittal balance of the spine is intimately related to the spatial location of the pelvis and shows a wide variability among individuals. The ultimate goal of treatment should be to achieve or maintain a correct alignment of the head over the pelvis. To date, there is a clear lack of studies describing and correlating spinal and pelvic parameters in patients with Scheuermann's disease before and after treatment. Such studies could help to establish a standard calculation of the optimal levels of deformity correction for each individual.
Level of evidenceLevel of evidence V.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Tomé-Bermejo F, Tsirikos AI. Conceptos actuales sobre la enfermedad de Scheuermann: presentación clínica, diagnóstico y controversias sobre su tratamiento. Rev Esp Cir Ortop Traumatol. 2012;56:491–505.