Unstable forearm fractures may require surgical management by reduction and osteosynthesis with intramedullary needles. This fixation should be removed early if it has been left exposed, but this could increase the risk of refracture in a bone in the period of remodelling. As an alternative we can keep the needles, buried subcutaneously, for a longer time, to protect the bone callus.
ObjectiveTo assess whether there are differences between using exposed needles with respect to burying them in paediatric patients with forearm fractures. Our hypothesis is that by burying the needles we keep them longer by reducing forearm refractures.
Material and methodsWe present a cohort of 75 paediatric patients with a forearm fracture between 2010 and 2016. Demographic data, surgical technique, complications and patient follow-up were collected.
ResultsThe implants were left exposed in 50 patients and 25 buried. The average time of removal of the exposed implants was 6.8weeks and 17.6weeks in the buried ones. No significant differences were found in terms of consolidation (p=0.19) or immobilisation time (p=0.22). Regarding refractures, a greater number was observed in the exposed osteosynthesis group (4 patients) compared to only one case with buried osteosynthesis, but there were no significant differences (p=0.49). No postsurgical complications were detected and the functionality was excellent at the end of the follow-up in both groups.
ConclusionLeaving implants buried in relation to skin exposed does not cause a decrease in the number of refractures or other complications, with adequate patient functionality in both cases.
Las fracturas inestables de antebrazo pueden requerir un manejo quirúrgico mediante reducción y osteosíntesis con agujas intramedulares. Esta fijación debe retirarse precozmente si se ha dejado expuesta, pero esto podría aumentar el riesgo de refracturas sobre un hueso en periodo de remodelado. Como alternativa podemos mantener durante más tiempo las agujas, enterradas a nivel subcutáneo, para proteger el callo óseo.
ObjetivoValorar si hay diferencias entre utilizar agujas expuestas respecto a enterrarlas en pacientes pediátricos con fracturas de antebrazo. Nuestra hipótesis es que al enterrar las agujas las mantenemos más tiempo reduciendo las refracturas de antebrazo.
Material y métodosPresentamos una cohorte de 75 pacientes pediátricos con fractura de antebrazo entre 2010 y 2016. Se recogieron datos demográficos, técnica quirúrgica, complicaciones y seguimiento del paciente.
ResultadosLos implantes se dejaron expuestos en 50 pacientes y 25 de forma enterrada. El tiempo medio de retirada de los implantes expuestos fue de 6,8semanas, y de 17,6semanas en los enterrados. No se hallaron diferencias significativas en cuanto a consolidación (p=0,19) ni en tiempo de inmovilización (p=0,22). Respecto a las refracturas, se observa un mayor número en el grupo de la osteosíntesis expuesta (4pacientes) respecto a solo un caso con osteosíntesis enterrada, pero sin llegar a presentar diferencias significativas (p=0,49). No se detectaron complicaciones posquirúrgicas y la funcionalidad fue excelente al final del seguimiento en ambos grupos.
ConclusiónDejar los implantes enterrados respecto a expuestos a piel no condiciona una disminución en el número de refracturas ni otras complicaciones, con una adecuada funcionalidad del paciente en ambos casos.
Forearm fractures are highly common in paediatric patients. They account for a fourth of all fractures and around 40% of them are in the diaphyseal region.1,2 Closed reduction and stabilisation with a closed plaster cast continues to be the gold standard in the majority of stable forearm fractures.3 However, in open or highly unstable fractures, correct alignment needs to be maintained through surgical treatment with osteosynthesis of the fracture.4
With regards to surgical treatment of these fractures in paediatric patients, fixation with intramedullary pins is the method of choice, achieving good alignment and with appropriate radio ulnar stability and less posterior immobilisation time.5
This type of implant offers several advantages: less soft tissue aggression, shorter time in surgery, minimal surgical approach and easily extractable.6 Nevertheless, controversy exists as to whether the pins should be left exposed or buried, and regarding the time they should remain in the fracture region.
One of the regularly used options is to leave the implants exposed through the skin during surgery to facilitate their subsequent extraction, but this may lead to skin irritation and increase the risk of local infection or even eventual osteomyelitis.7 However, removal must be performed early during the first 4–8weeks after surgery. This is when the risk is greatest, since the majority of refractures present during the first 9 months after the initial lesion,8 and this period of bone formation and remodelling is what leads to an increase in the risk.9
In an attempt to reduce the number of refractures we may leave the osteosynthesis material embedded at subcutaneous level, which would prevent any complications of foreign endomedullary material coming into direct contact with the exterior, and at the same time would help us to keep the implants for longer, until the remodelling and formation process of bone callus is more advanced. The drawback of this method is that the implant has to be removed surgically, under general anaesthesia.
The objective of this study was to assess whether there were any differences between using exposed pins compared with leaving them embedded in paediatric patients with diaphyseal forearm fractures. Our main hypothesis was that embedding pins and keeping them for longer leads to better results, reducing forearm refractures. As a secondary objective, we assessed the complications and final functionality of the patients, since our secondary hypothesis was that embedded implants lead to fewer complications and local infections.
Materials and methodsA retrospective comparative review was performed of all paediatric patients aged between 1 and 15 years who had presented with forearm fracture which was treated using intramedullary fixation during the period between 2010 and 2017 in our centre.
The main cohort studied comprised 270 paediatric patients who had undergone fixation with pins or screws due to forearm fracture. Out of this group we proceeded to exclude patients with forearm fractures who had not presented with intramedullary fixation (96patients) and those patients whose follow-up was carried out in other hospitals (99patients). Finally, the group under study presented with a total of 75patients who met with the established criteria in our objective for analysis.
Initial diagnosis and patient management was performed in the emergency paediatric department of our hospital. Following diagnosis, the patient was admitted to our paediatric orthopaedic unit and underwent emergency surgery by an orthopaedic surgeon from the unit.
The surgical team followed the standard protocol for these fractures. After the administration of general anaesthesia, closed reduction of the fracture was performed and assessment of stability, taking into consideration the instability risk factors, such as over 50% movement, aged over 9 years, and a complete fracture of the radius with angulation above 15°.10 Once the fracture characteristics had been confirmed, if the surgeon considered the fracture was unstable, he proceeded with insertion of the osteosynthesis material, either with titanium elastic nails by Depuy Synthes®, Pedifexs by Orthopediatrics®) or steel Kirschner (AK) type pins. Following correct alignment, the implants were cut and folded embedding them at subcutaneous level (Fig. 1) or cut and left exposed outside the skin. After this a brachial plaster cast was applied for immobilisation.
Patient follow-up was made in the outpatients department of the paediatric orthopaedic unit where immobilisation and fracture consolidation time was recorded, in addition to the interval up to extraction of the osteosynthesis material (EOM), the place where EOM was performed and any complications. The final functionality of the patient and whether or not refractures had occurred was also recorded, with evaluation of parameters in these cases.
For functional evaluation a scale was used7,11 where final functionality of the patient was classified into 4 categories. These were excellent if there was no discomfort with forced activity and a loss of less than 15° of forearm rotation; good if there was discomfort with forced activity and a loss of 15–30° rotation; normal if there was discomfort with daily activity and loss of rotation of 30–90°, and poor with loss or rotation >90°.
Osteosynthesis material extraction was performed surgically or in the doctor's surgery, depending on the type of treatment and preferences of the surgeon who undertook follow-up.
Statistical analysisInitial analysis of the final cohort was performed with the age parameter using the Shapiro–Wilk test to verify normality and the Lilliefors (Kolmogorov–Smirnov) test, with a significant result in both cases being p<0.05, for which it was not possible to obtain an appropriate normal sample distribution.
The analytical study of qualitative parameters was performed using the exact Fisher test and that of quantitative data used the Wilcoxon test, Mann–Whitney U test or the Student's t test whenever appropriate. Findings from the statistical tests were considered significant when p<0.05.
Sample size analysis was performed from review of published data on complications in the treatment of fractures with osteosynthesis material presented by the paediatric patients. It was necessary to have a sample of at least 47 patients (with 23 patients in each group), with a statistical power of 80% and accepting an alpha error of 5%.
All statistical analyses were performed using the free software R Commander 3.4.3.
ResultsThe final study cohort comprised 75 patients from which two main groups of comparison were obtained, depending on whether they presented with exposed implants (50 patients who formed 66% of the total) or embedded ones (who represented the remaining 33% of patients).
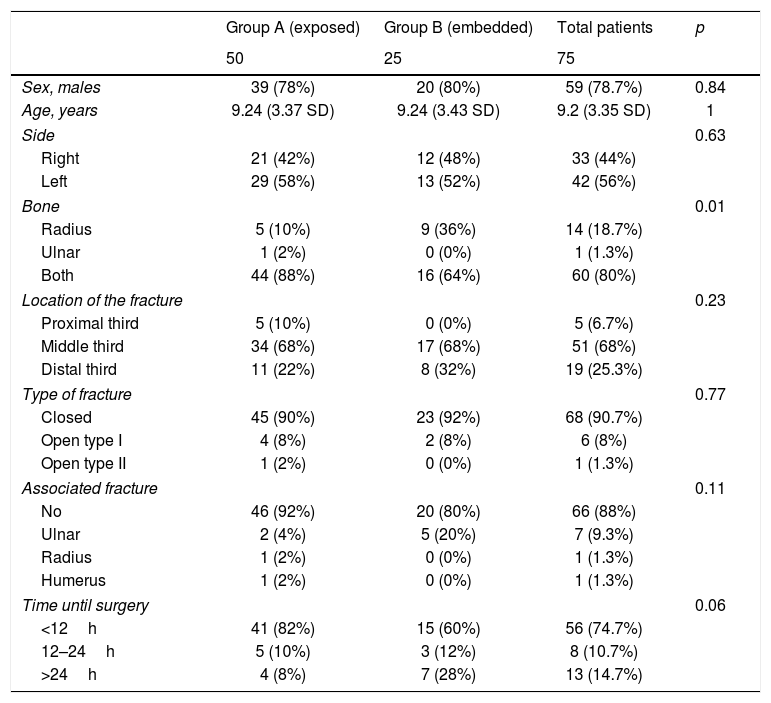
Baseline characteristics were collected from the patients (Table 1), including demographic data and main fracture characteristics, delay until surgical treatment and details of the same, together with any immediate complications.
Baseline demographic data.
| Group A (exposed) | Group B (embedded) | Total patients | p | |
|---|---|---|---|---|
| 50 | 25 | 75 | ||
| Sex, males | 39 (78%) | 20 (80%) | 59 (78.7%) | 0.84 |
| Age, years | 9.24 (3.37 SD) | 9.24 (3.43 SD) | 9.2 (3.35 SD) | 1 |
| Side | 0.63 | |||
| Right | 21 (42%) | 12 (48%) | 33 (44%) | |
| Left | 29 (58%) | 13 (52%) | 42 (56%) | |
| Bone | 0.01 | |||
| Radius | 5 (10%) | 9 (36%) | 14 (18.7%) | |
| Ulnar | 1 (2%) | 0 (0%) | 1 (1.3%) | |
| Both | 44 (88%) | 16 (64%) | 60 (80%) | |
| Location of the fracture | 0.23 | |||
| Proximal third | 5 (10%) | 0 (0%) | 5 (6.7%) | |
| Middle third | 34 (68%) | 17 (68%) | 51 (68%) | |
| Distal third | 11 (22%) | 8 (32%) | 19 (25.3%) | |
| Type of fracture | 0.77 | |||
| Closed | 45 (90%) | 23 (92%) | 68 (90.7%) | |
| Open type I | 4 (8%) | 2 (8%) | 6 (8%) | |
| Open type II | 1 (2%) | 0 (0%) | 1 (1.3%) | |
| Associated fracture | 0.11 | |||
| No | 46 (92%) | 20 (80%) | 66 (88%) | |
| Ulnar | 2 (4%) | 5 (20%) | 7 (9.3%) | |
| Radius | 1 (2%) | 0 (0%) | 1 (1.3%) | |
| Humerus | 1 (2%) | 0 (0%) | 1 (1.3%) | |
| Time until surgery | 0.06 | |||
| <12h | 41 (82%) | 15 (60%) | 56 (74.7%) | |
| 12–24h | 5 (10%) | 3 (12%) | 8 (10.7%) | |
| >24h | 4 (8%) | 7 (28%) | 13 (14.7%) | |
SD: standard deviation of the mean.
Data between brackets represent the percentage of the compared group.
Open fractures are classified according to the Gustilo classification.
There was a majority of males, who made up 78.7% of the total study patients and a mean age of 9.2years with a standard deviation (SD) of 3.35years, with no significant differences between the groups in both parameters. Regarding the bone most affected, differences were observed, with the fracture of both bones being the most prevalent.
In both groups a majority of closed fractures was observed, with a total of 68 subjects (90.7%), and only 9 patients (12%) presented with a fracture associated with that of the forearm. In this case there were no significant differences observed between the two study groups. The associated humeral fracture was a type II Garland supracondylar fracture, which was osteosynthesized during the same forearm operation. The associated forearm fractures presented with different diagnoses, with 3 plastic incurvations, 4 impellers and one greenstick fracture of the ulnar, all with characteristics of good stability and without the need to osteosynthesize them.
Regarding surgical characteristics, no significant differences were observed between the two groups with respect to surgical delay, but the majority (74.7%) were operated on within the first 24h. Mean time in surgery was 71.6min (30.4 SD), with no significant differences being observed between the two groups. With regard to fracture reduction, 77.3% of patients (58 subjects) were able to obtain correct closed reduction but the remainder required open reduction of both bones (12 patients, 16% of the total) or only the ulnar (4%) or radius (2.7%); however, no significant differences were found between the two groups compared. One or two osteosynthesis pins were used, depending on the characteristics of the fracture and its stability, but no differences were observed. Regarding surgical complications, one patient presented with a temporary lesion of the radial nerve which improved at the end of follow-up.
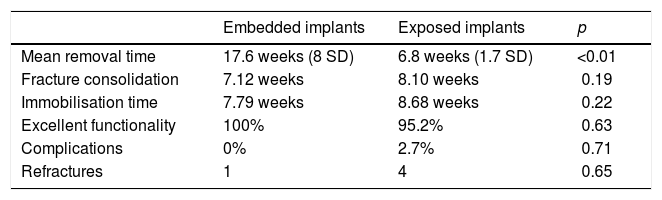
All patients were immobilised with a brachial plaster cast after surgery. The patients who had embedded pins presented with an immobilisation time of 7.79weeks and of 8.68weeks in the case of exposed pins, with no significant differences.
Mean fracture consolidation, assessed by X-ray, was 7.12 weeks in the case of embedded pins and 8.10 for exposed one, with no statistically significant differences were observed.
EOM was surgically performed on all the patients with embedded pins, whilst out of the patients with exposed pins, 28 patients had their removed in the surgeon's consultancy and the others had them surgically removed. The time interval between initial surgical intervention and EOM presented with significant differences, with a mean time of 6.8 weeks in the case of exposed implants and 17.6weeks in the case of embedded ones. Regarding complications on extraction, one patient presented with the impossibility of removing the implant without surgery and was therefore programmed for surgery.
Regarding final functionality, no significant difference were observed between the two groups, with all patients with embedded implants having excellent results. The 3 patients (4.8%) who presented good results were in the exposed implant group. These 3 patients had a lack of supination <30° at the end of their follow-up. There were no superficial or deep infections (Table 2).
Results with the comparison of the two groups studied.
| Embedded implants | Exposed implants | p | |
|---|---|---|---|
| Mean removal time | 17.6 weeks (8 SD) | 6.8 weeks (1.7 SD) | <0.01 |
| Fracture consolidation | 7.12 weeks | 8.10 weeks | 0.19 |
| Immobilisation time | 7.79 weeks | 8.68 weeks | 0.22 |
| Excellent functionality | 100% | 95.2% | 0.63 |
| Complications | 0% | 2.7% | 0.71 |
| Refractures | 1 | 4 | 0.65 |
SD: standard deviation of the mean.
Finally, 5 patients (6.7%) had refractures, 4 of whom were in the group of exposed implants. Despite this difference, no statistically significant differences were found between both groups.
DiscussionThe refracture risk for a forearm lesion is a major complication which may involve subsequent interventions and a much closer patient management.12
On assessment of the main hypothesis of our study on reducing refractures in paediatric patients with forearm fracture after endomedullary pinning, leaving the pins buried, we did not observe any significant differences to leaving them exposed, and we should therefore reject our main hypothesis.
Regarding our secondary objectives, where functionality and local complications or infection were concerned, finding also coincide that no differences were observed between the two groups studied.
These findings are not conclusive on a matter which has been little studied up until now, but both techniques appear to be viable in the prevention of refractures and present optimum outcomes in final functionality and in complications.
The Lascombes et al.5 group already stated, in their first case series of paediatric fractures treated with endomedullary pinning that the removal of the implants after 4 months led to refractures in 3 of the 50 cases studied. These results, which are very similar to those presented in our study, led to a change in the procedure dynamics and the maintaining of pins between 10 and 12 months after surgery. Later, in a more recent study by the same author9 it was stated that when the pins began to be maintained over 6 months no new refracture cases were observed. These outcomes appear to be related to the quality of the bone cortical and the remodelling of the medullary canal.
In our hospital centre transfer to endomedullary pinning was proposed due to its convenience, lower cutaneous aggression for the patient and prolonged stabilisation offered. However, only 7 patients (9.3%) were immobilised through osteosynthesis for over 6 months, as recommended by Lascombes et al.5 This event may be explained by the difficulty extraction entails with greater delay in time, since the entry point may reossify.
It therefore becomes obvious how important mean implant removal time in this type of patient is. In another study13 the mean refracture time was observed to be 14 weeks, due to the fact that it was still found to be within a bone remodelling period. Nevertheless, the exact period cannot be determined for implant removal to allows us to ensure that the patient does not present with a higher risk of refracture.
The refracture ratio observed in the majority of published series is approximately 5%,14 and does not usually change based on the method of fixation and implant usage, as already suggested by Kelly et al.15 in their article. After analysing a population similar to that used in this study, they were unable to observe any difference between the two treatment groups. This study also analysed secondary variables, such as infections or treatment complications, and similarly to our study data, no differences were observed.
The findings from our study were therefore in keeping with those published in current literature and suggest that burying or leaving implants exposed are the two viable options for the treatment of paediatric forearm fractures.
One factor which could be decisive when choosing one of these techniques is that on leaving the implants exposed, they may be removed at the surgeon's consultancy, without the need to anaesthetise the patient. This would be a more cost-effective process, which has already been assessed by other studies on humeral condylar fractures in paediatric patients.16 However, removal in the consultancy may be a painful process and many surgeons prefer to perform it in the operating theatre regardless of whether the implants are exposed or buried.
Regarding the limits of this study, one of them would be that it is retrospective in nature, which may have meant a loss of data and patients, or that the patients were taken from a single tertiary health centre. However, this enabled uniformity in treatment protocol and the management of these patients and being able to access more standardised data.
To conclude, although in our study we observed no significant differences between the management of paediatric forearm fractures with embedded implants or exposed implants with regard to refractures, complications and final functional outcome and although both options could be appropriate for the management of these fractures, we believe that endomedullary pinning, embedding the pins, could offer fracture stabilisation for longer. This leads to earlier removal of the external cast and fewer risks of infection and skin problems.
Level of evidenceLevel of evidence III.
FinancingThe authors declare they have not received any type of external financing from that of the main institution.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Jordà Gómez P, Antequera Cano JM, Ferràs-Tarrago J, Blasco MA, Mascarell A, Puchol E, et al. Implantes intramedulares enterrados para fracturas de antebrazo pediátricas. ¿Mejora la tasa de refracturas? Rev Esp Cir Ortop Traumatol. 2020;64:35–40.