Coronavirus disease 2019 (COVID-19) is a respiratory tract infection caused by a newly emergent coronavirus, that was first recognized in Wuhan, China, in December 2019. Currently, the World Health Organization (WHO) has defined the infection as a global pandemic and there is a health and social emergency for the management of this new infection. While most people with COVID-19 develop only mild or uncomplicated illness, approximately 14% develop severe disease that requires hospitalization and oxygen support, and 5% require admission to an intensive care unit. In severe cases, COVID-19 can be complicated by the acute respiratory distress syndrome (ARDS), sepsis and septic shock, and multiorgan failure. This consensus document has been prepared on evidence-informed guidelines developed by a multidisciplinary panel of health care providers from four Spanish scientific societies (Spanish Society of Intensive Care Medicine [SEMICYUC], Spanish Society of Pulmonologists [SEPAR], Spanish Society of Emergency [SEMES], Spanish Society of Anesthesiology, Reanimation, and Pain [SEDAR]) with experience in the clinical management of patients with COVID-19 and other viral infections, including SARS, as well as sepsis and ARDS. The document provides clinical recommendations for the noninvasive respiratory support (noninvasive ventilation, high flow oxygen therapy with nasal cannula) in any patient with suspected or confirmed presentation of COVID-19 with acute respiratory failure.
This consensus guidance should serve as a foundation for optimized supportive care to ensure the best possible chance for survival and to allow for reliable comparison of investigational therapeutic interventions as part of randomized controlled trials.
La enfermedad por coronavirus 2019 (COVID-19) es una infección del tracto respiratorio causada por un nuevo coronavirus emergente que se reconoció por primera vez en Wuhan, China, en diciembre de 2019. Actualmente la Organización Mundial de la Salud (OMS) ha definido la infección como pandemia y existe una situación de emergencia sanitaria y social para el manejo de esta nueva infección. Mientras que la mayoría de las personas con COVID-19 desarrollan solo una enfermedad leve o no complicada, aproximadamente el 14% desarrollan una enfermedad grave que requiere hospitalización y oxígeno, y el 5% pueden requerir ingreso en una Unidad de Cuidados Intensivos. En casos severos, COVID-19 puede complicarse por el síndrome de dificultad respiratoria aguda (SDRA), sepsis y shock séptico y fracaso multiorgánico. Este documento de consenso se ha preparado sobre directrices basadas en evidencia desarrolladas por un panel multidisciplinario de profesionales médicos de cuatro sociedades científicas españolas (Sociedad Española de Medicina Intensiva y Unidades Coronarias [SEMICYUC], Sociedad Española de Neumología y Cirugía Torácica [SEPAR], Sociedad Española de Urgencias y Emergencias [SEMES], Sociedad Española de Anestesiología, Reanimación y Terapéutica del Dolor [SEDAR]) con experiencia en el manejo clínico de pacientes con COVID-19 y otras infecciones virales, incluido el SARS, así como en sepsis y SDRA. El documento proporciona recomendaciones clínicas para el soporte respiratorio no invasivo (ventilación no invasiva, oxigenoterapia de alto flujo con cánula nasal) en cualquier paciente con presentación sospechada o confirmada de COVID-19 con insuficiencia respiratoria aguda.
Esta guía de consenso debe servir como base para una atención optimizada y garantizar la mejor posibilidad de supervivencia, así como permitir una comparación fiable de las futuras intervenciones terapéuticas de investigación que formen parte de futuros estudios observacionales o de ensayos clínicos.
This consensus document has been drafted in response to the current public health emergency and clinicians’ demand for guidelines. As such, it focuses on specific situations encountered outside routine clinical practice in hospitals, and must be adapted to the particular circumstances of any given scenario.
General introductionThis consensus document has been drawn up by the scientific societies involved in treating acute respiratory failure in adult patients. It includes a more detailed description of the recommendations for the use of non-invasive respiratory support (NIRS) in the management of acute respiratory failure (ARF) secondary to infection by the new SARS-CoV-2 coronavirus that causes the disease called COVID-19 that is intended to supplement the regularly updated recommendations issued by the Ministry of Health, Consumer Affairs and Social Welfare (MH).1,2
The World Health Organization (WHO) recently declared the disease caused by SARS-CoV-2 (COVID-19)3 a public health emergency of international concern. The ongoing COVID-19 pandemic is devastating, despite the implementation of extensive control measures. In reality, there are significant regional differences in the availability and accessibility of healthcare resources among the more than 70 countries currently affected by the virus. These differences might partly explain the low mortality rates despite the high number of cases. Health authorities and governments worldwide have developed contingency plans to manage local outbreaks,4 and these measures are essential for controlling the epidemic, protecting health workers on the front line, and mitigating the severity of patient outcomes.
A recent study of clinical characteristics in a selected cohort of 1099 COVID-19 patients across China5 showed that up to15% (173/1099) developed severe disease according to the American Thoracic Society's clinical criteria for severe community-acquired pneumonia,6 and of these 20.6% were at risk of admission to the ICU (33/173, 19%), invasive and non-invasive mechanical ventilation (81/173, 46%) or death (14/173, 8%), while 2.9% (5/173) required extracorporeal oxygenation systems.
Extrapolating these figures to the current situation in Spain compels us to anticipate events and demand that both national and regional health authorities draw up a contingency plan for managing healthcare resources and staff safety. This plan should include the procedures for using specific hospital areas, such as expert units capable of caring for ventilated patients (ICUs, intermediate respiratory care units [IRCU), emergency departments and wards equipped with the resources and staff needed to safely and efficiently deal with the epidemiological challenge of controlling and treating the COVID-19 outbreak in Spain. During the previous SARS (severe acute respiratory syndrome) and MERS (Middle East respiratory syndrome) epidemics, the infection rate among healthcare workers was 18.6% and 21% of cases during the MERS and SARS outbreaks, respectively.7,8
For this reason, both working groups and scientific societies need to establish contingency plans for dealing with an increasingly critical situation and optimize both material and human resources to be prepared to meet unprecedented demands. Specifically, we believe that this contingency plan should include the following strategies:
- •
Ensure that hospital managers establish protocols for personal protective equipment (PPE) for healthcare professionals. Ensure that healthcare personnel are trained in PPE donning and doffing techniques.
- •
Education campaigns, training, and simulation scenarios to assess the hospital staff's capacity to respond to different outbreak scenarios. Optimize and anticipate the human resources needed to improve the safety of healthcare personnel and maintain staff numbers despite absences caused by exposure to COVID-19.
- •
Identify reference hospitals that can safely handle a possible surge in cases.
- •
Increase the total capacity of ICUs and IRCUs, and prepare in advance the material resources, equipment, healthcare personnel, wards and emergency areas needed to cater for COVID-19 patients, if necessary.
- •
Establish a protocol for identifying suspected, probable and confirmed cases and setting in motion the corresponding care pathways.
- •
Establish a protocol for managing suspected severe case of COVID-19.
- •
Establish clear objectives for the care of patients and their families, together with visitation guidelines for hospitalised patients.
In conclusion, we cannot predict how many seriously ill COVID-19 patients we will receive, but we must learn from the experience of other countries and anticipate scenarios, distribute resources as rationally as possible, and do the best we can to be prepared and work together to overcome the epidemic.
The recommendations contained in this consensus document, prepared by the Spanish Society of Intensive and Critical Care and Coronary Units (SEMICYUC), the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR), the Spanish Society of Emergency Medicine (SEMES) and the Spanish Society of Anaesthesiology (SEDAR) are based on studies in other viral pandemics (influenza, SARS, MERS) and on the latest studies published on COVID-19. The level of evidence currently available is therefore low, given the lack of methodological robustness and the very nature of the disease. This document will be updated as the state of the knowledge evolves and changes are made in the recommendations issued by national and international organizations and societies.
General recommendations for the management of acute respiratory failure secondary to COVID-19Objectives- •
To correctly identify patients with ARF who may require non-invasive respiratory support (NIRS).
- •
To describe processes with high risk of NIRS failure.
ARF is the most frequent cause of mortality in patients with influenza and viral infections in general.9 With respect to COVID-19 (the infectious disease caused by SARS-CoV-2), 3.4% of infected patients in China presented with acute respiratory distress syndrome (ARDS), representing 40.3% of patients with severe disease.5 It is therefore essential to implement a therapeutic strategy to treat ARDS secondary to COVID-19 infection.
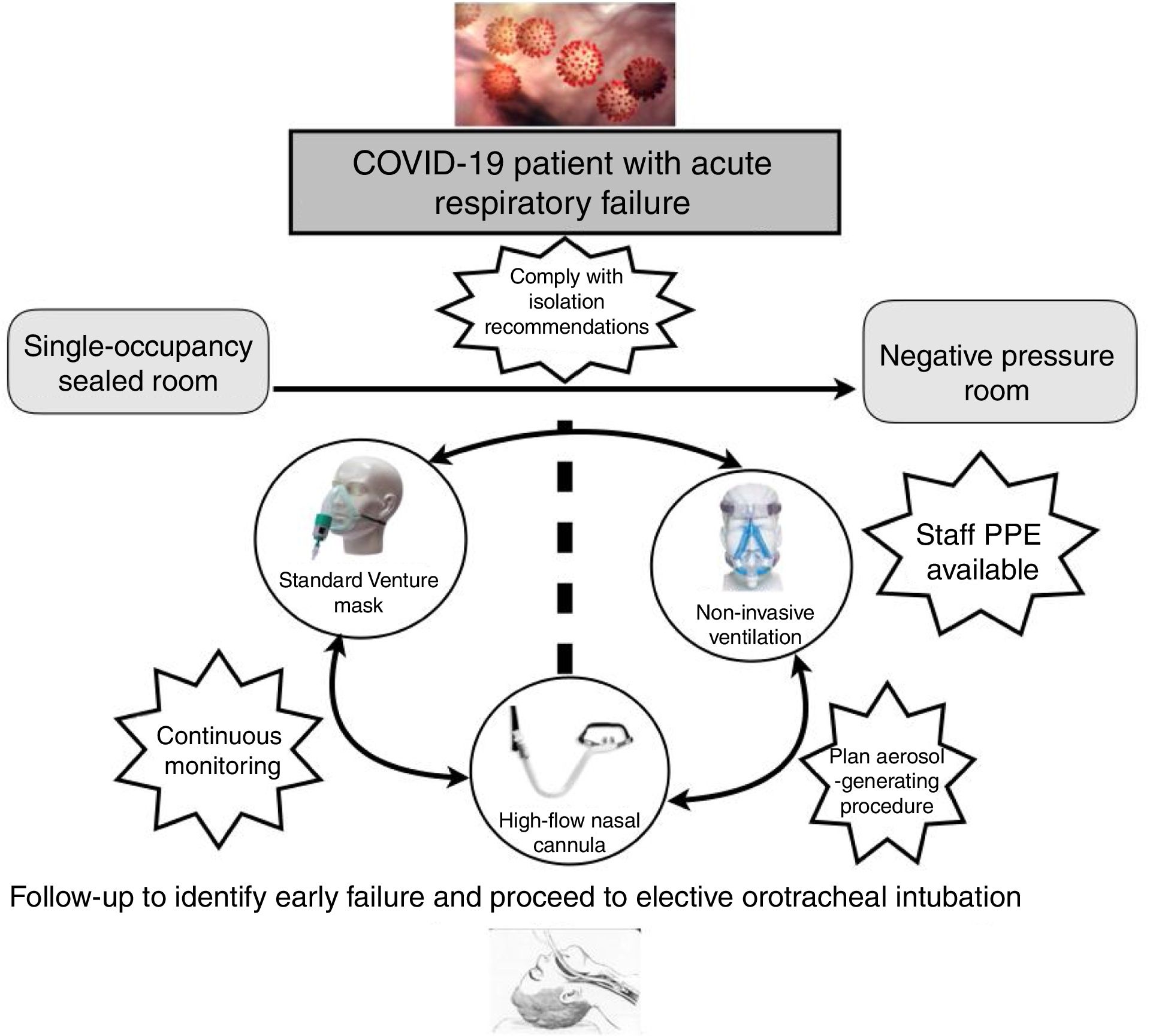
Monitoring, preferably non-invasive, is a key element in the management ARF in patients with COVID-19. These patients need to be placed in individual rooms, ideally with negative pressure, and this calls for centralized monitoring (pulse oximetry, respiratory rate) and, preferably, video surveillance.
Therapeutic strategy for NIRS in COVID-19The escalation therapeutic strategy proposed by Scala and Heunks for processes that cause ARF can also be used In SARS-CoV-2 infection.10 Conventional oxygen therapy, consisting in the administration of oxygen at different concentrations, is the base of the therapeutic pyramid. The next step is high flow nasal oxygen (HFNO) therapy, in which a mixture of varying proportions of air and oxygen (FiO2) are deliver at a high flow rate (up to 60l/min) through a nasal cannula. The gas must be heated and 100% humidified.11 HFNO, compared with conventional oxygen devices, maintains FiO2 at a constant level, reduces dead space, generates positive pressure that redistributes intra-alveolar fluid, and promotes alveolar recruitment.12 The next step is non-invasive ventilation (NIV), which is administered under spontaneous breathing, so patients require very little sedation, or none at all.13 The penultimate step is invasive mechanical ventilation (MV). In this case, volume control mode is usually used, and the patient must be intubated.10 The last step is extracorporeal membrane oxygenation (ECMO).14 The respiratory therapies currently used in NIRS are HFNO and NIV.
On the basis of the above, the general criteria for starting respiratory support in ARF secondary to COVID-19 are as follows15:
Clinical criteria:
- •
Moderate to severe dyspnoea with signs of respiratory effort and use of accessory muscles or paradoxical abdominal movement.
- •
Tachypnoea over 30bpm.
Blood gas criteria:
- •
PaO2/FiO2<200 (or the need for FiO2 greater than 0.4 to achieve an SpO2 of at least 92%).
- •
Acute ventilatory failure (pH<7.35 with PaCO2>45mmHg).
In patients meeting none of the above criteria, the initial treatment indicated is conventional oxygen therapy. In patients meeting one or more of the criteria, respiratory support, either invasive or non-invasive, is indicated. The use of NIRS for SARS and other viral pandemics is controversial, and in this context NIV failure rates are around 30%.16
More recently, NIV was also used in patients with ARF secondary to swine flu, with failure rates ranging from 13% to 77%.17–19 Despite the uncertainty of the evidence and the absence of randomized clinical trials, most observational studies suggest that NIV can be considered in carefully selected patients treated in a protected environment (ideally negative pressure rooms) in hospitals with experience in this technique. In the current epidemic in China, 5.1% of patients required NIV, 2.3% required MV and 0.5% ECMO.5 Therefore, the choice of therapy will also depend on the patient's basic pathology, mainly respiratory, their location (negative pressure room, sealed individual room with air changes) and the potential need for aerosol-generating procedures. Overall, clinicians can encounter three clinical scenarios:
- 1.
Patients with no previous pathology (de novo ARF) and hypoxaemic respiratory failure who, therefore, are at risk for escalation to ECMO. The failure rate of NIRS, mainly NIV, in this clinical scenario is extremely high, and there is evidence of higher mortality if MV is delayed. Therefore, we do not recommend NIRS in these patients.1,20,21 NIRS should only be considered in carefully selected patients, provided all the following criteria are met19,21–27:
- •
PaO2/FiO2>100 despite conventional oxygen therapy.
- •
No multi-organ failure (APACHE<20).
- •
Availability of an expert team and continuous monitoring. For this reason, NIRS should be administered in special units with a pre-established nursing ratio, such as ICUs and IRCUs.
- •
Early intubation (within the hour) if there is no improvement. For example, in addition to standard intubation criteria, intubation could be considered in patients treated with HFNO who have an ROX index (ratio of SpO2/FiO2 to respiratory rate) <3, <3.5 and <4 at 2, 6 and 12h from the start of HFNO therapy. Similarly, intubation could be considered in patients with a Heart rate, Acidosis (pH), Consciousness (GCS), Oxygenation, and Respiratory rate (HACOR) score >5 after 1h of NIV.
Extrapolating the evidence in de novo ARF, HFNO would be the treatment of choice.21,28 NIV is the second line option if response is poor but MV criteria are not met.
- •
- 2.
Patients with hypoxaemic respiratory failure, a do not intubate order, in whom NIV is the ceiling of therapy. NIRS is indicated in these patients, provided precautionary measures are in place. In this case, it is essential to establish the treatment objectives with the patient and their family by defining the ceiling of therapy. Generally speaking, treatment should start with HFNO before progressing to NIV.21,28 NIRS should be administered as follows29,30:
- 3.
Patients with severe exacerbation of COPD with acute or exacerbated hypercapnic respiratory failure: perform a therapeutic test with NIRS, particularly NIV. In these cases, HFNO can be useful if the patient cannot tolerate NIV, or it can be used during NIV rest periods.33–36
To limit transmission of infection to both healthcare personnel and other patients.
IntroductionThe use of NIRS carries a high risk of SARS-CoV-2 transmission.37–40 The capacity of SARS-CoV-2 to infect healthcare workers has been confirmed, although it is still too early to compare it with MERS and SARS.40 For this reason, the Ministry of Health, Consumer Affairs and Social Welfare has drawn up a series of recommendations for managing the disease, and the aim of this document is to disseminate measures for limiting transmission to healthcare personnel.2,39 It is imperative for hospital staff to follow the general preventive measure when administering NIRS in patients with suspected or confirmed SARS-CoV-2 infection, and in order to do so, the authorities must ensure sufficient supplies of protective material for safe NIRS.
General recommendations- (a)
Healthcare personnel caring for patients with suspected or confirmed COVID-19 receiving NIRS must wear personal protective equipment (PPE) to prevent infection2,22,37,39,41 when performing aerosol-generating procedures that have been associated with an increased risk of transmission of airborne pathogens. Preventive measures should protect against microorganisms transmitted by droplets and contact, including:
- •
A high efficiency FFP2 mask or preferably FFP3, if available.
- •
Goggles
- •
Tie long hair in a ponytail or low bun and wear a surgical cap.
- •
Gloves.
- •
Long-sleeve fluid resistant isolation gowns.
- •
- (b)
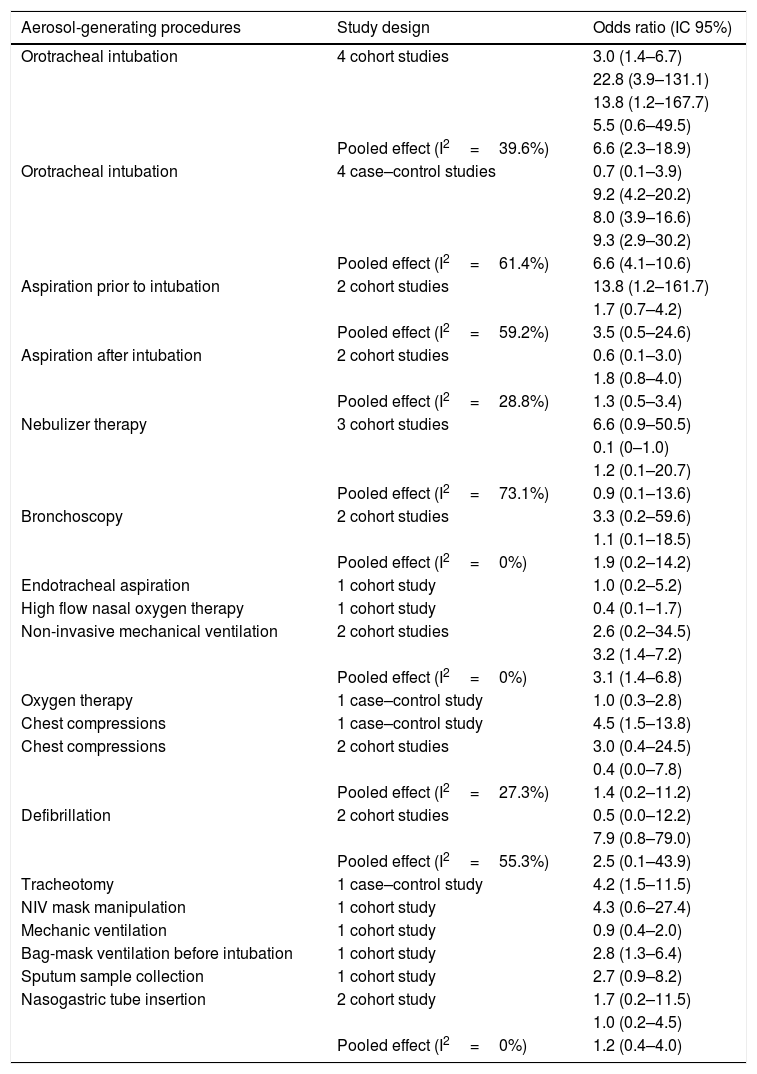
The feasibility of performing aerosol-generating procedures will depend on the patient's location within the hospital. Most of the evidence available on NIRS devices as invasive procedures and the risk of transmitting respiratory pathogens to healthcare staff concerns orotracheal intubation, patients with artificial airways, and non-invasive ventilation, although the results come from small, low-quality studies and are therefore difficult to interpret (Table 1). In mild cases, therefore, the patient should be placed in a negative pressure room. If this is not available, the patient should be place in a single-occupancy room with bathroom. The door of the room must be closed at all times.39 Serious cases with severe hypoxaemia should be admitted to special units.
Table 1.Summary of aerosol-generating procedures and risk of transmission of acute respiratory diseases.
Aerosol-generating procedures Study design Odds ratio (IC 95%) Orotracheal intubation 4 cohort studies 3.0 (1.4–6.7) 22.8 (3.9–131.1) 13.8 (1.2–167.7) 5.5 (0.6–49.5) Pooled effect (I2=39.6%) 6.6 (2.3–18.9) Orotracheal intubation 4 case–control studies 0.7 (0.1–3.9) 9.2 (4.2–20.2) 8.0 (3.9–16.6) 9.3 (2.9–30.2) Pooled effect (I2=61.4%) 6.6 (4.1–10.6) Aspiration prior to intubation 2 cohort studies 13.8 (1.2–161.7) 1.7 (0.7–4.2) Pooled effect (I2=59.2%) 3.5 (0.5–24.6) Aspiration after intubation 2 cohort studies 0.6 (0.1–3.0) 1.8 (0.8–4.0) Pooled effect (I2=28.8%) 1.3 (0.5–3.4) Nebulizer therapy 3 cohort studies 6.6 (0.9–50.5) 0.1 (0–1.0) 1.2 (0.1–20.7) Pooled effect (I2=73.1%) 0.9 (0.1–13.6) Bronchoscopy 2 cohort studies 3.3 (0.2–59.6) 1.1 (0.1–18.5) Pooled effect (I2=0%) 1.9 (0.2–14.2) Endotracheal aspiration 1 cohort study 1.0 (0.2–5.2) High flow nasal oxygen therapy 1 cohort study 0.4 (0.1–1.7) Non-invasive mechanical ventilation 2 cohort studies 2.6 (0.2–34.5) 3.2 (1.4–7.2) Pooled effect (I2=0%) 3.1 (1.4–6.8) Oxygen therapy 1 case–control study 1.0 (0.3–2.8) Chest compressions 1 case–control study 4.5 (1.5–13.8) Chest compressions 2 cohort studies 3.0 (0.4–24.5) 0.4 (0.0–7.8) Pooled effect (I2=27.3%) 1.4 (0.2–11.2) Defibrillation 2 cohort studies 0.5 (0.0–12.2) 7.9 (0.8–79.0) Pooled effect (I2=55.3%) 2.5 (0.1–43.9) Tracheotomy 1 case–control study 4.2 (1.5–11.5) NIV mask manipulation 1 cohort study 4.3 (0.6–27.4) Mechanic ventilation 1 cohort study 0.9 (0.4–2.0) Bag-mask ventilation before intubation 1 cohort study 2.8 (1.3–6.4) Sputum sample collection 1 cohort study 2.7 (0.9–8.2) Nasogastric tube insertion 2 cohort study 1.7 (0.2–11.5) 1.0 (0.2–4.5) Pooled effect (I2=0%) 1.2 (0.4–4.0) CI: confidence interval; I2: heterogeneity index.
Results of studies selected for the systematic review that measure the risk of transmission of SARS to healthcare workers exposed vs. not expose to the procedures listed.48,49
- (c)
For intrahospital transfer, both the patient and the staff member transferring the patient must wear surgical masks. During transfer, the patient's bed must be covered with a clean disposable sheet that is then removed and disposed of as hazardous medical waste (group 3, biological agents).39
The Ministry of Health, Consumer Affairs and Social Welfare recommends administering oxygen through masks with an exhalation filter, but these masks are not universally available in our setting. In the absence of such masks, a surgical mask can be safely placed over the nasal prongs or oxygen mask to limit the spread of the virus. There are no studies comparing the efficacy of exhalation filter masks and surgical masks in reducing the spread of SARS-CoV-2,39 but oxygen therapy is considered a low-risk aerosol-generating procedure.39,40
High flow nasal oxygen therapyThe aforementioned general recommendations should be followed, observing a minimum distance of 2m between patients and healthcare personnel without adequate protection.42 Although the extent of particle dispersion in this type of therapy remains unclear, and the benefit of placing a surgical mask over the nasal prongs has not been studied, it is an option in an extreme situation.
Non-invasive mechanical ventilationA minimum distance of 2m should be maintained between patients and healthcare personnel without adequate protection.
In general, according to the available evidence, the use of NIRS is not contraindicated in patients with COVID-19, but the respiratory therapy used will not only depend on the severity of the respiratory failure but also on the availability of a room that complies with the isolation and safety recommendations of the World Health Organization (WHO). The most serious cases that will probably require rapid intubation should be placed in the ICU in order to avoid intubation delays that would affect the patient's evolution (Fig. 1).
- 1.
Ventilator settings:
- •
Although there are uncertainties surrounding particle dispersion in COVID-19, in the SARS epidemic some articles showed particle dispersion to a radius of no more that 4 feet (1.25m) when using a single-limb circuit with a leak port.8,43,44
- •
Double limb circuits are preferable, since they prevent air leaks from both the inspiratory and expiratory breathing circuits. High efficiency antibacterial expiratory filters should be used to avoid reverse contamination from the patient to the ventilator.39
- •
If double limb systems are unavailable and single limb ventilators are unavoidable, attach a high-efficiency, low resistance antimicrobial filter to the leak port of the single limb to minimize dispersion of exhaled gas that may contaminate ambient air. It also appears feasible to connect a T valve to the circuit in order to place the filter and leak port distal to the valve, although this will increase dead space.
- •
If an antimicrobial filter cannot be connected to the leak port, a similar filter must be placed between the patient/ventilator interface (no leak ports) and the circuit. In this case, the ventilator settings may need to be adjusted to increase pressure support to compensate for the increased resistance.
- •
Instead of double limb or single limb systems with leak port, a single-limb systems with an active valve can be used, placing an antimicrobial filter at the outlet of the active valve.
- •
We do not recommend using heat and moisture exchangers (HME).45
- •
- 2.
Choice of interface:
The interface is the device that facilitates both the physical and functional relationship between two independent elements: the ventilator and the patient. It is an indispensable element in NIV, and delivers positive pressure to the patient without the need for an artificial airway. The recommendations for NIV interfaces in SARS-CoV-2 infection are as follows40,41,46,47:
- •
An interface without a leak port should be used, and accessory ports, if any, should not be used.
- •
The use of helmets should be prioritized if available and staff are trained in the placement and use of this device.
- •
In general terms, the first alternative to the helmet is the full face mask and, failing that, the oronasal mask.
- •
Face mask should be monitored for leaks, particularly oronasal interfaces. Any leaks should be corrected, primarily to avoid injuries to the patient's skin, but also to ensure the integrity of the closed circuit and prevent exhalation of contaminated air. Protective patches, which can increase leakage, should be avoided, and hyper oxygenated oil should be applied as required.
- •
Nasal masks are not recommended as they generate more aerosols, and because SARS-CoV-2 infection usually involves acute hypoxaemic failure.
- •
- 3.
Choice of elbow46:
- •
We recommend using elbows without an anti-asphyxia valve. These elbows are usually colour-coded blue, and require strict monitoring to guard against possible ventilator malfunction. However, the risk/benefit balance (asphyxia vs. dispersion) favours these elbows, and there is little risk of accidental disconnection that remains undetected or is not corrected in time, since these patients are located in highly complex rooms under the continuous care of specialized healthcare personnel. Nevertheless, the nurse-patient ratio must remain above the minimum safe level.
- •
We advise against the use of anti-rebreathing elbows (which have anti-asphyxia valves) due to the risk of greater dispersion of exhaled air.
- •
The current pandemic of COVID-19 cases requires infection control precautions to be maximized. Nebulizers generate aerosol particles of between 1 and 5μm that can carry bacteria and viruses to the lung. The risk of transmitting infection through droplet nuclei and aerosols may increase when using nebulizers due to their potential to generate a high volume of respiratory aerosols that can be propelled further than the distance achieved by natural dispersion. Furthermore, larger particles can stimulate coughing in patients and passers-by, thereby increasing the risk of disease spread. Nebulizer therapy in patients with COVID-19 infection has the potential to transmit potentially viable COVID-19 to susceptible subjects.
Some hospitals have recently replaced nebulizers with metered-dose inhalers (MDI) with spacers or valved-holding chambers (VHC). Inhaled therapy should preferably be administered with an MDI with a VHC; however, it is important to note that patients with acute respiratory failure will have difficulties using these devices.
Nebulizer therapy should only be used in the following situations:
- 1.
Severe, life-threatening respiratory disease (e.g., patients with hypoventilation or compromised ventilation, severe COPD, or cystic fibrosis).
- 2.
Patients that are unable to cooperate or cannot follow the instructions required for an MDI with VHC.
- 3.
Poor responders to MDI+VHC therapy.
Despite the large body of evidence showing their lack of superiority, or inferiority, to MDI+VHC, “open” nebulizers are still widely used in hospital settings.
In order to reduce the risk of in-hospital transmission of infectious respiratory diseases in the context of the current COVID-19 pandemic, we encourage all healthcare professionals to seriously consider avoiding the use of open nebulizers in spontaneously breathing patients if the aforementioned inhalers are not available. Patient and staff safety must be our top priority.
If inhaled therapy is indicated, we recommend using vibrating mesh nebulizers with a mouthpiece or face mask. The risk of dispersion can be reduced by placing a surgical mask over the device. Bear in mind that a higher drug dose may be needed if a mouthpiece with an anti-dispersion valve is used (particularly in the case of beta2-adrenergic agonist bronchodilators), so the prescription should be adjusted accordingly.
Jet systems have a greater capacity for particle dispersion than other nebulizers, and should therefore be avoided. If unavoidable, the nebulizer must be covered with a surgical mask.
When using inhaled therapy in combination with NIRS, we recommend the following:
- •
Generally speaking, inhaled therapy should be administered via a pressurized cartridges with an adapter or spacer chamber. If used in combination with NIV, the nebulizer should be connected to the inspiratory limb of the ventilator and the aerosol drug should be delivered during inspiration.
- •
If aerosol therapy is used, the first choice should be a circuit with a vibrating mesh nebulizer elbow. Failing this, a vibrating mesh nebulizer can be connected to the NIV circuit using a T valve. Being a “closed system” there is no risk of dispersion, provided the mask is closely monitored for unintentional leaks.
- •
Jet nebulizers with a T tube generate greater turbulence, larger particles, and therefore a higher risk of particle dispersion.
- •
In patients receiving HFNO, pressurized metered dose inhalers with spacer, a mouthpiece with a vibrating mesh nebulizer or a mesh nebulizer connected to the dry limb of the water reservoir should be used.
- •
Generally speaking, pressure support in NIV and temperature in HFNO should be reduced, respectively, when combined with aerosol therapy.
Please cite this article as: Cinesi Gómez C, Peñuelas Rodríguez Ó, Luján Torné Ml, Egea Santaolalla C, Masa Jiménez JF, García Fernández J, et al. Recomendaciones de consenso respecto al soporte respiratorio no invasivo en el paciente adulto con insuficiencia respiratoria aguda secundaria a infección por SARS-CoV-2. Rev Esp Anestesiol Reanim. 2020;67:261–270.