Anatomical risk factors predisposing to ACL (anterior cruciate ligament) and/or avulsion fractures of tibial spines (AFET) have been reported in paediatric patients with controversial results. Our aim is to compare morphometric parameters in magnetic resonance imaging (MRI) of patients with immature skeleton presenting AFET or ACL rupture versus healthy controls.
MethodsObservational study of a transverse cohort where all those patients with immature skeleton presenting ACL rupture or AFET were collected consecutively. A control group of patients with open physis and MRI reported without lesions was added. A trained observer measured in each MRI with previously standardized technique: (A) the width of the intercondylar femoral notch, (B) the opening angle of the intercondylar femoral notch.
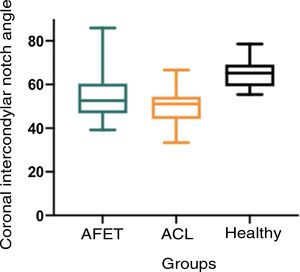
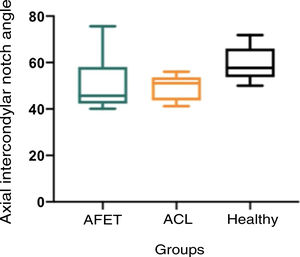
ResultsThe sample was composed of 11 patients with ACL rupture, 11 patients with TEA and 11 normal controls. The opening angle of the intercondylar femoral notch, measured in axial and coronal sections, was significantly lower in those patients with ACL rupture versus healthy controls (p=.0256 and p=.0097). The rest of the variables studied did not present significant differences between groups.
ConclusionIn patients with an immature skeleton, a narrower femoral intercondylar notch is associated with ACL rupture, while those with an ETF do not present a distinctive bone anatomy versus healthy controls. These findings suggest that bone morphometric parameters are associated with a lesional or other pattern in open-knee.
Se han reportado factores de riesgo anatómicos que predisponen a rotura de LCA (ligamento cruzado anterior) y/o fracturas avulsivas de espinas tibiales (FAET) en pacientes pediátricos con resultados controversiales. Nuestro objetivo es comparar parámetros morfométricos en resonancia magnética (RM) de pacientes con esqueleto inmaduro que presenten FAET o rotura de LCA versus controles sanos.
MétodosEstudio observacional de una cohorte transversal donde se recolectaron de forma consecutiva todos aquellos pacientes con esqueleto inmaduro que se presentaran una rotura de LCA o una FAET. Se agregó un grupo control de pacientes con fisis abierta y RM informadas sin lesiones. Un observador entrenado midió en cada una de las RM con técnica previamente estandarizada: (A) el ancho de la escotadura intercondílea femoral, (B) el ángulo de apertura de la escotadura intercondílea femoral.
ResultadosLa muestra se compuso de 11 pacientes con rotura de LCA, 11 pacientes con AET y 11 controles normales. El ángulo de apertura de la escotadura intercondílea femoral, medido en cortes axiales y coronales, fue significativamente menor en aquellos pacientes con rotura LCA versus controles sanos (p=0,0256 y p=0.0097). El resto de las variables estudiadas no presentó diferencias significativas entre grupos.
ConclusiónEn pacientes con esqueleto inmaduro una escotadura intercondílea femoral más estrecho se asocia a rotura de LCA, mientras que aquellos con una FAET no presentan una anatomía ósea distintiva versus controles sanos. Estos hallazgos sugieren que parámetros morfométricos óseos se asocian a un patrón lesional u otro en rodillas con fisis abierta.
Anterior cruciate ligament (ACL) injuries in skeletally immature patients may occur as midsubstance ligament ruptures or as tibial spine avulsion fracture (AFET).1–4 Over the last 20 years, an increasing incidence of these injuries has been reported in children, which is attributed to increased participation in sports and a higher level of competition among this population.5,6
It is estimated that at least 60% of ACL injuries in skeletally immature patients follow an indirect (non-contact) mechanism, highlighting the importance of identifying risk factors to target prevention strategies.7 This is particularly relevant in the paediatric population, where an ACL injury is devastating, and exposes patients to surgery, prolonged rehabilitation, and increased risk of disability with potential contralateral injury. ACL rupture prevention programmes have been shown to reduce injury rates and are cost-effective in at-risk populations.8 Bone morphology of the knee has been extensively studied in the adult population, identifying predisposing factors for ACL rupture.9 However, few studies have reported the correlation between anatomical variables and different patterns of ACL injury in children.10 There has been particular interest in the shape of the intercondylar notch, with controversial results in the paediatric population.11,12 The aim of our study was to determine whether in paediatric cohorts of knees with ACL rupture, versus AFET, versus healthy controls matched for sex and age, there are distinctive morphological parameters of the femoral intercondylar notch that predispose to a particular injury pattern. The hypothesis of the present study was that there are differences in the shape of the femoral intercondylar notch in skeletally immature patients with an AFET versus those with a midsubstance ACL rupture.
Materials and methodWe conducted an observational study of a cross-sectional cohort, which was approved by our institution’s scientific ethics committee.
To select the study group, we reviewed radiological images after online imaging and magnetic resonance imaging (MRI) of the last 11 patients with a diagnosis of tibial spine fracture (AFET group) operated by our institution’s children's knee surgery team between 2017 and 2019. Inclusion criteria were patients with open physis and an acute AFET indicated for surgery. Patients over the age of 18 years, with previous knee surgeries or injuries, or who did not have an MRI study were excluded.
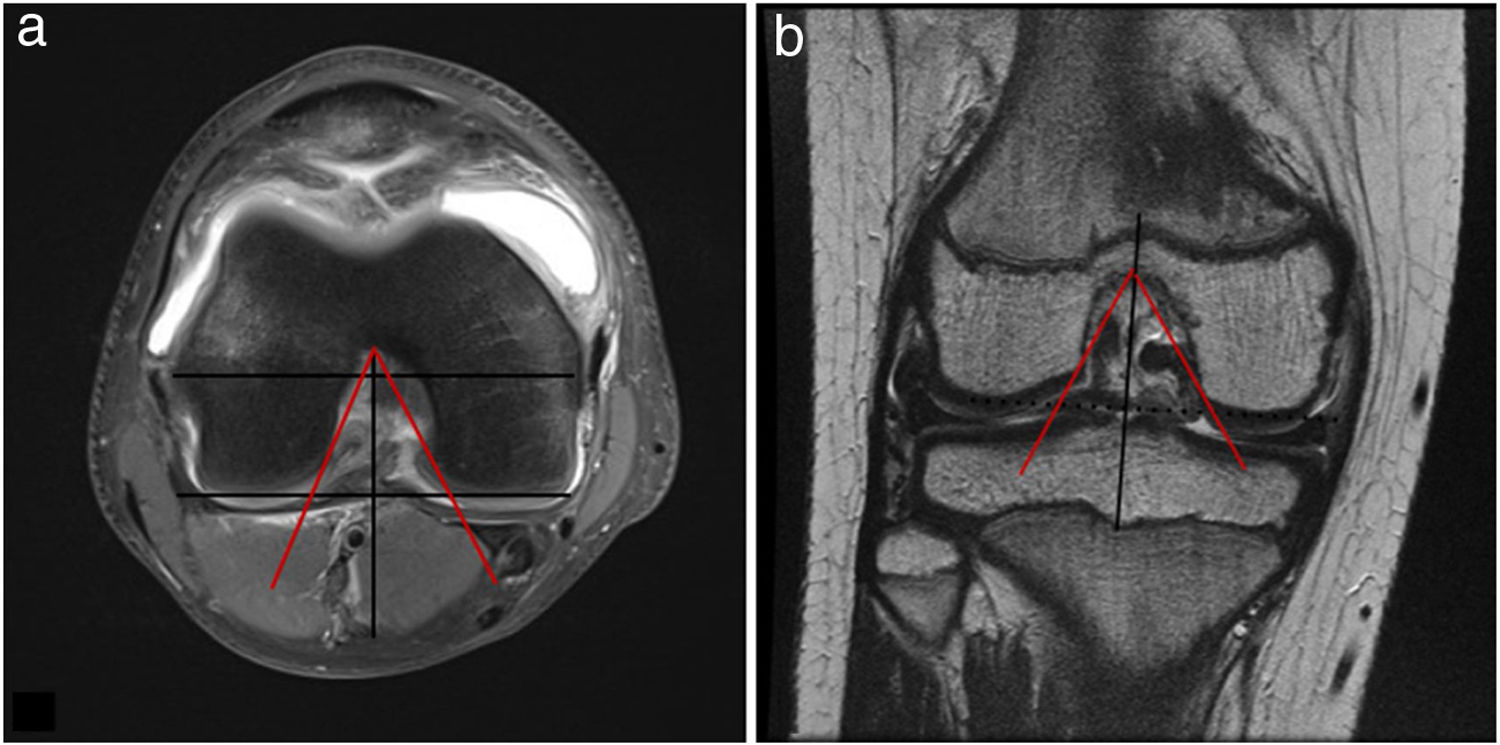
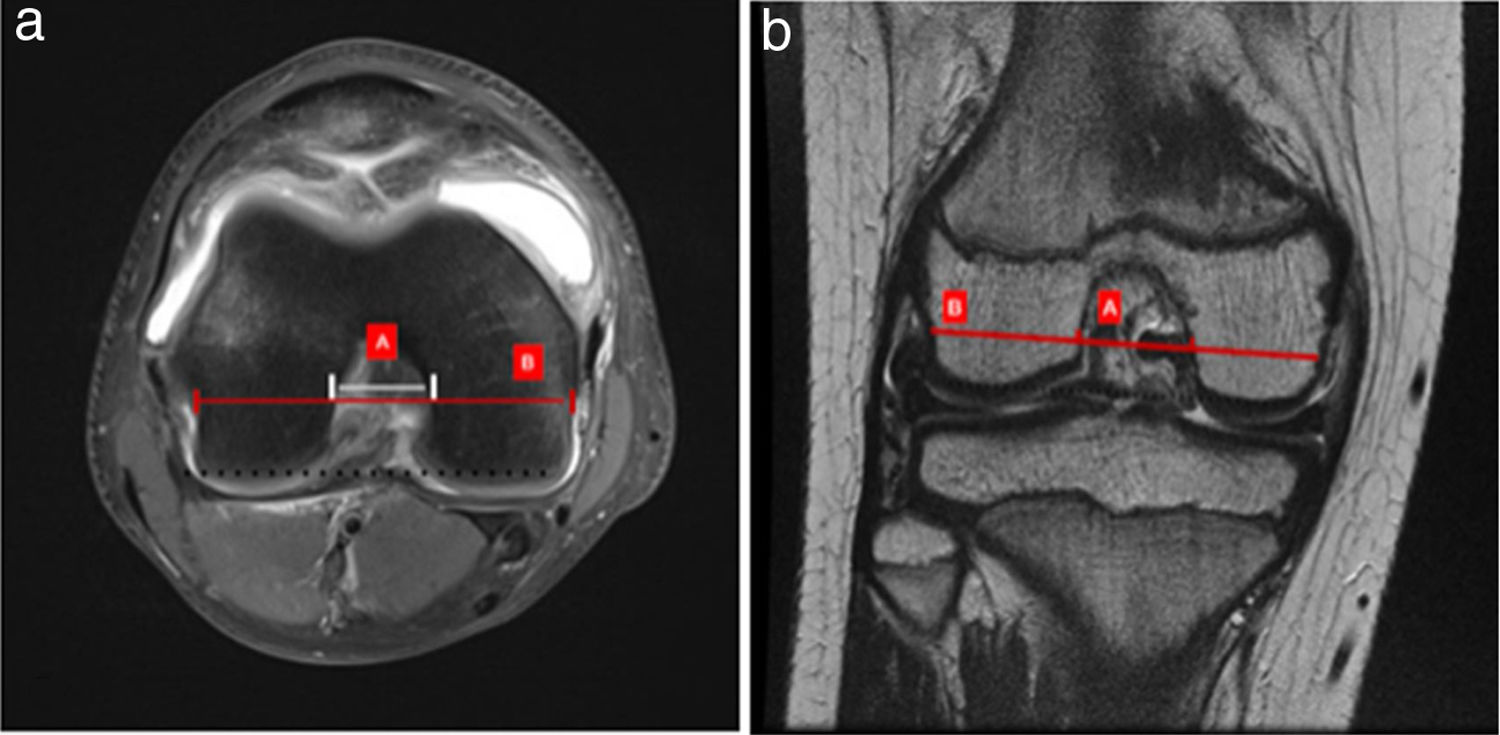
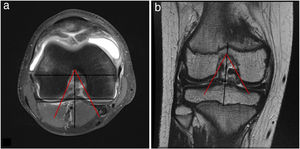
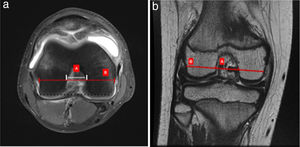
Measurements of morphometric parameters were performed on MRI of knees with open physes, according to previously reported techniques.13 These included coronal intercondylar notch angle, axial intercondylar notch angle (Fig. 1), coronal intercondylar notch width index (CINWI) and axial intercondylar notch index (AINWI) (Fig. 2) using the method described by Stein et al.14 The PD fat sat sequence was used for axial section measurements and T2 sequences for coronal sections. For the measurement of the intercondylar notch angles and the intercondylar notch index, the section showing the popliteal groove at its greatest depth was chosen. All measurements were performed by the same orthopaedic surgeon on three different occasions, obtaining the mean and standard deviation of each measurement.
(a) Measurement of the axial intercondylar notch. In fat saturation sequence on axial section, marking the deepest area of the popliteal recess (upper black line), a line is drawn perpendicular to the posterior transcondylar edge (lower black line), which will be the vertex of the angle of the intercondylar notch (red lines). (b) On coronal section, marking the deepest popliteal recess in T2 sequence, a line is drawn perpendicular to the inferior borders of the lateral and medial condyle (black line) marking the deepest point of the intercondylar notch from where the apex of the angle of the intercondylar notch begins (red lines).
(a) Axial intercondylar notch width index. On axial section where the popliteal recess is observed in greater depth, in fat saturation sequence, a line is drawn marking the edge of the medial and lateral femoral condyles (dotted black line) and a line parallel to this line that goes from the edge of the popliteal recess to the opposite femoral edge (B), and at this height the width of the intercondylar notch is measured (white line), obtaining values for calculation of B/A index. (b) Coronal intercondylar notch width index. On coronal section, where the popliteal recess is observed in greater depth in T2 sequence, the red line of femoral diameter (B) is drawn parallel to the edges of the femoral condyles, and at that level the width of the intercondylar notch is measured (red dots A).
For the control groups, 2 cohorts of consecutive patients were identified assessed by our institution’s children's knee team between 2017 and 2019, for whom MRI had been requested as part of their study. The first control group consisted of patients with a complete anterior cruciate ligament injury (ACL control) and another group of patients whose MRI reported no pathological findings (Healthy control). The same measurements as previously described for the AFET group were performed in both control groups.
Statistical analysisSTATA version 15 (Texas, USA) was used for the statistical analysis. The Fisher's exact and chi-square tests were used to compare the groups in terms of age and gender. An analysis of variance test (ANOVA) with Bonferroni correction was used to compare the results of the MRI morphometric parameters. A p<.005 was considered statistically significant.
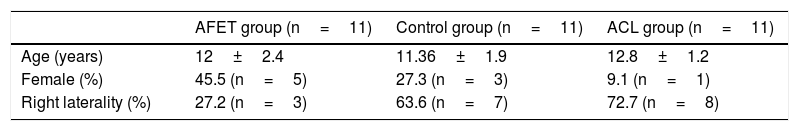
ResultsThe sample comprised 11 patients in the AFET group (6 male, 5 female) with a mean age of 12 years (range 7–16 years). The ACL group comprised 11 patients (10 males, 1 female) with a mean age of 12.8 years (range 11–15). The Healthy control group comprised 11 patients (8 males, 3 females) with a mean age of 11.4 years (range 9–14 years). The groups were comparable in age and gender according to statistical analysis by chi-square and Fisher's test, respectively. Demographic data for the groups are shown in Table 1.
Demographics of the groups.
| AFET group (n=11) | Control group (n=11) | ACL group (n=11) | |
|---|---|---|---|
| Age (years) | 12±2.4 | 11.36±1.9 | 12.8±1.2 |
| Female (%) | 45.5 (n=5) | 27.3 (n=3) | 9.1 (n=1) |
| Right laterality (%) | 27.2 (n=3) | 63.6 (n=7) | 72.7 (n=8) |
ACL: anterior cruciate ligament; AFET: avulsion fracture of tibial spines.
Age corresponds to mean±SD.
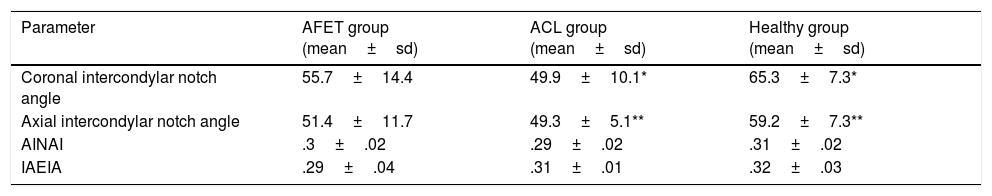
The results obtained from the measurement and comparison of the MRI morphometric parameters are shown in Table 2.
Morphometric parameters.
| Parameter | AFET group (mean±sd) | ACL group (mean±sd) | Healthy group (mean±sd) |
|---|---|---|---|
| Coronal intercondylar notch angle | 55.7±14.4 | 49.9±10.1* | 65.3±7.3* |
| Axial intercondylar notch angle | 51.4±11.7 | 49.3±5.1** | 59.2±7.3** |
| AINAI | .3±.02 | .29±.02 | .31±.02 |
| IAEIA | .29±.04 | .31±.01 | .32±.03 |
AINAI: Axial intercondylar notch angle index; CINAI: Coronal intercondylar notch angle index.
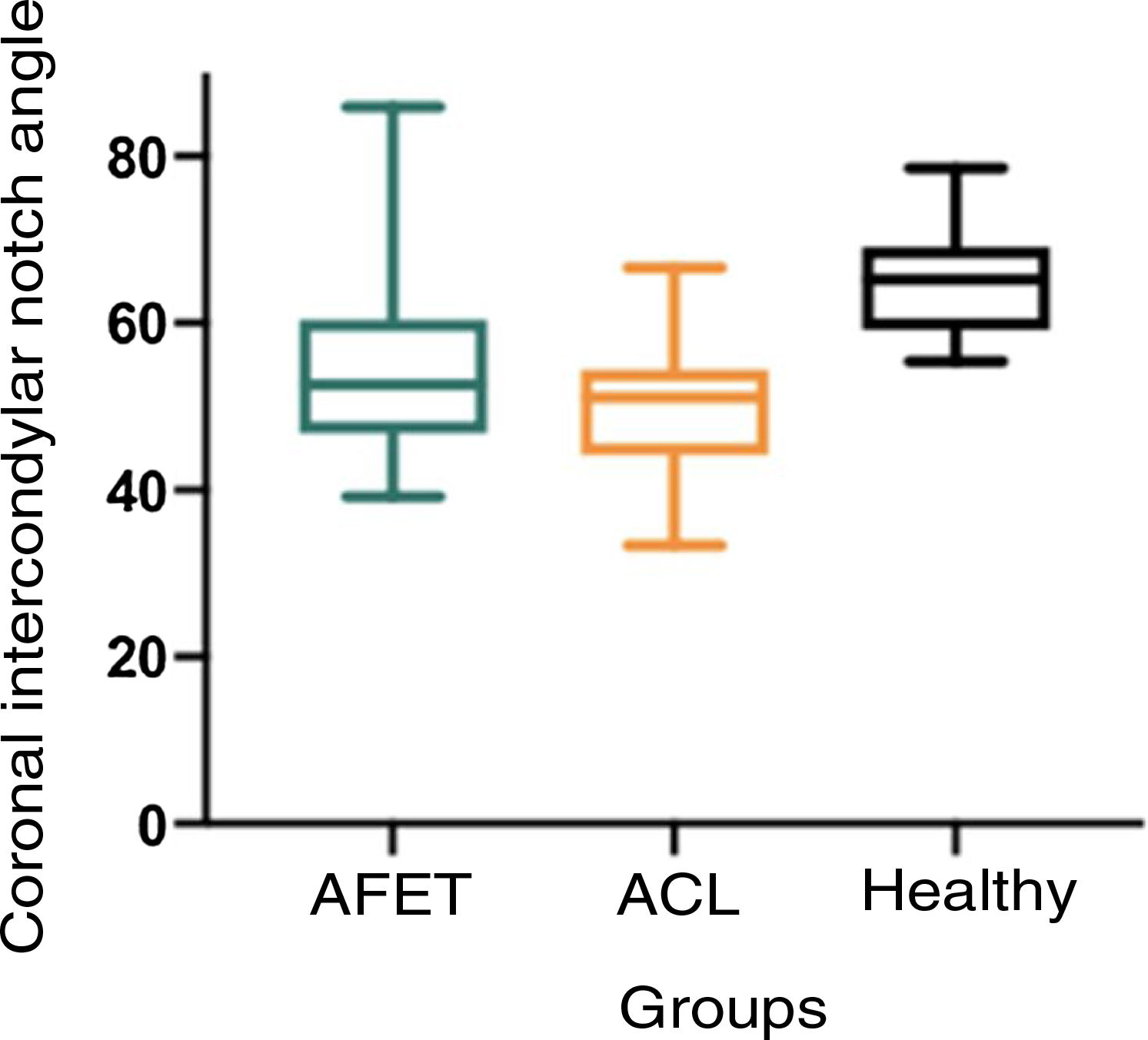
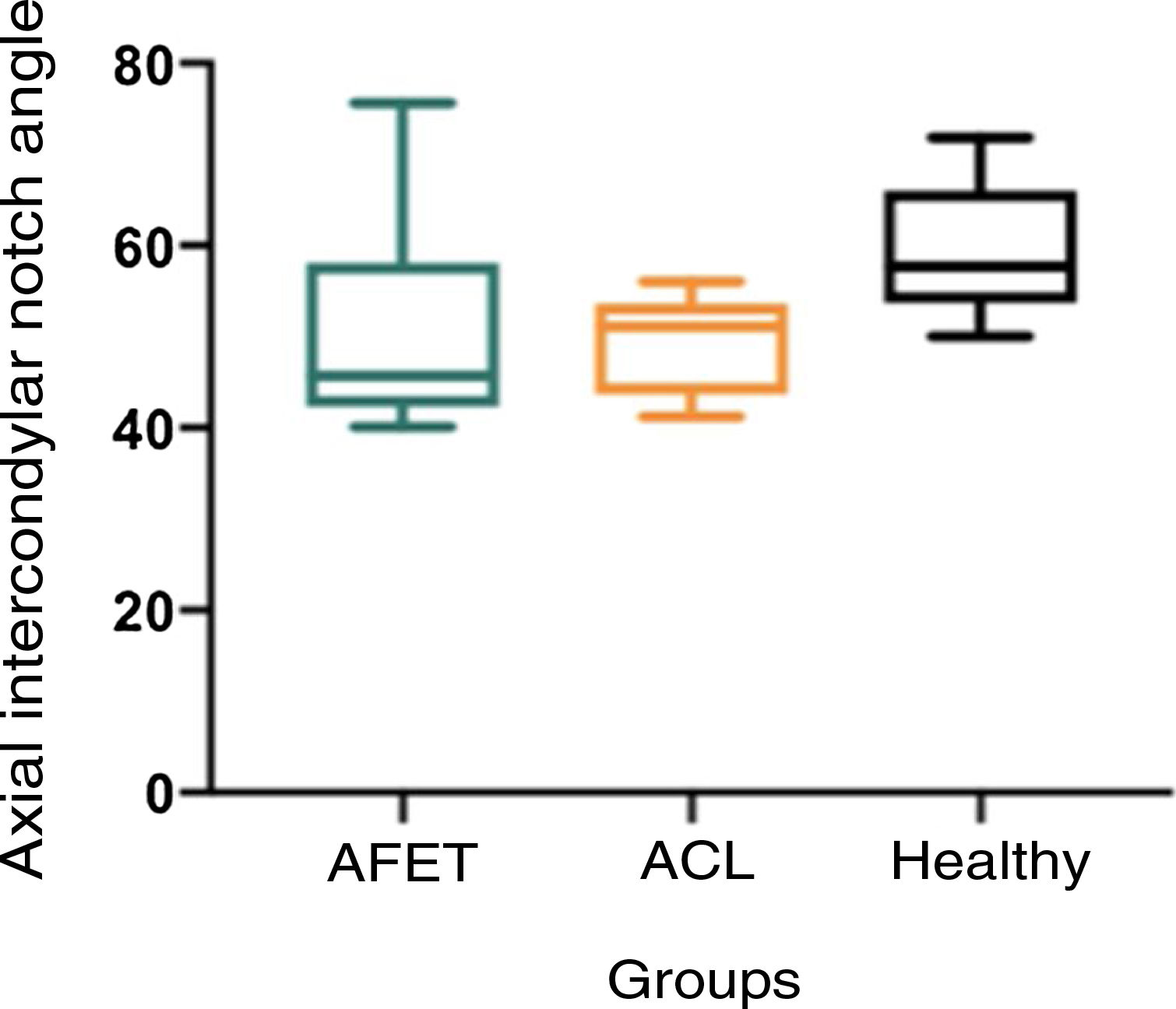
On analysis of the coronal intercondylar notch angle, we observed that the ACL control group had a lower mean angle (49.9±10.1) than the Healthy control group (65.3±7.3), with a statistically significant difference between the groups (p=.0097) (Fig. 3). Regarding axial intercondylar notch angle, the ACL group was lower than the Healthy control group, with a mean of 49.3±5.1 versus 51.2±7.3, and this difference was statistically significant (p=.0256) (Fig. 4).
No statistically significant difference was found between the groups in relation to coronal intercondylar notch width index or axial intercondylar notch width index.
DiscussionThe main finding of our study was that skeletally immature patients with a midsubstance ACL rupture have a distinctive bone morphology in their knee when compared to those with an AFET or healthy controls. Patients with ACL rupture had a significantly narrower intercondylar groove versus healthy controls matched for sex and age. On the other hand, patients with open physes with an AFET had no morphological differences versus healthy controls.
In the adult population, several anatomical factors have been described that would be associated with an increased risk of ACL injury. Palmer et al. were the first to describe the association between intercondylar notch stenosis and ACL injury.15–19 Multiple anatomical factors, such as increased posterior tibial slope of the tibial plateau, a flatter tibial plateau,20–22 decreased width of the femoral condyle,23 increased volume of the intercondylar notch24 and decreased height and volume of the tibial spine have been associated with ACL injury in the adult population.25,26 In skeletally immature patients, there is less literature on factors that increase the risk of ACL injury. Domzalski et al.5 established a correlation with a narrower intercondylar notch width index in paediatric patients, and Souryal et al. also evaluated 2500 radiographs, showing a correlation between a narrower intercondylar notch width index and ACL ruptures in children.16 In line with the findings of our study, Kocher et al.12 reported that a narrower notch width index was associated with a higher risk of midsubstance ACL injury than AFET. However, most of these studies measured these parameters on radiographs, which translates into high variability in technique and results as described by Herzog et al.27 More recent studies have used MRI measurements, showing an increased risk of ACL injury in association with anatomical factors such as increased lateral tibial slope13 and a narrower notch width index.9 Shaw et al.9 demonstrated that patients with wider tibial eminences had a higher risk for AFET than for midsubstance ACL injury.
Based on the literature and the findings of our study, we can infer that with the same mechanism of injury, patients with anatomical risk factors (narrower notch angle) would be more susceptible to a midsubstance ACL rupture, while those with more "normal" anatomy would be more prone to AFET, irrespective of age and gender. This could be explained by the biomechanical theories described by Alentorn-Geli et al. where they suggest that the shape of the intercondylar notch would be more relevant than its volume as a risk factor for ACL rupture.28 In line with our findings, they propose that a narrow intercondylar notch, which does not necessarily correlate with a narrower or smaller volume notch index, would predispose to ACL rupture due to impingement of the ligament against the medial femoral condyle under anterior translation and forced valgus forces. The main clinical relevance of this study is to further the identification of anatomical risk factors so that we can target prevention strategies. Optimising the prevention of these injuries is of utmost importance, especially in the paediatric population. ACL rupture prevention programmes, designed as exercise sequences, have been shown to significantly reduce the rate of ruptures, and even more so if applied in at-risk populations.8 Early ACL rupture has a worse prognosis than AFET, and it is therefore crucial to reduce the incidence of these injuries.
In terms of the clinical usefulness of these findings, notch measurements can be performed in a simple and accessible way by plain knee X-ray, but it depends on the correct positioning of the patient and there is variability in technique, magnification and projection.29 It has been shown that this variability decreases when measurements are performed on MRI.30 Likewise, Herzog et al. demonstrated that measurement of the notch width index on MRI was more accurate than on X-ray, given the late ossification of the proximal tibial epiphysis in children, MRI measurements represent the joint surface more accurately. Taking this into consideration, radiography may be a useful screening tool for anatomical risk factors that is more accessible and lower cost. However, MRI, which has recently become more widely used in child athletes, will be more accurate in identifying these anthropometric parameters. As described for patellofemoral instability, we must make headway in identifying risk factors that will help us recognise vulnerable subgroups.
The limitations of our study include the retrospective nature of our research, with the inherent biases of such a study. A larger sample size would increase the statistical power of our study; however, AFETs are rare injuries, and this series is comparable in number to previously published studies. Likewise, despite the limited sample size, our results were significant. Morphometric measurements were performed by a single, unblinded observer. However, these measurement tools have been validated previously, with interobserver agreement reported to be almost perfect (kappa .84).12
ConclusionIn skeletally immature patients a narrower intercondylar notch was associated with an increased risk of midsubstance ACL rupture versus healthy controls in the paediatric population of our study. In contrast, patients who sustained an avulsion tibial spine fracture did not have a distinct femoral intercondylar notch bone anatomy compared to healthy controls. The findings of our study suggest that femoral bone morphometric parameters are associated with an injury or other pattern in knees with open physes.
Level of evidenceLevel of evidence IV.
Please cite this article as: L. Silva, N. Bernal, M. Tuca et al., Una escotadura intercondílea estrecha favorece la rotura del ligamento cruzado anterior (LCA) en pacientes con esqueleto inmaduro, Revista Española de Cirugía Ortopédica y Traumatología. Rev Esp Cir Ortop Traumatol. 2021;61:201–206.