Physeal bridge resection and insertion of interposition material has had mixed success rates in the literature. Using the arthroscopic approach, some authors have reported good results in their patients. The aim of the study was to evaluate the treatment of post-traumatic central physeal bridges with arthroscopically assisted resection and fat interposition.
Materials and methodsA retrospective study was conducted on 5 patients (6 procedures), who developed a physeal bridge after a traumatic injury. A CT or MRI scan was performed preoperatively in all patients to assess the size of the physeal bridge. Inclusion criteria were patients with documented existing or developing deformities, a physeal bridge <50% of the physeal area, and with at least 2 years of growth remaining. Clinical outcomes were classified according to Marsch and Polzhofer criteria (excellent, good or poor).
ResultsExcellent results were obtained in two patients, good in one, and the other two cases were rated as poor. In patients with a poor outcome, high energy trauma mechanisms were identified in both cases. Moreover, incorrect initial treatment or delayed physeal bridge resection was identified.
ConclusionsThe arthroscopically assisted technique provides best visualization with minimal morbidity. Although our results are not as good as previous studies, it cannot be considered that the technique itself is the cause of the failure, as several risk factors associated to bad prognosis of these injuries were found.
La resección-interposición de los puentes fisarios presenta tasas de éxito variables en la literatura. Respecto al uso de escisión asistida por artroscopio, se han descrito buenos resultados. El objetivo ha sido valorar los resultados del tratamiento de puentes fisarios centrales postraumáticos mediante resección asistida por artroscopio e interposición de grasa.
Material y métodosEstudio retrospectivo sobre 5 pacientes (6 procedimientos), los cuales desarrollaron puentes fisarios tras una fractura fisaria. En todos los pacientes se realizó de forma preoperatoria RMN o TAC para cuantificar el tamaño del puente óseo, y se utilizó la clasificación de Peterson para definir el tipo (periférico, alargado o central). Los criterios de inclusión fueron: puentes fisarios <50% del cartílago fisario total, deformidad progresiva o discrepancia de longitud, y un crecimiento potencial restante de al menos 2 años. Los resultados se evaluaron mediante los criterios de Marsch y Polzhofer en excelentes, buenos o malos.
ResultadosSe obtuvieron resultados excelentes en 2 pacientes, bueno en uno, y malos resultados en los 2 casos restantes. Respecto a los pacientes con mal resultado, hemos identificado la asociación de mecanismos de alta energía en ambos casos, asociándose también un incorrecto tratamiento inicial o resección del puente de forma tardía.
ConclusionesLa asociación de un artroscopio a la resección de un puente fisario permite una excelente visualización con baja morbilidad. Los resultados obtenidos no son tan positivos como los mostrados por otros autores, si bien no podemos atribuir los malos resultados a la técnica propiamente dicha al haber asociación de factores de mal pronóstico.
Although rare, physeal growth arrest secondary to a bone bridge or bar is the most common complication following a physeal fracture. Its frequency ranges between 1% and 10% of all epiphysiolysis procedures.1 The result of complete physeal closure is hypogrowth in length and progressive angulation in the case of partial closure. Early diagnosis helps to prevent the onset of deformity. The most sensitive test is magnetic resonance imaging (MRI), which can detect the appearance of bone bridges within the first 3 months after the trauma, earlier than simple radiography.2 Therefore, this test should be requested in cases of clinical–radiological suspicion of development of a physeal bridge. Furthermore, MRI enables three-dimensional mapping of those physeal bridges which may require surgery. However, the main disadvantage of this technique is the time it requires, which in many cases leads to sedation or general anesthesia. Computed tomography (CT) scans enable quick explorations with low doses of radiation. Specifically, helical CT is highly accurate for preoperative three-dimensional mapping, making it easy to differentiate between physeal cartilage and bone.3
Surgery is indicated in cases of lesions which cause partial growth arrests and meet the following conditions: physeal bars occupying less than 50% of the physis and which have a potential growth of 2 years or 2cm.1,4 Central physeal lesions5 require a metaphyseal access and the performance of a bone window which enables visualization of the surrounding, healthy physis. A difficult access can lead to incomplete resection, and, therefore, Stricker described the use of an arthroscope to help improve the visualization of the healthy peripheral physis.6
The aim of this study was to show the results of the treatment of post-traumatic physeal bridges through resection assisted by an arthroscope. Due to the small sample size, it was difficult to establish the risk factors that could determine the prognosis. However, we have sought to identify those variables that could be associated with an unsatisfactory evolution of the lesion.
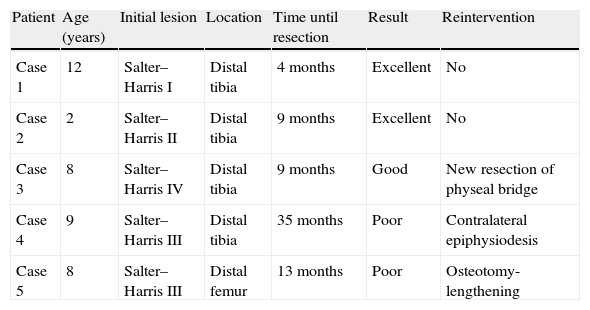
Materials and methodsThe authors intervened a total of 5 patients (6 procedures) through arthroscope-assisted desepiphysiodesis by a metaphyseal portal (Table 1) during the period between 2000 and 2011. In all cases, the physeal bridge was produced by a previous trauma. Cases due to an infectious etiology were discarded. There was 1 case which required reoperation due to incomplete resection. As for gender, 3 patients were boys and 2 were girls. The mean age was 7.8 years (range: 2–12 years).
Characteristics of patients.
| Patient | Age (years) | Initial lesion | Location | Time until resection | Result | Reintervention |
| Case 1 | 12 | Salter–Harris I | Distal tibia | 4 months | Excellent | No |
| Case 2 | 2 | Salter–Harris II | Distal tibia | 9 months | Excellent | No |
| Case 3 | 8 | Salter–Harris IV | Distal tibia | 9 months | Good | New resection of physeal bridge |
| Case 4 | 9 | Salter–Harris III | Distal tibia | 35 months | Poor | Contralateral epiphysiodesis |
| Case 5 | 8 | Salter–Harris III | Distal femur | 13 months | Poor | Osteotomy-lengthening |
The lesions were located in the distal tibia in 4 patients, whilst the remaining were located in the distal femur. According to the Salter–Harris classification there was 1 case of type IV fracture, 2 of type III, 1 of type II and 1 of type I. All patients underwent a diagnostic study using MRI or CT scans to quantify the size of the physeal bridge following the method proposed by Carlson and Wenger.7
The indications for surgical intervention were: physeal bridges <50% of the total physeal cartilage, progressive deformity or length discrepancy, and at least 2 years of subsequent potential growth. The Peterson criteria were followed in order to classify the type of injury according to its size and location: total or partial physeal bridges and peripheral, elongated or central location.8 This method identified 4 central bone bridges and 1 elongated bridge. We discarded patients with peripheral bridges, because the use of an arthroscope is not indicated in such cases.9 All cases had a size under 50% of the total physeal area.
The resection–interposition method employed was an evolution of the classic Langeskiöld technique,10 except for the use of an arthroscope to enable better visualization. Surgery was performed under general anesthesia and pneumatic ischemia of the limb. We produced a window of about 2cm in the metaphyseal cortical using a chisel. With the aid of a high-speed surgical mill, we advanced through the cancellous bone until we reached the physeal bridge area, identified by radiological control. With the mill we proceeded to advance through the bone bar through its central point until the epiphysis was crossed, requiring constant irrigation to allow elimination of the bone remnants in the region. Once the center passage channel was created, we introduced the 30° arthroscope to identify the healthy physeal cartilage. We used the mill to resect the bony tissue constituting the bridge until we reached the healthy physeal tissue, identified by its bluish-white tint. Thus, the entire periphery of the bone bridge was delimited using the arthroscope and mill in combination.9 The liberated physeal space was filled exclusively with fat in order to prevent recurrence.10 We did not employ metal markers routinely to evaluate subsequent growth. In the postoperative period, we immobilized the limb for 1 week, after which active mobility exercises were started. Load on the limb was permitted after the fourth week.
The assessment of subsequent growth was carried out by means of simple radiographs and teleradiographs of the entire limb at 3 months after surgery and then every 6 months. Monitoring was continued until the patient reached skeletal maturity. Only in cases with unsatisfactory or doubtful evolution did we resort to MRI in order to elucidate a possible recurrence. The results were evaluated according to the criteria of Marsch and Polzhofer,9 based on length and angulation discrepancy. The results were considered excellent when the residual deformity was minimal (length discrepancy <2cm and angulation less than 9°) and good when there was a recovery of physeal growth, but with a slight residual deformity which required associated surgical procedures (contralateral epiphysiodesis or corrective osteotomies). The result was considered poor when there was no adequate physeal growth response.
ResultsIn all 5 cases, the mean period elapsed between physeal fracture and surgical resection was 14 months (range: 4–35 months). In 3 cases the lesion involved high energy trauma and in 2 cases the cause was an ankle twist. The mean duration of the surgical procedure was 90min (range: 65–110min). The mean follow-up period was 6.7 years (range: 2–12 years).
We obtained excellent results in 2 patients (Figs. 1 and 2). None of them presented a length discrepancy, although case 1 did present a slight valgus of 6° in the ankle after 2 years of follow-up. One case was classified as a good result because it required a new surgical resection due to persistence of a bone bridge remnant (Figs. 3 and 4). This patient presented a large, elongated, bony bridge, which hindered complete resection. Therefore, a control MRI was performed at 3 months after surgery which showed a residual bridge of 2mm. It was difficult to establish whether it was an incomplete resection or a recurrence. Evolution at 4 years was satisfactory, leaving a slight ankle varus of 5°, without dysmetria in the affected leg. Two patients in the series had poor results; no recovery of physeal growth could be observed. Case 4 presented distal tibial physis growth arrest, resulting in a length discrepancy of 3.5cm. As treatment, we opted for a contralateral epiphysiodesis, resulting in a length discrepancy of 2cm compared to the other leg after 12 years. Regarding patient 5, in addition to the risk factors inherent to the type of physeal injury, there was an associated incorrect osteosynthesis (transphyseal screws) which itself is a potential cause of epiphysiodesis. Patients considered as having poor outcome fractures had suffered high-energy trauma mechanisms and had not received early treatment after physeal injury (13 and 35 months after fracture).
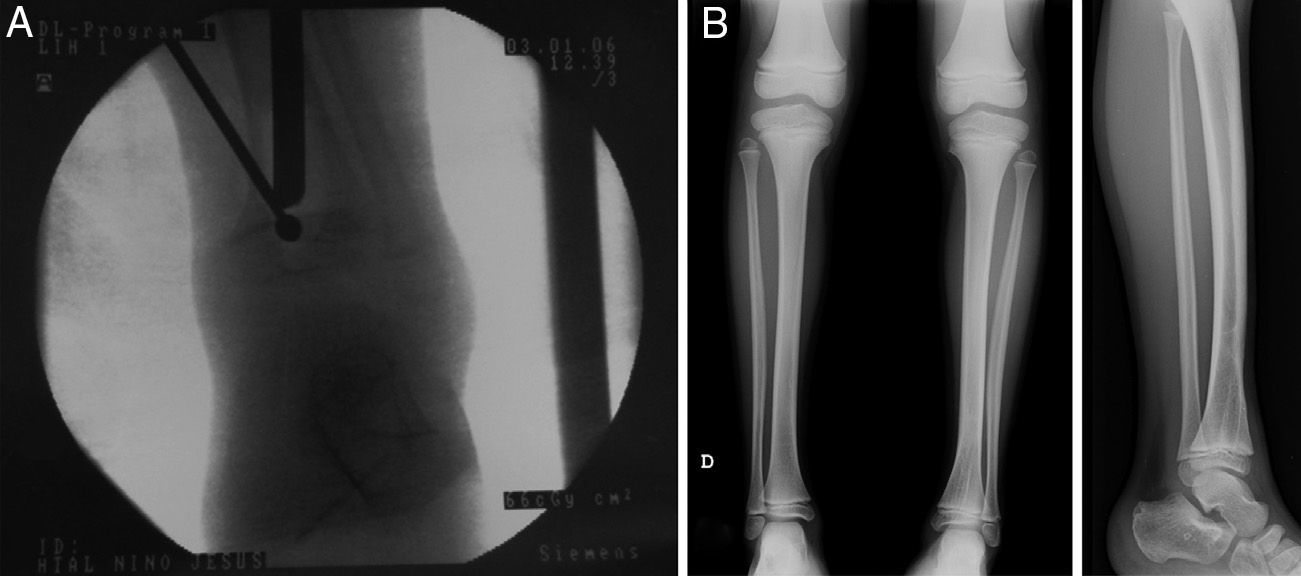
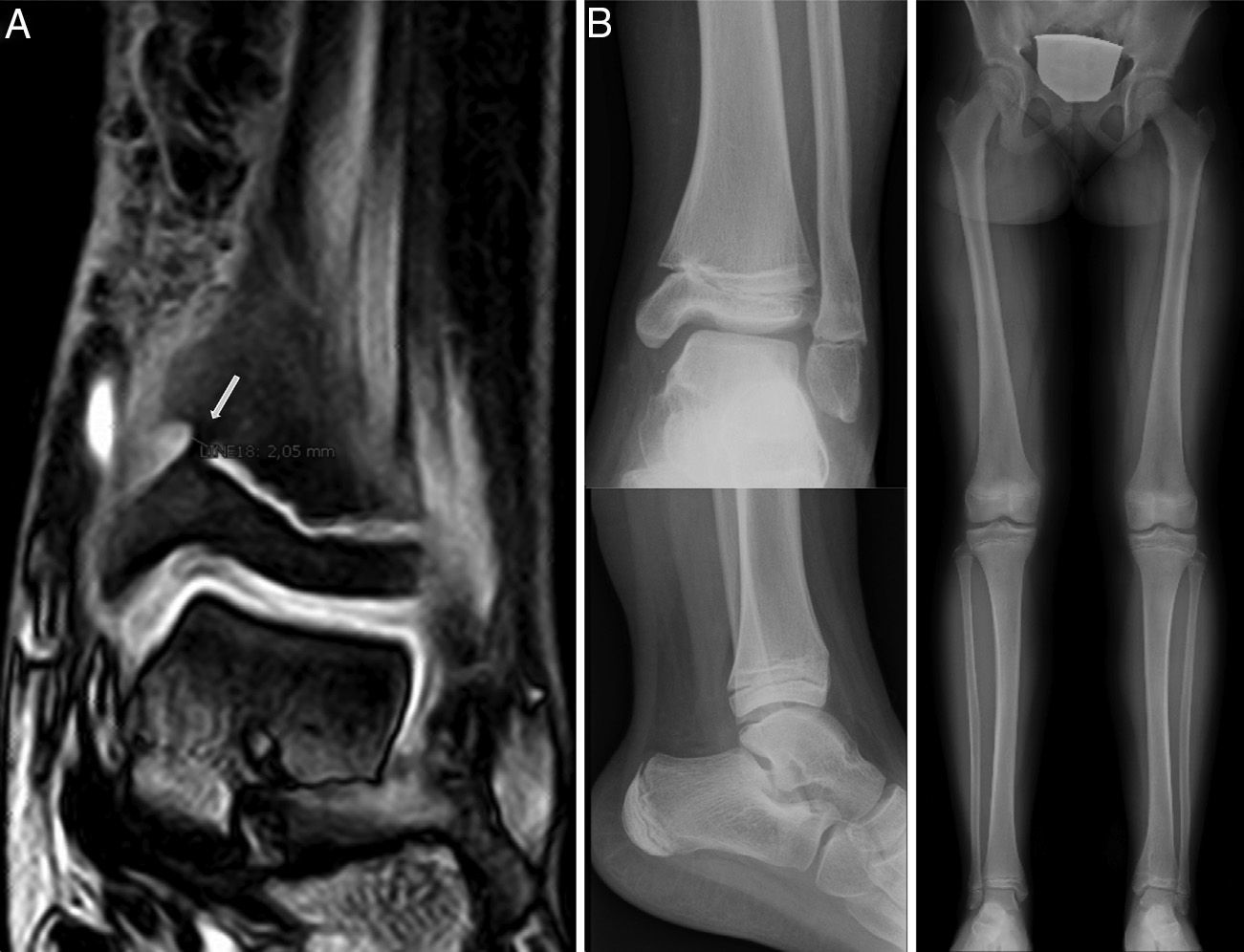
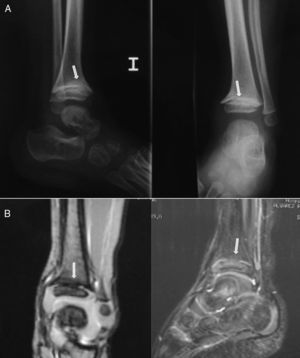
Case 2: a 2-year-old boy who developed a central bone bridge in the distal tibia after Salter–Harris type II epiphysiolysis 6 months earlier. Plain radiographs (A) suggested the presence of a central partial physeal arrest (arrows), which was confirmed by MRI (B). This lesion caused a mild varus angular deformity and length discrepancy of 5mm.
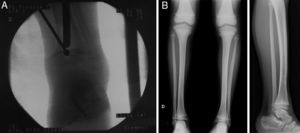
Case 2: the previous injury was treated through arthroscopically assisted resection 9 months after the initial injury. (A) Intraoperative fluoroscopic image showing the simultaneous use of a high-speed mill and arthroscope. (B) Simple radiograph obtained after 5 years follow-up showing a correct alignment without length discrepancy.
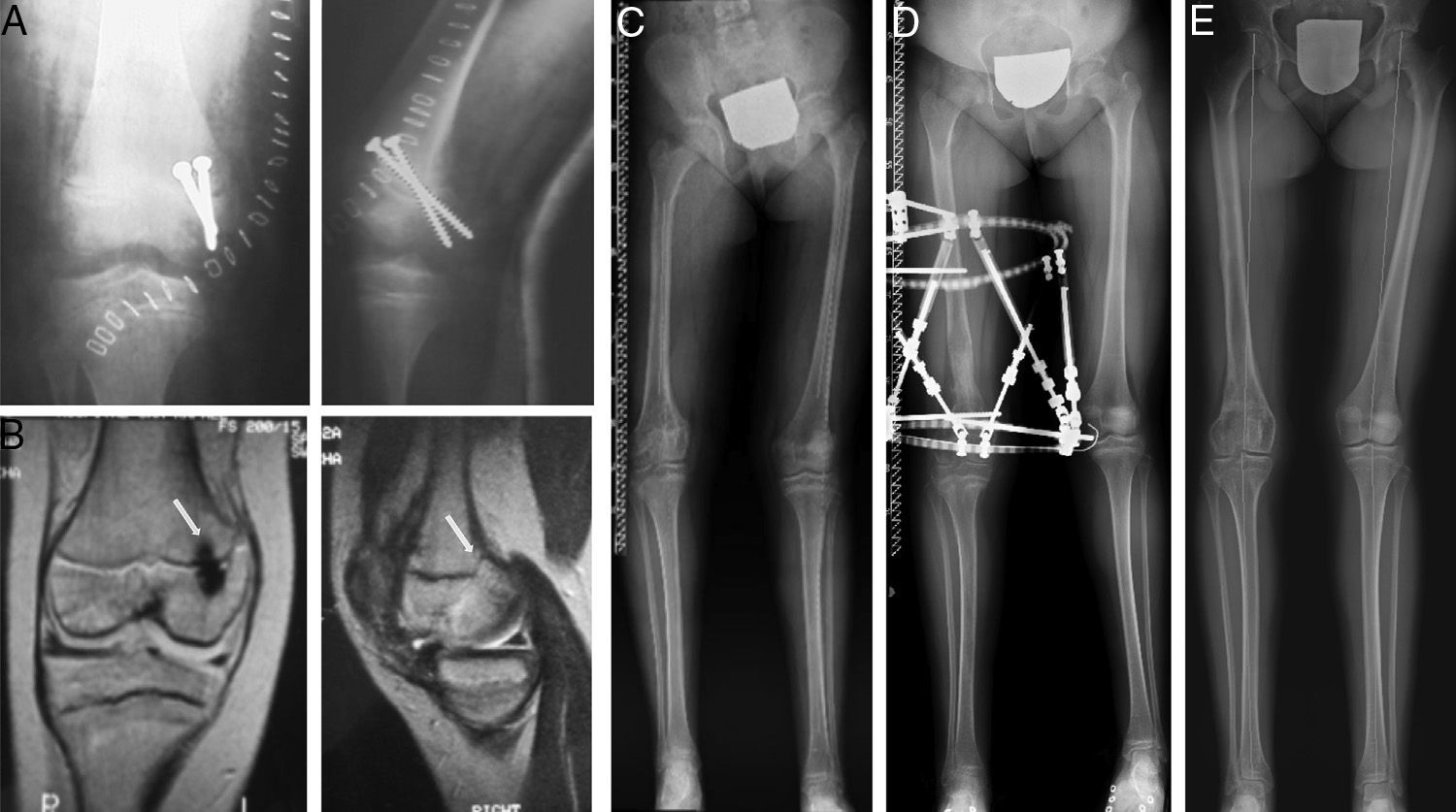
Case 3: an 8-year-old girl who suffered a fall resulting in type IV epiphysiolysis in the distal tibia (A). We performed osteosynthesis using Kirschner wires (B). At 7 months of the lesion, MRI (C) identified an elongated partial bony bridge in the distal medial tibia which caused varus deformity.
Case 3: following surgical resection, the MRI scan (A) showed incomplete resection, leaving an anteromedial bony bridge remnant of 2mm (arrow). Therefore, we performed a new, arthroscopy-assisted intervention. A control radiograph after 4 years showed minimal varus angulation with no length discrepancy (B).
No perioperative complications, such as refractures, neurovascular lesions or infections, took place.
DiscussionPost-traumatic physeal bone bridges appear when there is contact between the epiphysis and metaphysis, a situation that can occur after a displaced fracture. On the other hand, there are ischemic mechanisms present in epiphyseal vascularization that can also assist in the development of this complication.11
There are risk factors that help to predict the formation of a bone bar after a physeal fracture.11,12 As for the location, although traumatic lesions in the growth plate are more common in the upper limbs, bone bridges appear more frequently in the lower limbs, especially in the distal femoral physis and proximal and distal tibial physis.13 This is explained by the higher frequency of high-energy trauma events in these locations, and by physeal morphology itself, which presents ondulations in the knee area.
Barmada et al.14 reported that anatomical reduction decreased the probability of formation of physeal bridges. They observed that, in Salter–Harris type I and II physeal fractures, those cases with a “gap” or residual space greater than 3mm after reduction presented a 60% incidence of bony bridges. In another study of the distal tibia, Leary et al.15 identified the degree of initial displacement and the mechanism of injury as the most predictive factors.
In our study we observed a high incidence of high-energy trauma events (3 patients). An inadequate treatment of the initial fracture by violent manipulations during reduction or an incorrect osteosynthesis may increase the risk of epiphysiodesis. As an example, the use of threaded pins or transfixing physeal screws (Fig. 5) has been associated with this complication.7
Case 5: a 7-year-old girl who suffered type III epiphysiolysis of the distal femur after a traffic accident. We performed an incorrect osteosynthesis using transfixing screws on the physis (A). We subsequently removed the screws and obtained an MRI study (9 months after the initial lesion), which revealed the presence of a posteromedial physeal bridge (B). In spite of the surgical resection of the bridge, the injured physis did not regain growth (C) and led to the development of a 5.6cm shortening compared to the contralateral limb, as well as a varus deformity of 4.5° (anatomical lateral distal femoral angle: 106°) and antecurvatum deformity (anatomical posterior distal femoral angle: 57°). We opted for lengthening-correction osteotomy using a circular external fixator (D). At 6 years after the initial lesion, the control teleradiograph obtained (E) showed a neutral alignment of the limb with a length discrepancy of just 2mm (B).
The time period elapsed from the fracture until bridge resection could be considered as a prognostic factor. Although a precise time limit for the recovery of physeal growth has not been established, some authors have suggested better outcomes with relatively early treatment.12 Comparing the results of our series, we observed that this time span was lower (4.9 and 9 months) for the 3 cases with good results, compared to 13 and 35 months of delay in the 2 cases with poor outcomes.
There is some controversy regarding the ideal method for confirming the diagnosis of physeal bridges. MRI is useful for the initial diagnosis and 3D mapping. In addition, it may also be useful for monitoring the efficacy of surgical treatment.16 In this series we did not perform MRI routinely. We only employed this imaging technique in doubtful cases or in those with inadequate radiographic evolution.
Several studies have found relapses in the formation of bone bridges in cases where interposition material was not used. The most frequent materials for this purpose are fat and polymethylmethacrylate, although studies in animals have shown promising results with the use of cultured chondrocytes.17 Fat has the advantage that it is an inexpensive, autologous tissue, which is easy to obtain, can proliferate in parallel with growth, and does not require subsequent extraction.12
Resection–interposition of physeal bridges presents highly variable success rates. Peterson,1 who reported the largest series, with 98 patients followed until skeletal maturity, observed 84% growth recovery compared to the contralateral limb, although in 87% of cases resection of the bridge was not sufficient and additional surgical procedures were required. Regarding complications, this author found 18% of recurrence, 2% of fractures and 3% of infection. In a study of 22 patients, Loder et al.3 obtained excellent or good results in 73% of cases. These authors recommended performing corrective osteotomy >10° for knee and ankle deformities simultaneously, especially when the bony bridge was >25% of the physis. Furthermore, Bronfen et al.18 reported poor results in 8 of 17 patients treated, despite associating corrective osteotomies in 16 patients. In this study, all the poor results except for 1 were attributed to technical errors or inadequate indications.
There are very few published articles on the use of arthroscopy for the resection of central physeal bars. The longest series using this technique is that by Marsch and Polzhofer,9 which, in a study of 32 patients, showed 87% of good or excellent results. These authors attributed the poor results of 4 patients to infectious etiology in 3 patients, and to the large size of the bony bridge in the other (50%). The present results are not as positive as those shown by these authors, but they should not be attributed to the surgical technique. In addition to the fact that this series was part of the learning curve of the technique, the 2 patients with poor outcomes presented various poor prognostic factors. Both cases had been caused by high-energy trauma, and whilst one of them associated an incorrect initial intervention, the bridge resection of the other was performed belatedly. The obvious limitation of our study is that it was a retrospective study with a small sample size. The low frequency of physeal lesions meant that we were not able to include more cases and that the conclusions reached could not be more significant. Nevertheless, we consider the technique of arthroscope-guided resection and interposition of fat as a potentially useful intervention for the treatment of central bony bridges, since it enables recovery of the growth potential of the physis. The arthroscopic approach enables an excellent visualization of the limits of physeal arrest, thus decreasing morbidity on the healthy growth plate. Although it is a technically demanding procedure which requires familiarity with the use of arthroscopic techniques, it can avoid other, more aggressive surgical interventions.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
FinancingThere have been no sources of financing for the development of this study.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Moreta J, Abril JC, Miranda C. Tratamiento de los puentes fisarios centrales postraumáticos mediante resección-interposición asistida por artroscopio. Rev Esp Cir Ortop Traumatol. 2013;57:333–339.