To compare the results obtained with computer assisted surgery with conventional techniques and evaluate the influence of navigation at different levels of preoperative deformity.
Materials and methodA retrospective study was conducted on 100 cases with primary total knee arthroplasty performed with conventional or computer assisted surgery. A comparison was made of the post-operative mechanical axis of the lower limb between both groups and in terms of pre-operative deformity.
ResultsOptimal alignment is most often obtained by using the navigation system (62%) than by a conventional technique (36%). Patients with deformities under 10° varus showed a mean post-operative alignment within the optimal range (0±3° deviation from the neutral mechanical axis), while those with more than 15° of varus show an alignment out of range, regardless of the technique used (p=.002). In those with a deformity of between 10° and 15° of pre-operative varus alignment, values were found closer to the neutral axis in the navigation group (178.7°) than in the conventional technique (175.5°), although these differences are not statistically significant (p=.127).
ConclusionPost-operative alignment obtained with navigation is better than with the conventional technique, with a smaller percentage of cases out of range, and greater accuracy in placing implants. A potential benefit was observed in navigation for cases with deformities of between 10° and 15° of varus.
Conocer los resultados obtenidos con cirugía asistida por ordenador en nuestro medio en comparación con las técnicas convencionales y analizar la influencia de la navegación ante distintos grados de deformidad preoperatoria.
Material y métodoEstudio retrospectivo con 100 pacientes intervenidos de artroplastia total de rodilla mediante técnica convencional y cirugía asistida por ordenador. Se comparó el eje mecánico postoperatorio del miembro inferior en carga entre ambos grupos y en función de la deformidad preoperatoria de cada caso.
ResultadosSe obtiene una alineación óptima con mayor frecuencia al utilizar el sistema de navegación (62%) que mediante una técnica convencional (36%). Los pacientes con deformidades menores de 10° de varo presentaron una media de alineación postoperatoria dentro del intervalo óptimo (0±3° de desviación del eje mecánico neutro) mientras que aquellos con más de 15° de varo muestran una alineación fuera de rango, independientemente de la técnica empleada (p=0,002). En aquellos con una deformidad de entre 10 y 15° de varo preoperatoria los valores de alineación se encontraron más próximos al eje neutro en el grupo de la navegación (178,7°) que en el de técnica convencional (175,5°), aunque estas diferencias no son estadísticamente significativas (p=0,127).
ConclusiónLa alineación postoperatoria obtenida con la navegación es mejor que con la técnica convencional, con un menor porcentaje de casos fuera de rango y una mayor precisión en la colocación de los implantes. Se observa un potencial beneficio de la navegación para aquellos casos con deformidades de entre 10 y 15° de varo.
Postoperative alignment of the lower limb is a factor with a considerable relevance in determining long-term survival of a total knee arthroplasty. A wrong positioning of the components conditions an asymmetric load distribution, giving rise to an increase in the risk of aseptic loosening, instability and pain.1 In this regard, computer-assisted surgery (CAS) systems have been developed with the aim of providing greater precision to this procedure and reducing the percentage of cases with malalignment, which should translate into a decrease of the failure rates, along with an increase in implant survival. In addition, CAS offers intraoperative information in real time about the condition of the ligaments and the kinematic arch of the knee.2 Numerous works have been published so far comparing the results obtained with conventional instrumentation techniques versus those obtained through the use of surgical navigation techniques, mainly regarding postoperative alignment and, more recently, on clinical and functional parameters. The results achieved show considerable variability, ranging from those favorable to navigation3–15 to others which found no differences between both methods,16–24 so this is a controversial topic. Some authors have also argued in favor of the potential benefit that these systems could offer in cases with significant intra- and extraarticular deformities, in which restoring a neutral postoperative alignment correctly is much more complex.13 However, the degree of deformity at which the use of these systems would offer an advantage over conventional instrumentation has not been established.
The objective of this work is to establish the clinical and functional results, as well as those obtained in terms of radiographic alignment in the coronal plane, obtained with CAS in our medium compared to conventional techniques and to analyze the influence of navigation in different levels of preoperative frontal deformity.
Materials and methodsWe conducted a retrospective cohort study with 100 patients who suffered knee arthrosis and underwent primary total knee arthroplasty at our center between June 2009 and March 2011. Out of this total, 50 had been operated using a conventional technique and the other 50 with the aid of computer-assisted navigation systems. The sample size for a cohort study was calculated based on the results of the most recent metaanalysis,25 according to which 13% of the navigation prostheses were outside the desired interval of ±3° of the mechanical axis. Based on a relative risk of detection of 0.35, with an α error of 0.5 and β of 0.8, we established a minimum sample size of 100 cases (50 in each group, upon establishing a ratio of 1 exposed/not exposed). This calculation was conducted with the software package Epidat version 4.0. Case selection was carried out by reviewing, consecutively and following a chronological order, all those patients intervened for total knee arthroplasty in the given period. We included patients operated for primary total knee prosthesis with a Genesis II model (Smith &Nephew®, Memphis, Tennessee, USA) – both the design with conservation of the posterior cruciate ligament (cruciate retained, CR) and the posterior stabilized, (PS) –, with an evolution of at least 1 year, regardless of age, presence of extra- or intraarticular deformities, and prior surgical interventions. As exclusion criteria we established not presenting full postoperative monitoring during the first year; reconversion of an initially navigated procedure into conventional during the intervention; existence of a prior indication of the technique to employ, either conventional or navigated surgery, due to the patient presenting specific characteristics that made one of the options preferable to the other. The study was approved by the Ethics Committee of the Biomedical Research Foundation at our hospital.
All the procedures were conducted by the 5 surgeons of the hip and knee arthroplasty unit. All of them had conducted a minimum of 200 conventional knee arthroplasty interventions previously, and between 10 and 15 navigation-assisted surgeries with the same software employed in every case in the study.
In our service, navigation was available 2 days per week; during the other 3 days we performed conventional techniques. The day of intervention of each patient was established by following the surgery waiting list. As indicated in the exclusion criteria, those patients in whom there was a specific reason that indicated one technique over another were excluded from the revision, so that all the cases finally included were assigned indistinctly to one group or the other. This procedure attempted to minimize a possible selection bias which could have taken place by the fact of having patients undergo one of the techniques for a specific reason.
The surgical procedures were carried out under ischemia, with a pneumatic cuff applied in the base of the thigh and removed at the end of the intervention, once the lower limb had been bandaged. We followed a standard approach in all cases, with incision in the midline and parapatellar medial arthrotomy with patellar eversion. We placed a Genesis II model (Smith & Nephew®, Memphis, Tennessee, USA) in all cases. We used both the CR and PS designs, implanting one or the other according to the criteria of each surgeon. The femoral CR component was implanted without cement, with 2 flex-lock anchors. The femoral and tibial PS components were cemented in all cases.
In the conventional surgery group we used intramedullary guides for the placement of the femoral component. Tibial alignment was established through extramedullary and/or intramedullary guides. In cases intervened with navigation, we used the BrainLab Knee Essential software system (BrainLab, Feldkirchen, Germany) for the Genesis II model. This system does not require prior images and is based on optic location (infrared light) with passive emitters. In this group we did not employ intramedullary guides in the femur or tibia.
We collected demographic data for each patient. As clinical parameters we registered the movement arc and the KSS questionnaire during the preoperative period and after 1 year. We evaluated the preoperative and postoperative mechanical axis in the frontal plane after 1 year evolution in full radiographs of the lower limbs under load. The value was calculated as the angle formed between a line from the center of the femoral head to the center of the knee joint, and another from the center of the knee to the center of the ankle joint. We considered as neutral a value of 180°; lower values represented varus deviations and higher values represented valgus deviations from the axis. We accepted postoperative mechanical angles of 180±3° as correct values.26 All the measurements were carried out by the same observer (a resident in the 5th year of service). With regard to the surgery, we registered the duration of surgery and ischemia.
After the data collection and treatment process we created a database in a Microsoft Excel file, where we recoded the variables. The statistical analysis of the data was carried out using the software package SPSS 20.0 (IBM, Chicago, Illinois, USA).
We used the Chi-squared test for the analysis of the categorized qualitative and quantitative variables, and used the exact Fisher test when the expected frequency was less than 5 in over 20% of the fields. For the quantitative variables we carried out an analysis of normality through the Shapiro–Wilk test. When these followed a normal distribution we applied parametric tests, like the Student t test, to compare samples (for independent data and paired data). For variables that did not follow a normal distribution we applied nonparametric tests, like the Mann–Whitney U test, to compare means.
The ANOVA test was used for comparison of means of the postoperative mechanical axes between the different preoperative mechanical axis groups and the 2 surgical techniques employed. Next, after verifying the homogeneity of variances, we conducted a posteriori (post hoc) comparisons using the Tukey method.
The size of the response to the clinical variables of “flexion” and “extension”, as well as the scores of the KSS questionnaires before and after the surgery, were measured according to the statistics of size of the effect and the standardized mean of the response. We could state that this magnitude was clinically relevant with values over 0.8.27
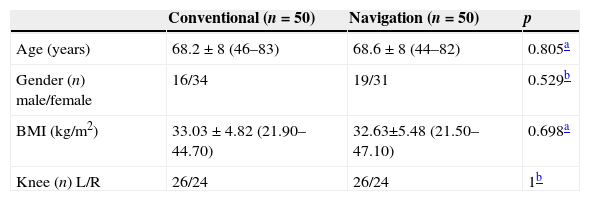
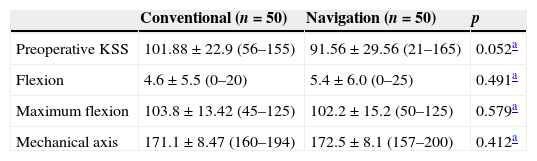
ResultsTable 1 shows the demographic data of the patients included in the study. No statistically significant differences were observed between both groups in terms of age, gender, BMI and laterality of the operated knee, so we assumed that the 2 groups were homogeneous regarding these factors. Neither did we find differences in the preoperative radiographic and clinical data of both groups (Table 2).
Descriptive analysis of the variables age, gender, BMI and operated side.
| Conventional (n=50) | Navigation (n=50) | p | |
|---|---|---|---|
| Age (years) | 68.2±8 (46–83) | 68.6±8 (44–82) | 0.805a |
| Gender (n) male/female | 16/34 | 19/31 | 0.529b |
| BMI (kg/m2) | 33.03±4.82 (21.90–44.70) | 32.63±5.48 (21.50–47.10) | 0.698a |
| Knee (n) L/R | 26/24 | 26/24 | 1b |
BMI: body mass index; L: left; R: right.
Values are given as mean and standard deviation, with the interval in brackets.
Descriptive analysis of the preoperative variables: KSS score, flexion and maximum flexion, and mechanical axis.
| Conventional (n=50) | Navigation (n=50) | p | |
|---|---|---|---|
| Preoperative KSS | 101.88±22.9 (56–155) | 91.56±29.56 (21–165) | 0.052a |
| Flexion | 4.6±5.5 (0–20) | 5.4±6.0 (0–25) | 0.491a |
| Maximum flexion | 103.8±13.42 (45–125) | 102.2±15.2 (50–125) | 0.579a |
| Mechanical axis | 171.1±8.47 (160–194) | 172.5±8.1 (157–200) | 0.412a |
Values are given as mean and standard deviation, with the interval in brackets.
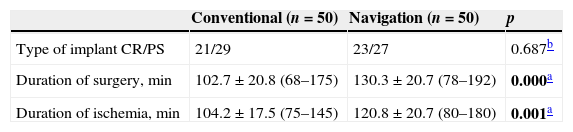
Regarding the duration of surgery, both the time of the surgery and of ischemia were significantly higher in the navigation-assisted surgery group, with a mean difference in surgery time of 27.5min (95% CI: 19.2–35.9min), and 16.3min in ischemia time (95% CI: 6.4–26.1min). The distribution of CR and PS implants was similar in both groups (Table 3).
Comparative analysis between the type of implant, duration of surgery and duration of ischemia.
| Conventional (n=50) | Navigation (n=50) | p | |
|---|---|---|---|
| Type of implant CR/PS | 21/29 | 23/27 | 0.687b |
| Duration of surgery, min | 102.7±20.8 (68–175) | 130.3±20.7 (78–192) | 0.000a |
| Duration of ischemia, min | 104.2±17.5 (75–145) | 120.8±20.7 (80–180) | 0.001a |
For the variables of duration of surgery and duration of ischemia, values are given as mean and standard deviation, with the interval in brackets.
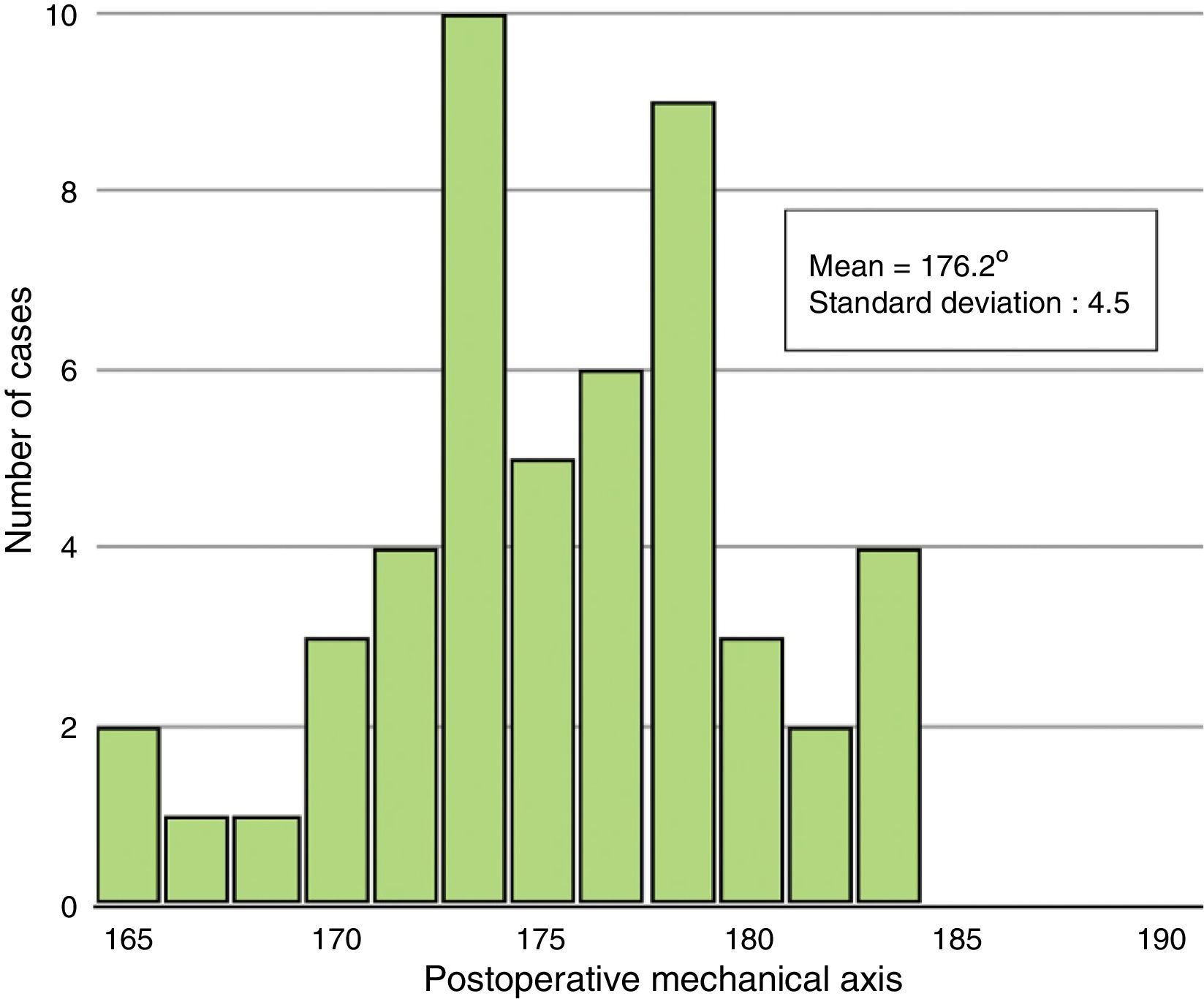
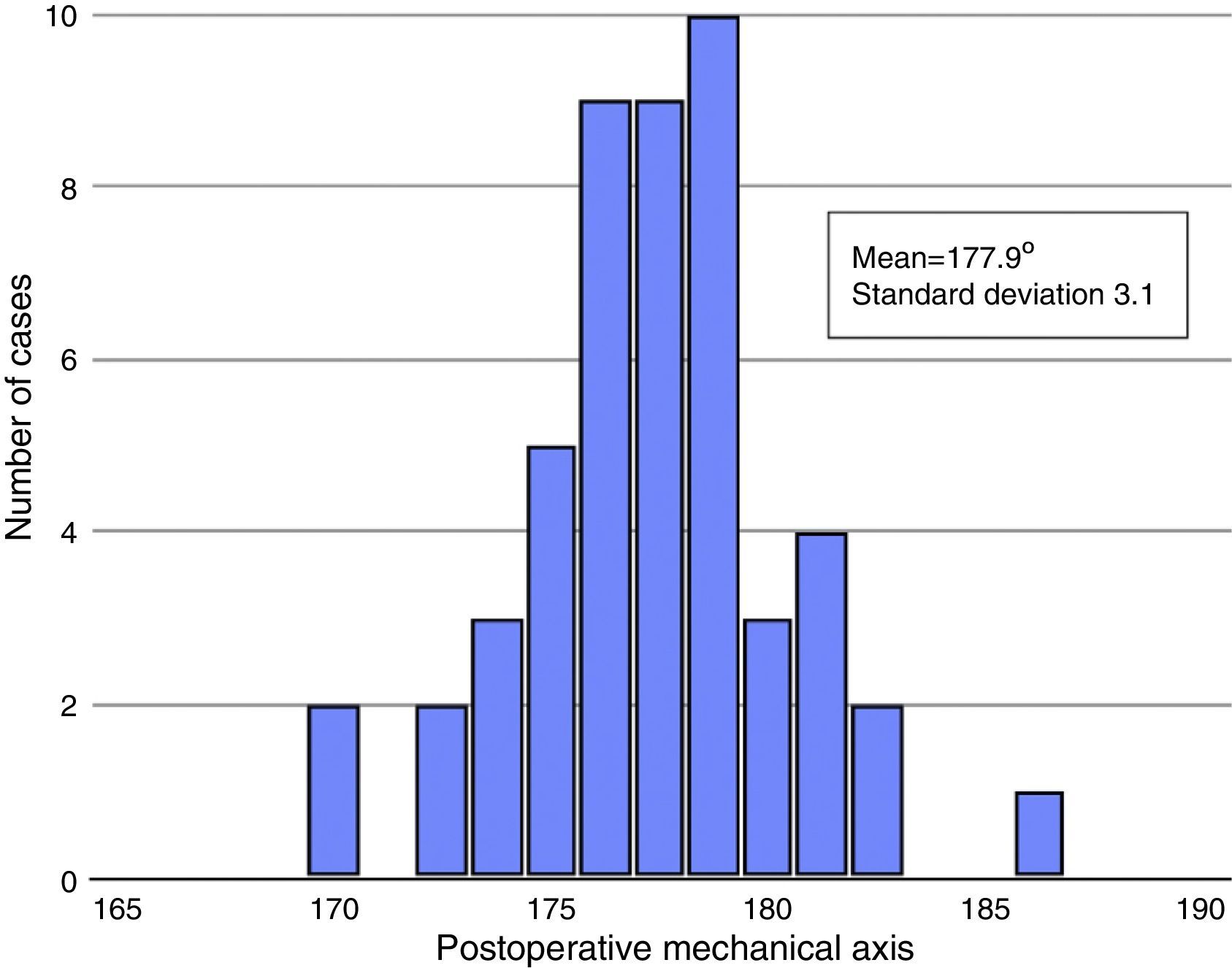
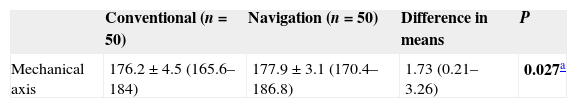
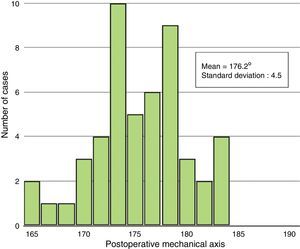
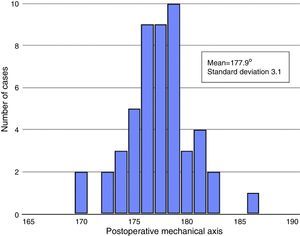
Regarding the postoperative data, when we analyzed the alignment of the lower limb we found significant differences between the mechanical axes, with values that were closer to those accepted as optimal (180° for the mechanical axis) in the navigation group (Table 4). The dispersion was less in this group, in both cases showing lower standard deviations than the conventional group, as shown in graphic format by the frequency histograms (Figs. 1 and 2). In addition, the percentage of cases with a correct alignment was significantly higher in the group of patients intervened with navigation, with 62%, whereas this was only true in 36% of cases intervened following the conventional technique (p=.009).
Analysis of the postoperative mechanical axis.
| Conventional (n=50) | Navigation (n=50) | Difference in means | P | |
|---|---|---|---|---|
| Mechanical axis | 176.2±4.5 (165.6–184) | 177.9±3.1 (170.4–186.8) | 1.73 (0.21–3.26) | 0.027a |
Values are given as mean and standard deviation, with the interval in brackets.
Mechanical axis: values over 180° indicate valgus, whilst values under 180° indicate varus.
Difference in means, with 95% confidence interval in brackets.
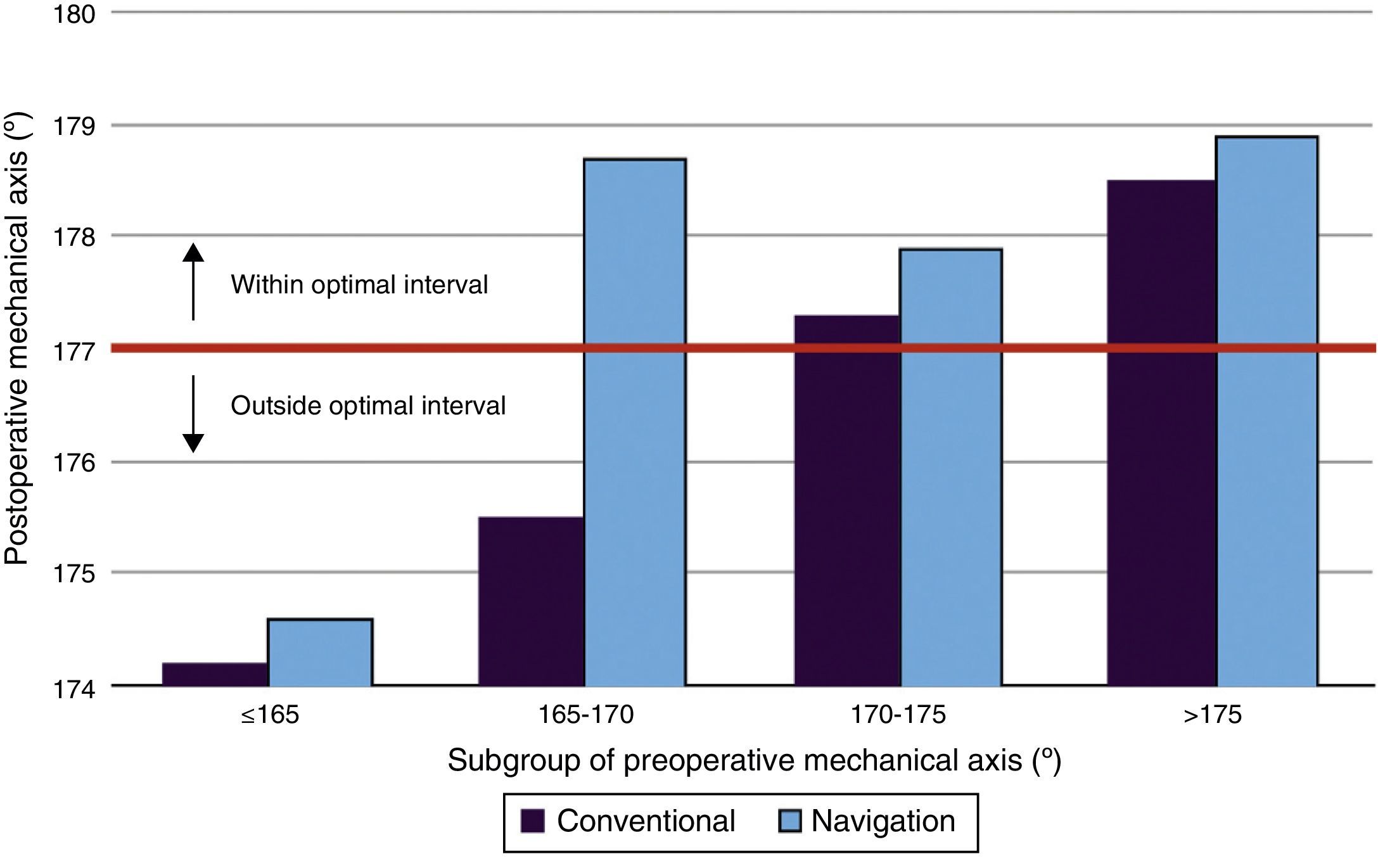
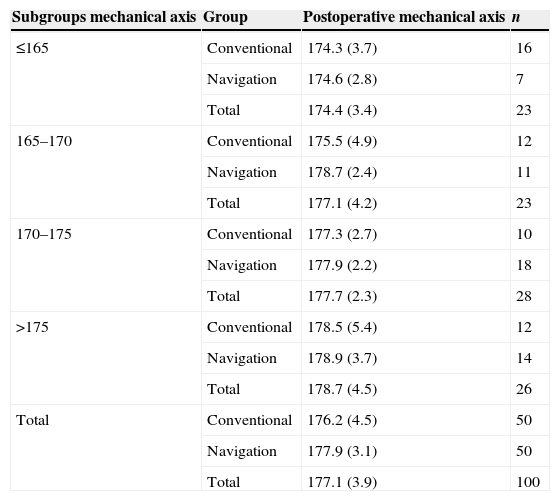
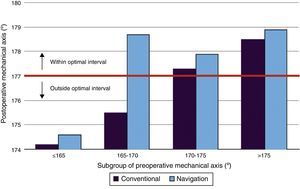
In order to conduct an in-depth analysis of the alignment data we divided the patients into 4 subgroups based on the preoperative value of the mechanical axis, taking as cutoff points the values of the 25, 50 and 75 percentiles, and we studied whether preoperative deformity determined postoperative alignment, as well as the influence of the surgical technique employed (Table 5). This was done by means of an ANOVA test. This test found significant differences between the mean values of the postoperative mechanical axis between the different groups of preoperative mechanical axis (p=.002); but not between the 2 types of surgical techniques (p=.127), and it was not possible to demonstrate the existence of an interaction between both factors (preoperative deformity and surgical technique employed) (p=.486). Subsequent comparisons using the Tukey method found that patients with a preoperative deformity greater than 15° had a postoperative alignment which was further from the neutral axis than patients with a deformity smaller than 10°, regardless of the surgical technique employed (p=.009 and p=.001). Nevertheless, it is notable that within this group patients who underwent navigation-assisted surgery presented a better alignment despite not reaching statistical significance, as previously mentioned (Fig. 3).
Descriptive analysis of the variable postoperative mechanical axis in the different subgroups of preoperative mechanical axis.
| Subgroups mechanical axis | Group | Postoperative mechanical axis | n |
|---|---|---|---|
| ≤165 | Conventional | 174.3 (3.7) | 16 |
| Navigation | 174.6 (2.8) | 7 | |
| Total | 174.4 (3.4) | 23 | |
| 165–170 | Conventional | 175.5 (4.9) | 12 |
| Navigation | 178.7 (2.4) | 11 | |
| Total | 177.1 (4.2) | 23 | |
| 170–175 | Conventional | 177.3 (2.7) | 10 |
| Navigation | 177.9 (2.2) | 18 | |
| Total | 177.7 (2.3) | 28 | |
| >175 | Conventional | 178.5 (5.4) | 12 |
| Navigation | 178.9 (3.7) | 14 | |
| Total | 178.7 (4.5) | 26 | |
| Total | Conventional | 176.2 (4.5) | 50 |
| Navigation | 177.9 (3.1) | 50 | |
| Total | 177.1 (3.9) | 100 |
Values are given as mean and standard deviation (in brackets).
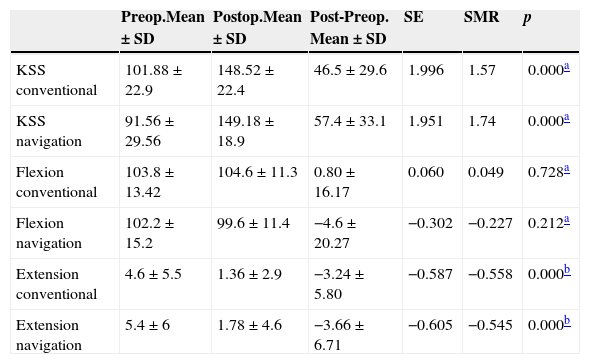
Regarding the clinical data, when comparing the pre- and postoperative results we observed that patients in both groups presented an improvement in their KSS scores and degree of extension. However, looking at the values of the statistics describing the size of the effect and the standardized mean of the response we can say that the magnitude of the improvement was only clinically significant in terms of the KSS scores for both groups. Nevertheless, we did not find significant differences (p=.094) when comparing the means of the differences of the total KSS scores between both groups, so we cannot state that the increase in KSS scores was significantly higher in one group compared to the other (Table 6).
Comparison of the pre- and postoperative results of the KSS scores, flexion and extension.
| Preop.Mean±SD | Postop.Mean±SD | Post-Preop. Mean±SD | SE | SMR | p | |
|---|---|---|---|---|---|---|
| KSS conventional | 101.88±22.9 | 148.52±22.4 | 46.5±29.6 | 1.996 | 1.57 | 0.000a |
| KSS navigation | 91.56±29.56 | 149.18±18.9 | 57.4±33.1 | 1.951 | 1.74 | 0.000a |
| Flexion conventional | 103.8±13.42 | 104.6±11.3 | 0.80±16.17 | 0.060 | 0.049 | 0.728a |
| Flexion navigation | 102.2±15.2 | 99.6±11.4 | −4.6±20.27 | −0.302 | −0.227 | 0.212a |
| Extension conventional | 4.6±5.5 | 1.36±2.9 | −3.24±5.80 | −0.587 | −0.558 | 0.000b |
| Extension navigation | 5.4±6 | 1.78±4.6 | −3.66±6.71 | −0.605 | −0.545 | 0.000b |
SD: standard deviation; SE: size of the effect; SMR: standardized mean of the response.
Values are given as mean and standard deviation (in brackets).
Therefore, we can say that both groups presented a significant and clinically relevant improvement in their KSS scores, albeit without that increase being significantly higher in one group compared to the other.
DiscussionIn our series, optimal alignment of the lower limb was achieved more frequently by using the computer-assisted navigation system (62%) instead of a conventional technique (36%).
The first prospective study comparing the conventional technique and navigation in total knee arthroplasty took place in 2001. In it, Mielke et al.16 reported finding no differences between both techniques in terms of the alignment of the lower limb, using as reference the measurement of the mechanical axis. Since then, there have been numerous works along the same lines which have offered highly variable results.
Several studies have proven that navigation systems contribute to achieve a better positioning of the prosthetic components and a better alignment of the lower limb, whilst also finding, coinciding with our results, a higher percentage of cases with a mechanical axis within an interval considered as optimal (±3° regarding the neutral mechanical axis).3,8–15,28 The high percentage of cases within the normal range obtained with both navigation-assisted techniques and conventional surgery are striking compared with our series. In many of these works, optimal postoperative alignment was achieved in around 95% of cases in groups undergoing navigation-assisted surgery, whereas in our study this figure was only 62%. Likewise, the rates of patients with a correct alignment following conventional surgery were very high, around 75%, compared to 38% in our series. Only Maculé-Beneyto et al.,10 in their multicenter work, found results which were lower than ours, with 29% of cases with a correct final alignment after conventional surgery and 48% in the navigation group.
However, other authors have not been able to demonstrate significant differences regarding postoperative alignment between these 2 types of surgical techniques.16–24 Likewise, the percentages of patients with a correct postoperative mechanical axis (0±3°) reported by these studies are high, over 80% in the navigation group in most of the works; and between 70% and 80% in the groups where navigation was not employed, even higher than our rate of patients in the navigation-assisted surgery group with a postoperative mechanical axis within the optimal range.
We also found differences between the means of the mechanical axis with values closer to those accepted as optimal in the navigation group. However, the difference of means of the mechanical axis was only of 1.73°, and although statistically significant, the clinical relevance of such a small difference is questionable.
Not only does the difference of means in the mechanical axis favor navigation-assisted surgery, but also the distribution of these variables shows less dispersion in this group, with standard deviations for the postoperative mechanical axis of 4.5° in the conventional surgery group and of 3.1° in the navigation group, thus indicating that we achieved greater precision with navigation than with conventional techniques.
However, the difference between one technique and the other is of just a few degrees, which is within the range of imprecision of the measurements caused by intra- and interobserver variability, as well as projection errors of the radiographs.29 Huang et al.30 found that the measurement of the mechanical axis has a variability of between 1° and 3°. However, this error may be greater in situations in which it is difficult to position patients correctly at the time of obtaining the radiograph, as in the case of obese patients and those with severe deformities in flexion. According to Krackow et al.,29 the artifact produced with a rotation and flexion under 10° is lower than 2°. However, the changes become relevant with values between 10° and 20°, with variations around 7° in the alignment of the lower limb. In 2007, Brouwer et al.31 validated the results published by Krackow et al. in cadaver studies, in which they found that both rotation without flexion and flexion without rotation caused minimal changes in the angles projected on a radiograph. However, the combination of 15° external rotation and 15° flexion produces an apparent varus deformity of 4°.
On one hand, some authors have supported that navigation is especially interesting for patients with significant intra-13 and extraarticular32 deformities, in whom bone loss and ligamentous lesions hinder the restoration of correct alignment and stability using conventional techniques and instruments. In particular, Sorrells et al.33 found that those cases with a preoperative alignment with more than 10° varus or valgus had a higher probability of presenting postoperative alignment outside the ranges considered as optimal. For this reason, we studied the relationship between preoperative alignment and the type of technique employed in surgery with postoperative alignment, and observed that patients with preoperative deformities lower than 10° varus presented a mean postoperative alignment within the correct interval regardless of the technique used, whereas patients with a preoperative varus of 15° or more presented an alignment outside the mean range, also regardless of the technique employed. However, we did notice a trend toward presenting better postoperative alignment among those patients with preoperative varus between 10° and 15° who were intervened with a navigation-assisted technique versus those who underwent a conventional technique (178.7 versus 175.5), although the differences did not reach statistical significance. If this trend were confirmed, these results could indicate that perhaps navigation would be able to “rescue” those patients with a preoperative varus alignment within 10° and 15°. This group would be the one that could benefit the most from the use of navigation systems. In their study, Hernández Vaquero et al.13 compared both surgical techniques in patients with a mechanical axis over 10° and in patients with an axis under 10°, and in both cases obtained a better final alignment with the use of navigation. These authors argued that perhaps the most important role that surgical navigation could have in arthroplasty would be in cases of complex knees which presented significant deformities or when mechanical alignment could not be used, thus representing an alternative to traditional instrumentation in trying to achieve an effective treatment of these patients.
The clinical and functional evaluation was based on the scores obtained in the KSS questionnaire, as well as the degree of flexion and extension of the knee. As far as we could discern, none of the works published to date has reported the size of the effect or the standardized mean response, so we were unable to compare the magnitude of the improvement observed in our study with that obtained by these works. Our results coincide with the majority of those published in the sense that all find an improvement in the scores of the different questionnaires used, and specifically of the KSS, but this improvement was similar in both groups, with no significant differences being found in the final scores between the conventional surgery and navigation groups. Only Hoffart et al.24 found better postoperative scores in the navigation group, both in the total KSS and in the clinical and functional sections. Unlike them, Schmitt et al.34 not only did not find differences, but in fact found that the conventional surgery group had a higher score in the postoperative functional KSS (94.1) than the 2 groups of navigation-assisted surgery with which it was compared (85.6 and 76.3), based upon similar preoperative scores. Likewise, different metaanalyses have concluded that the use of CAS does not help to improve postoperative function in total knee arthroplasties.25,35
We identified a series of limitations in the present work. Firstly, we should bear in mind that this was a retrospective study in which the patients were included after being intervened and were chosen among a group of patients based on the criteria described previously. In this type of studies it is common to have some selection bias which affects the inclusion or exclusion of patients, thus there is a risk that the sample selected is not representative of the population extracted. We attempted to diminish that error insofar as possible by including patients consecutively in the dates indicated until the desired sample size was reached, as long as the relevant complementary tests were obtained, essentially teleradiographs. However, not all surgeons in the team request this test during the preoperative study, as is the case in routine monitoring, so some patients who did not have it could not be included in the study. Neither did we include those in whom some specific reason indicated a specific technique, thus attempting to avoid selecting patients in whom one technique was more advantageous than the other given their specific conditions.
Another limitation was that the selected sample size was calculated in order to adjust to the comparative analysis of the alignment of the postoperative mechanical axis between the 2 surgical technique groups. However, when delving into an analysis by subgroups, the number of cases was reduced and so the statistical analysis lost some power. In addition, since cases presenting preoperative varus deformity were predominant, we were not able to analyze the results of navigation in different subgroups of valgus deviation.
On the other hand, since all radiographic measurements were conducted by a single observer, it was not possible to compare intra- and interobserver variability.
We can conclude that navigation has led to better results in terms of postoperative alignment, with a lower percentage of cases outside the range and better precision in the placement of implants.
Overall, patients with preoperative deformities greater than 10° had a better postoperative alignment than those with deformities greater than 15° regardless of the technique employed. However, among those cases with a preoperative mechanical axis within 10° and 15° varus, the use of navigation systems seemed to produce a better postoperative alignment.
Level of evidenceLevel of evidence II.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Benavente P, López Orosa C, Oteo Maldonado JA, Orois Codesal A, García Lázaro FL. Cirugía asistida por ordenador. Su utilidad en distintos grados de deformidades preoperatorias. Rev Esp Cir Ortop Traumatol. 2015;59:245–253.