Iatrogenic tracheal rupture (ITR) is a serious complication secondary to procedures such as emergent orotracheal intubation or tracheostomy, among others. The management of ITR depends on the size, extension and location of the injury, along with the patient's respiratory status and comorbidities. The priority of treatment is to keep the airway permeable to ensure adequate ventilation. We present the case of a tracheal rupture after performing a percutaneous tracheostomy, in a patient diagnosed with severe acute respiratory distress syndrome secondary to bilateral interstitial pneumonia due to SARS-Cov-2. The issues are discussed, such as the management (conservative vs. surgical) depending on the features of the injury and the patient, in the extraordinary context that the COVID-19 pandemic has entailed.
La rotura traqueal iatrogénica (RTI) es una complicación grave secundaria a procedimientos como intubación orotraqueal emergente o realización de traqueostomía entre otros. El manejo de la RTI depende del tamaño, extensión y localización de la lesión, junto con el estado respiratorio y comorbilidades del paciente. La prioridad del tratamiento es mantener permeable la vía aérea para asegurar una adecuada ventilación. Presentamos el caso de una rotura traqueal tras la realización de traqueostomía percutánea, en un paciente diagnosticado de síndrome de distrés respiratorio agudo grave secundario a neumonía intersticial bilateral por SARS-CoV-2, e intentamos arrojar luz sobre el manejo (conservador vs. quirúrgico) en función de las características de la lesión y del paciente, en el contexto tan particular que ha supuesto la pandemia COVID-19.
Iatrogenic tracheal rupture (ITR) is a serious complication secondary to procedures such as orotracheal intubation (OTI), tracheostomy (percutaneous or surgical), neck and mediastinum surgery, fibreoptic bronchoscopy, and others. The estimated incidence of ITR varies from 0.05% to 0.37% in single lumen OTI1, 0.5% to 1% in dual lumen OTI2 and 1% in percutaneous tracheostomy3. The management of ITR depends on the size and extent of the lesion, the location, the patient’s respiratory status and comorbidities. The priority is to keep the airway patent to ensure adequate ventilation.
We report a case of ITR after percutaneous tracheostomy in a patient diagnosed with severe acute respiratory distress secondary to SARS-CoV-2-induced bilateral interstitial pneumonia in which conservative management led to closure of the fistula and tracheostomy decannulation with no complications.
Case reportA 70-year-old man was diagnosed with SARS-CoV-2-induced bilateral interstitial pneumonia and admitted to the Resuscitation and Critical Care Unit due to severe acute respiratory distress syndrome (ARDS). His clinical history was significant for smoking, mild hypertension and dyslipidaemia under dietary treatment. During his stay on the hospital ward he had been treated with antibiotics (azithromycin and ceftriaxone), antivirals (lopinavir/ritonavir) and immunomodulators (methylprednisolone, hydroxychloroquine and tocilizumab).
After transfer to the Resuscitation and Critical Care Unit the patient required urgent endotracheal intubation due to respiratory failure, which was performed without incident, and severe hypoxaemia that lasted for several days and required protective mechanical ventilation, sedation and neuromuscular relaxation with several cycles of prone positioning lasting around 16 h. His respiratory and clinical status (haemodynamic instability, difficulty in sedoanalgesia, and adaptation to mechanical ventilation) did not stabilise until day 25 of admission, when were able to perform percutaneous tracheostomy in order to optimize weaning from mechanical ventilation.
The fibreoptic-guided percutaneous tracheostomy was performed in the operating room, inserting a number 8 Tracoe® cuffed tube between the second and third tracheal rings following, as far as possible, the safety recommendations published in the consensus document on tracheostomy in patients with COVID-194. No complications were observed during percutaneous dilation or fibreoptic bronchoscopy performed at the end of the procedure to confirm the distance to the carina.
A few minutes after performing the tracheostomy, a large subcutaneous emphysema was observed gradually spreading to both pectorals, upper limbs, neck and face, together with a leak of around 20% of the prescribed minute volume. At that time, peripheral oxygen saturation was between 95%–98% with an FiO2 of 0.8 and heart rate of 90 bpm. The patient required vasoactive support with low-dose norepinephrine to achieve a mean arterial pressure between 65−70 mmHg.
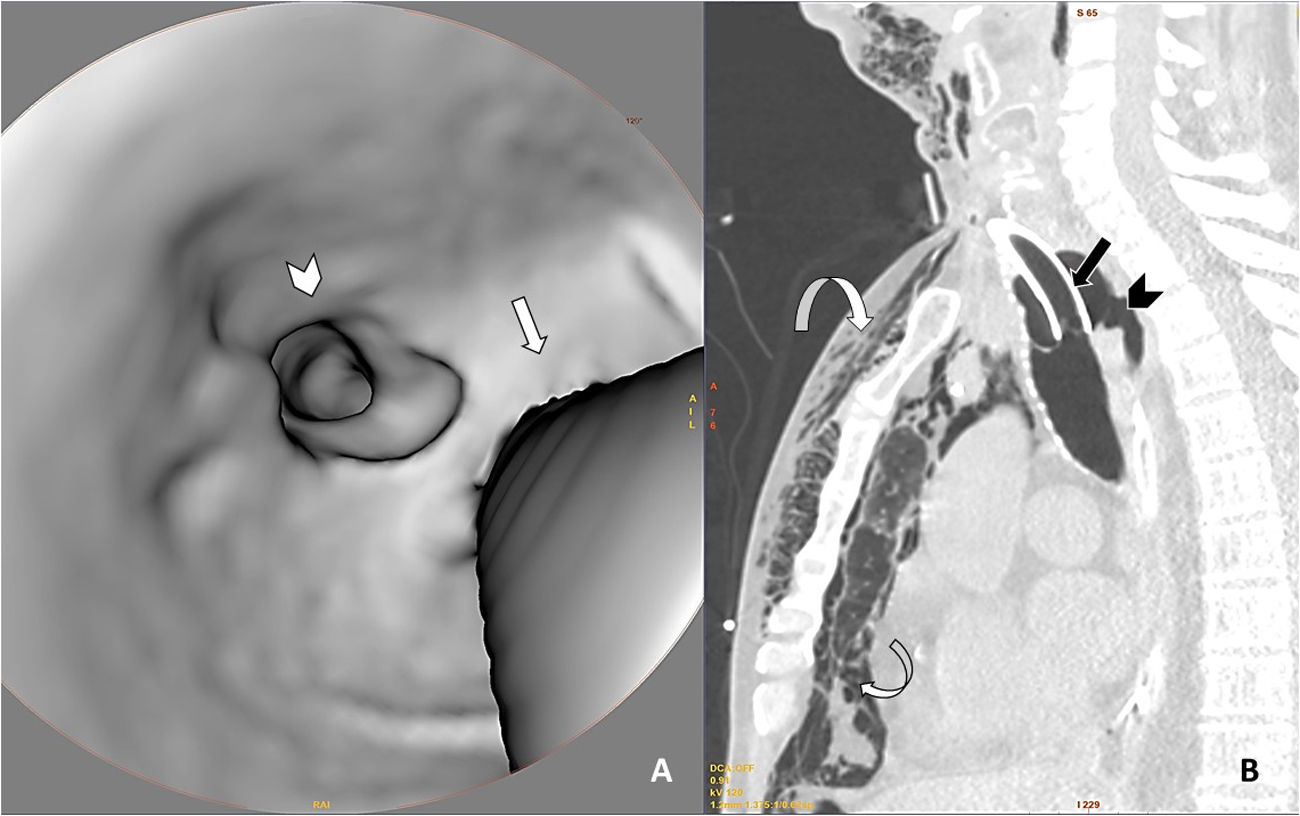
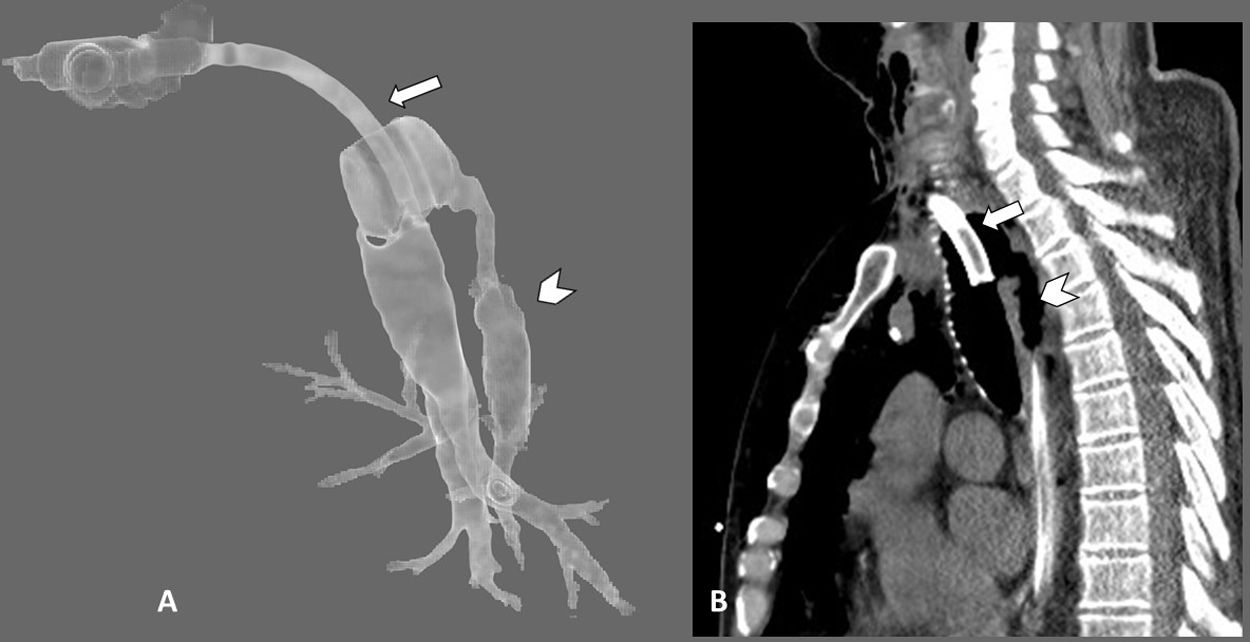
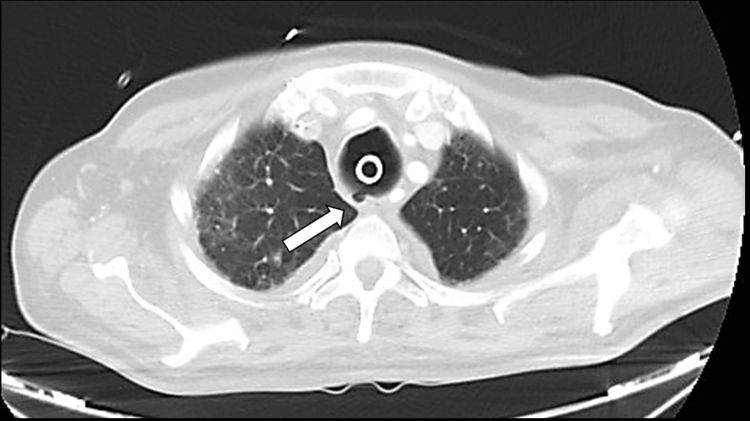
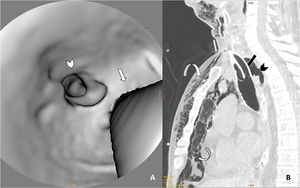
Given the suspicion of ITR that had not been noted during the fibreoptic bronchoscopy performed at the end of the tracheostomy, we decided to perform a cervicothoracic CT. This showed a sabre-sheath trachea (AP axis greater than the transverse, indicative of tracheomalacia) with a perforation measuring 6 mm in length in the craniocaudal axis of the posterior tracheal wall that communicated directly with the pneumomediastinum chamber, accompanied by generalised subcutaneous emphysema that extended through all the visualized planes from the upper abdomen to the lower region of the skull. Moderate right haemothorax and residual left anterior pneumothorax were also observed, as well as multiple foci of pulmonary consolidation and diffuse ground glass opacities, predominantly peripheral, indicative of ARDS due to SARS-CoV-2 pneumonia (Figs. 1, 2 and 3).
Neck and chest CT scan with 3D axial reconstruction of the trachea (A) and sagittal reconstruction of the upper thorax (lung window) (B) showing a defect in the posterior wall of the trachea (arrowhead in both images) associated with pneumomediastinum and marked subcutaneous emphysema (curved arrows). To help interpret the 3D reconstruction, straight arrows have been added in both images to indicate the posterior edge of the tracheostomy tube.
A: Axial chest CT image using a lung window showing tracheal rupture (black arrow head), pneumomediastinum and marked subcutaneous cellular emphysema (curved arrow). The right hemithorax shows high-density pleural effusion associated with haemothorax (white arrowhead), as well as patchy ground-glass opacities in the lung parenchyma associated with SARS-CoV-2 involvement (white straight arrow). B: 3D reconstruction of subcutaneous emphysema.
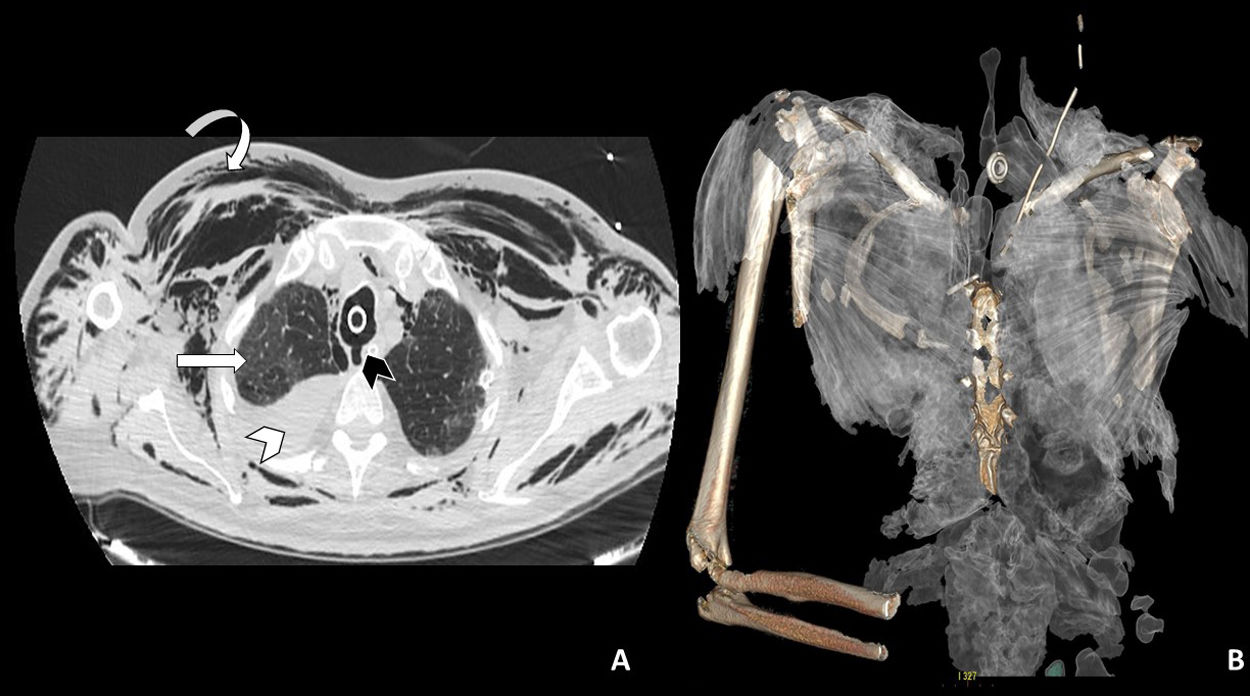
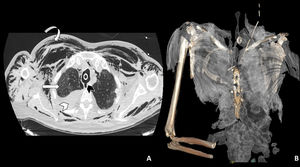
Given the radiological findings, the ENT was contacted and it was decided to perform OTI in the operating room to remove the tracheostomy and perform a new one, this time surgical, distal to the previous one (at the approximate level of T3-T4 vertebrae). A number 9 Tracoe® cuffed tracheal tube with a drain on the lateral cervical surface was inserted without incident. Following this, the antibiotic prophylaxis for mediastinitis was extended and, since the patient had previously required high doses of sedoanalgesia and relaxation, the neuromuscular blockade was maintained for 10 further days to avoid sudden episodes of maladjustment and cough that could increase the tracheal defect. The patient’s respiratory and haemodynamic evolution was satisfactory. During this period, 2 chest tubes were also placed for drainage of both hemopneumothorax. The patient made good progress, so we decided to perform a follow-up CT 12 days after the new tracheostomy, which showed persistence of the defect in the upper third of the posterior tracheal wall and the formation of a pseudodiverticulum, fibrotic changes in the adjacent mediastinal fat, resolution of the pneumomediastinum and absence of subcutaneous emphysema or evidence of collections or air leak at other levels (Fig. 4).
Axial chest CT image (lung window) performed 12 days after the new tracheostomy, in which persistence of the tear is observed in the upper third of the posterior tracheal wall, with the formation of a pseudodiverticulum (arrow) and resolution of pneumomediastinum and subcutaneous emphysema.
We reassessed the patient daily together with the ENT specialist, and it was decided to resume respiratory weaning, withdraw neuromuscular relaxation and progressively reducing sedoanalgesia. Eighteen days after the intervention, and under fibreoptic guidance, the tracheostomy cannula was changed to a number 8 fenestrated cuffed tube. Having observed that the patient breathed spontaneously without incident over the next few days, he was finally decannulated 3 days before leaving unit. The patient was transferred to the ward 55 days after admission to the Resuscitation and Critical Care Unit, eupnoeic, with excellent respiratory mechanics and in good general clinical condition. The ENT specialist followed up his tracheal lesion.
DiscussionITR is a rare complication that can arise after numerous procedures and, therefore, using the existing literature it is hard to establish its true incidence secondary to percutaneous tracheostomy. The estimated incidence of IRT varies, according to the published series, between 0.05% and 1%1–3.
The clinical manifestations described in the literature that should lead to suspicion of ITR are: subcutaneous emphysema predominantly in the chest, neck and face (present in most cases), pneumothorax and pneumomediastinum, usually visible on imaging tests, accompanied or not by respiratory failure. Despite the immediate availability of CT in our hospital, the gold standard for diagnosis continues to be fibreoptic bronchoscopy3.
Different risk factors have been considered, and can be divided into anatomical and mechanical characteristics5. The anatomical characteristics include female sex, age over 50 years, tracheal abnormalities (tracheomalacia, tracheal stenosis, weakness of the pars membranosa), diseases that alter the position of the trachea (mediastinal collections, adenopathies, tumours), chronic use of steroids, COPD, and other lesions or inflammatory processes of the airway tree, such as those caused by infectious agents. The main mechanical risk factors are urgent OTI (the probability increases up to 15% after urgent/emergent procedures in patients with an ASA III-IV physical status6), inadequate tube size, operator inexperience leading to repeated intubation attempts, traumatic OTI with the need for fasteners, overinflation of the cuff, and mobilization of the head and neck during intubation, the latter being common in COVID-19 patients undergoing prone positioning to treat refractory hypoxaemia due to ARDS. The cases with higher mortality are those that are associated with emergency intubation and/or the development of mediastinitis. The impact of the length of the defect is still a unclear5,7.
Our patient presented several of the aforementioned risk factors, since he was 70 years old, his airway epithelium was probably vulnerable due to both SARS-CoV-2 treatment (immunomodulators, corticosteroids and antivirals) and the viral infection itself, his trachea was considerably dilated and weakened after 25 days on mechanical ventilation with high inspiratory and expiratory airway pressures, and he had undergone cyclical prone positioning due to severe ARDS.
Conservative management appears to be indicated for small lesions (<2 cm) with no oesophageal damage, in stable patients with contained subcutaneous emphysema, in patients not requiring mechanical ventilation or in patients that do not present significant leaks if mechanical ventilation is necessary. Surgery is indicated in unstable patients with extensive lesions that affect mediastinal structures8, and several authors agree that surgery is indicated when tracheal damage is observed intraoperatively and can be corrected immediately5. Other less aggressive approaches have also been proposed, including repairing the defect with cervicotomy without the need for thoracotomy. Another less invasive option, although not without complications, is the endoscopic placement of a self-expandable tracheal stent8.
Finally, extracorporeal membrane oxygenation could be a non-surgical treatment option for IRT9, as it would provide ultra-protective ventilation and reduce both airway pressures and air leakage. It could also facilitate oxygenation in patients with ARDS with refractory hypoxaemia, although this has not yet been tested extensively.
In our patient, surgical management of the lesion was initially considered, since he was in poor overall condition, with ARDS that required high airway pressures, and at high risk for mediastinitis. However, there were 2 major obstacles to this: our hospital does not have a thoracic surgery service and the patient could not be transferred to another hospital due to his critical condition and to the fact that by April 2020 all hospitals in the Community of Madrid were overwhelmed. Extracorporeal membrane oxygenation, which would have allowed us to deliver ultra-protective ventilation, reduce airway pressure, and permit the tear to resolve spontaneously, was also unavailable in our hospital.
The strategy chosen in this case is also considered conservative, or minimally invasive as other authors call it6, since it only involved performing a new tracheostomy distal to the previous percutaneous incision, thus avoiding a breathing circuit lesion that would aggravate the ITR. This allowed the tracheal defect to close spontaneously and prevent further leakage, even at the expense of fibrosis of the adjacent mediastinal fat. To complete the strategy and prevent other complications, both hemopneumothoraxes were drained and the aforementioned antibiotic prophylaxis was started.
The even though conservative strategy implemented was our only option, it is in line with recommendations found in the literature5,10 for lesions of this type in patients with a favourable prognosis.
ITR is an uncommon complication, and this makes it difficult to establish recommendations that are applicable to most patients. Due to the uncertainties surrounding the choice of conservative vs surgical treatment of this complication and its high rate of mortality, it is essential to take a multidisciplinary approach and individualise management in accordance with the severity of the injury and the available resources.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Redondo Martínez P, Gijón Herreros N, Delgado García DR, Quílez Caballero E, Porras Muñoz MC, García del Valle y Manzano S. Rotura traqueal iatrogénica en paciente con síndrome de distrés respiratorio agudo por neumonía SARS-CoV-2. Rev Esp Anestesiol Reanim. 2021;68:597–601.