Surgical treatment during Covid-19 pandemic is controversial. Currently, most clinical guidelines advise to defer surgical patients during the Covid-19 pandemic, although the supporting data is sparse. We assumed that a Covid-19-free hospital, on the back of strong isolation measures and targeted screening, could reduce complications and enable us to continue treating high-risk patients.
MethodsProspective study with retrospective analysis of 355 patients who had undergone nondeferrable oncological surgery between March 16th, 2020, and April 14th, 2020, at our institution. The aim of the study was to assess the hospital restructuring and surgical protocols to be able to safely handle non-deferrable surgeries during the first wave of the Covid-19 pandemic. We implemented structural changes and an updated surgical-anesthetic protocol in order to isolate Covid-19 patients from other surgical patients. Comprehensive targeted screening for Covid-19 patients was made. PCR tests were requested for suspected Covid-19 patients. We analyzed mortality and complications related to both surgery and Covid-19 during hospital admission and also 15 and 30 days after surgery. We compared it with a sample of similar patients in the pre-pandemic period.
ResultsOf the 355 patients enrolled in our study, 21 were removed due to Covid-19 infection, leaving a total of 334 patients in our final analysis. Post-operative complications were found in 37 patients (11.07%). Two patients died after surgery (0.6%). At the end of the study, Covid-19-related adverse outcomes were detected in six patients (1.79%). When comparing the complications of our original sample with the complications that occurred in the pre-covid era, we found no statistically significant differences.
ConclusionsOur results show that the surgical treatment of oncologic patients during the Covid-19 pandemic is safe, as long as the hospital performs surgeries under strict isolation measures and a robust screening method. It is necessary to select Covid-19 free hospitals for this matter in this and future pandemics.
El tratamiento quirúrgico durante la pandemia de Covid-19 es controvertido. Actualmente, la mayoría de las guías clínicas recomiendan posponer la cirugía a los pacientes durante la pandemia de Covid-19, aunque los datos de apoyo son escasos. Asumimos que un hospital sin Covid-19, apoyado en fuertes medidas de aislamiento y exámenes de detección específicos, podría reducir las complicaciones y permitirnos continuar tratando a pacientes de alto riesgo.
MétodosEstudio prospectivo con análisis retrospectivo de 355 pacientes sometidos a cirugía oncológica no diferible entre el 16 de marzo de 2020 y el 14 de abril de 2020 en nuestra institución. El objetivo del estudio fue valorar la reestructuración hospitalaria y de los protocolos quirúrgicos para poder manejar con seguridad las cirugías no diferibles durante la primera ola de pandemia por Covid-19. Implementamos cambios estructurales y un protocolo de anestésico-quirúrgico actualizado para aislar a los pacientes con Covid-19 de otros pacientes quirúrgicos. Se realizó una evaluación exhaustiva dirigida a detectar pacientes con Covid-19. Se solicitaron pruebas de PCR para pacientes sospechosos de Covid-19. Analizamos la mortalidad y las complicaciones relacionadas tanto con la cirugía como con la Covid-19 durante el ingreso hospitalario y también a los 15 días y al mes de la cirugía. Comparamos nuestros resultados con una muestra de pacientes similar en el periodo pre-pandemia.
ResultadosDe los 355 pacientes incluidos en nuestro estudio, 21 fueron eliminados debido a la infección por Covid-19, lo que deja un total de 334 pacientes en nuestro análisis final. Se encontraron complicaciones postoperatorias en 37 pacientes (11,07%). Dos pacientes fallecieron tras la cirugía (0,6%). Al final del estudio, se detectaron resultados adversos relacionados con Covid-19 en seis pacientes (1,79%). Al comparar las complicaciones de nuestra muestra original con las que ocurrieron en la era pre-Covid-19, no encontramos diferencias estadísticamente significativas.
ConclusionesNuestros resultados muestran que el tratamiento quirúrgico de los pacientes oncológicos durante la pandemia de Covid-19 es seguro, siempre que el hospital realice cirugías bajo estrictas medidas de aislamiento y un método de detección robusto. Es necesario seleccionar hospitales libres de Covid-19 con este objetivo en esta y futuras pandemias.
In December 2019, the first cases of COVID-19 infection were reported in Wuhan, China. By early 2020, the situation had turned into an epidemic, and by March 2020 it had been declared a global pandemic1. The incubation period for this infection is up to 2 weeks, during which time the virus is extremely contagious, making it very difficult to identify and isolate asymptomatic carriers2.
On 15 March 2020, the Spanish government declared a state of alarm3. Almost every hospital in the country was ordered to prioritize COVID-19 cases, and beds were therefore only available for COVID patients and those with life-threatening disease. As the situation worsened, the government designated intensive care units (ICU) and operating rooms to handle the treatment of complicated cases of COVID-19. Cancer surgery was delayed, because short-term COVID-19 mortality rate could not be compared to other diseases.
Chemotherapy, radiation therapy, cancer surgery, and diagnostic and follow-up tests were also delayed, jeopardizing cancer diagnoses and the possibility of administering effective treatment4.
Current evidence suggests that symptoms of COVID-19 are more serious in cancer patients, so it is important to assess the risk-benefit ratio in this type of patient5. Opinions varied on whether cancer treatments should be postponed or not, and there were no conclusive studies in this regard. A recent study showed high mortality in asymptomatic patients who underwent elective surgery6.
The risk of COVID-19 transmission can be minimized by efficient in-hospital containment measures. A good screening method is key to detecting patients with COVID-19 infection before surgery and identifying possible vectors among hospital staff. A well-organised care pathway and a small, experienced team of surgeons and anaesthesiologists is equally important. Close collaboration between anaesthesiologists and surgeons is essential in this process. We therefore need to establish protocols to ensure that patients can receive their treatment, including non-deferrable surgeries, without becoming infected with COVID-19.
MethodsDesignWe decided to perform this study after the Ministry of Health designated our hospital as the main centre for non-deferrable cancer surgery in our city, since many hospitals had been allocated exclusively to the treatment of COVID-19 patients. This prospective observational study was approved by the hospital's ethics committee (MD20/004 April 20, 2020). All patients gave their informed consent for their data to be processed for research purposes. All authors reviewed the text and verified the accuracy of the data and overall compliance with the protocol. The patients were included from 16 March 2020, 2 days after the declaration of a state of emergency in Spain, to 14 April 2020. This period, which encompassed the weeks with the highest incidence of the disease, was a particularly challenging time. Data were collected from patient medical records. Structural modifications were made to the hospital to create two difference care pathways in which an entire floor and 4 ICU beds were set aside for the exclusive care of cancer patients with COVID-19. All the physicians and nurses on this floor were involved exclusively in the treatment of COVID-19 patients and had no contact with other areas. The remaining floors were dedicated to the care of postoperative patients without COVID-19.
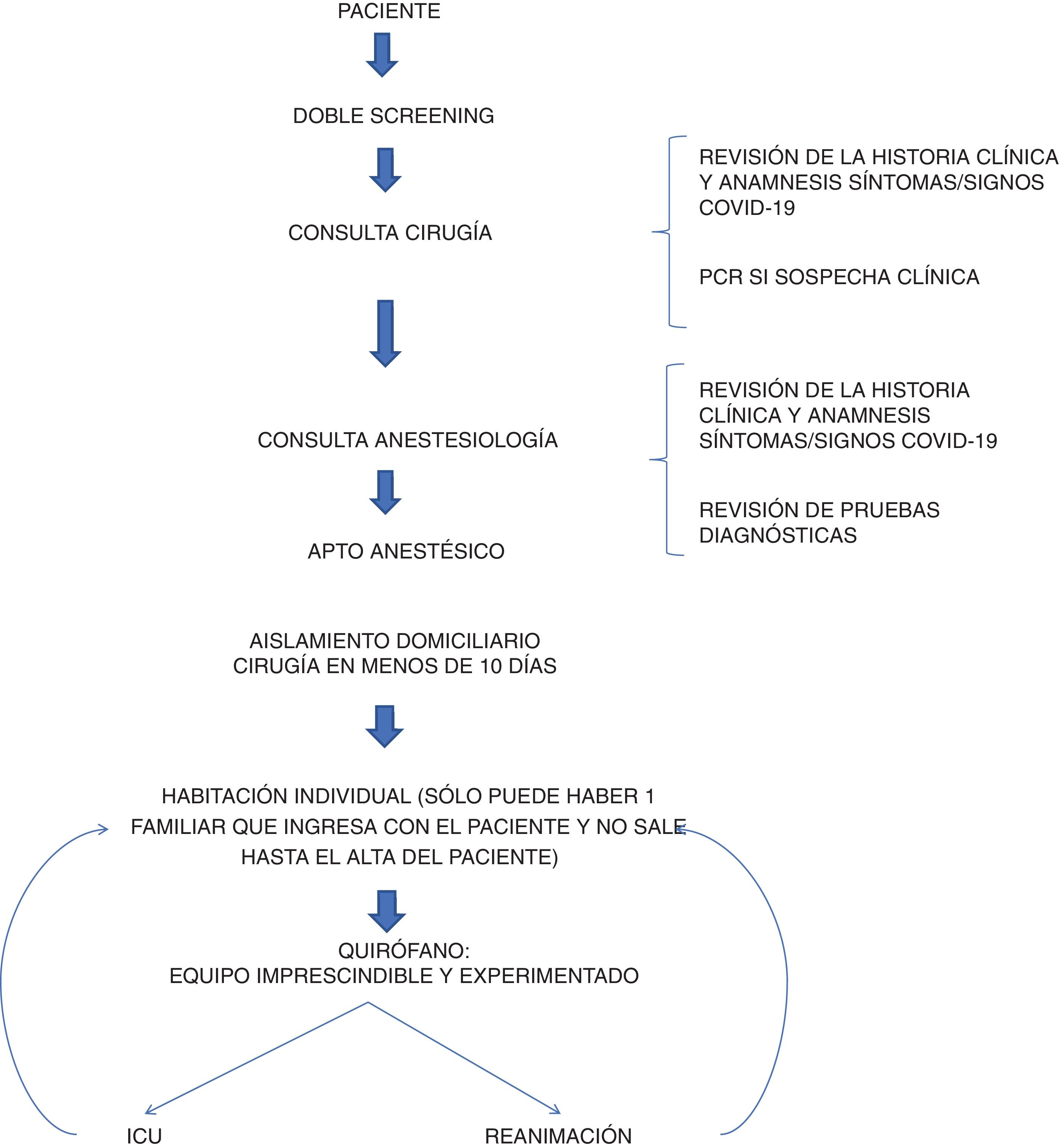
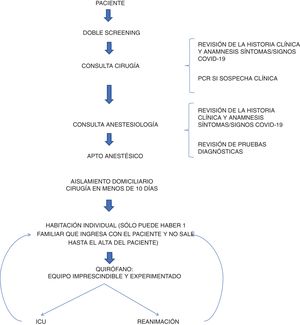
A surgical protocol was established for patients undergoing surgery during the epidemic. A double screening strategy was implemented to identify patients with symptoms of COVID-19 in both the pre-surgery and pre-anaesthesia consultation. The surgeon established the indication for surgery after reviewing the patient’s history, and interviewed the patient in detail to detect any possible COVID-19 infection. All tests and consultations were performed on the same day to minimize unnecessary hospital visits. It was mandatory for all patients to have preoperative lab tests (hemogram, biochemistry and clotting) and a chest X-ray reviewed by a specialized chest radiologist. If the radiography was suspicious, a chest computed tomography (CT) scan was requested and was reviewed by the radiologist. If the report was inconclusive, the images were evaluated by another radiologist—a chest specialist. Finally, the results were reviewed in the anaesthesia consultation, in which the patient was again interrogated for symptoms of infection or epidemiological risk factors for COVID-19 and the appropriate anaesthesia strategy was decided. At that time, the shortage of polymerase chain reaction (PCR) kits in Spain limited testing to patients with a strong suspicions of infection. Isolation measures were taken. The patients were ordered to observe strict home isolation in the days prior to the test. Efforts were made to shorten the time between consultation and surgery to less than10 days on average.
The surgical protocol was as follows (Fig. 1): the patient was admitted the same day of surgery and was isolated in a room until he or she was taken to the operating room. Mask and gloves were mandatory in all patients from the time of admission to anaesthesia induction. The patient was monitored and anaesthetized by a team wearing personal protective equipment (PPE) that was changed after treating each patient. Endotracheal intubation was performed with a video laryngoscope, avoiding manual ventilation and the use of aerosol-generating laryngeal masks and other devices. For the same reason, spinal/epidural anaesthesia was used whenever possible. Both medical and nursing staff wore full PPE, and the number of staff present during each intervention was minimised as far as possible. When laparoscopy was performed, a closed suction system was used until the end of the surgery to avoid aerosolization. In the case of surgeries with a high risk of infection, such as ENT procedures, the surgical team used an FPP2 mask. Conventional surgical masks were used in all other procedures. The operating room was meticulously cleaned between patients and disinfected using a 1:10 bleach solution before and after surgery. The entire facility was cleaned with the same product every 4 h. After surgery, patients were transferred to a resuscitation unit, from where they were transferred to the surgical ward as soon as possible, or remained in the ICU for 24 h, depending on the type of surgery performed. Once on the ward, an enhanced recovery after surgery (ERAS) protocol was implemented in all patients who met the corresponding criteria. If the patient presented any complications after hospital discharge, they were instructed to go to our hospital emergency department for evaluation.
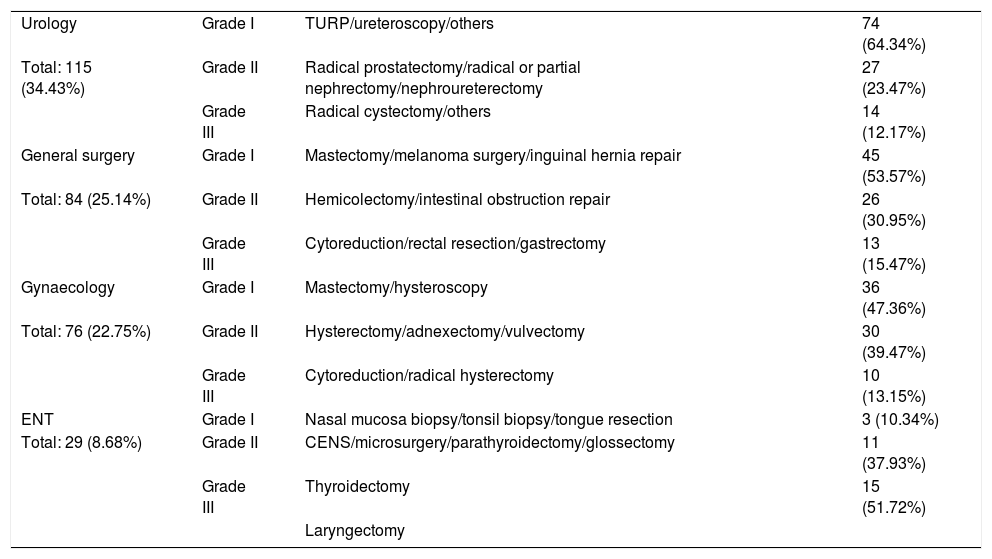
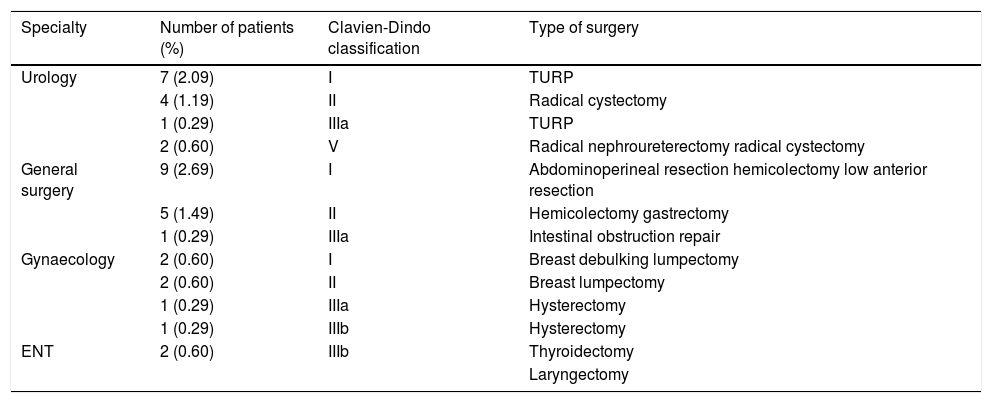
Surgeries were classified into 3 levels, according to their complexity: Level 1 includes procedures involving minor risks and general technical difficulties. Level 2 includes complex procedures with a moderate risk and technical difficulties. Level 3 includes very complex procedures with high technical difficulties. Table 1 summarizes surgeries by specialty.
Surgical procedures.
| Urology | Grade I | TURP/ureteroscopy/others | 74 (64.34%) |
| Total: 115 (34.43%) | Grade II | Radical prostatectomy/radical or partial nephrectomy/nephroureterectomy | 27 (23.47%) |
| Grade III | Radical cystectomy/others | 14 (12.17%) | |
| General surgery | Grade I | Mastectomy/melanoma surgery/inguinal hernia repair | 45 (53.57%) |
| Total: 84 (25.14%) | Grade II | Hemicolectomy/intestinal obstruction repair | 26 (30.95%) |
| Grade III | Cytoreduction/rectal resection/gastrectomy | 13 (15.47%) | |
| Gynaecology | Grade I | Mastectomy/hysteroscopy | 36 (47.36%) |
| Total: 76 (22.75%) | Grade II | Hysterectomy/adnexectomy/vulvectomy | 30 (39.47%) |
| Grade III | Cytoreduction/radical hysterectomy | 10 (13.15%) | |
| ENT | Grade I | Nasal mucosa biopsy/tonsil biopsy/tongue resection | 3 (10.34%) |
| Total: 29 (8.68%) | Grade II | CENS/microsurgery/parathyroidectomy/glossectomy | 11 (37.93%) |
| Grade III | Thyroidectomy | 15 (51.72%) | |
| Laryngectomy |
ESS: endoscopic sinus surgery; TURP: transurethral resection of the prostate.
During the postoperative evaluation the clinician paid particular attention to possible symptoms of COVID-19. Patients were seen at the surgery outpatient clinic within 10–20 days of discharge.
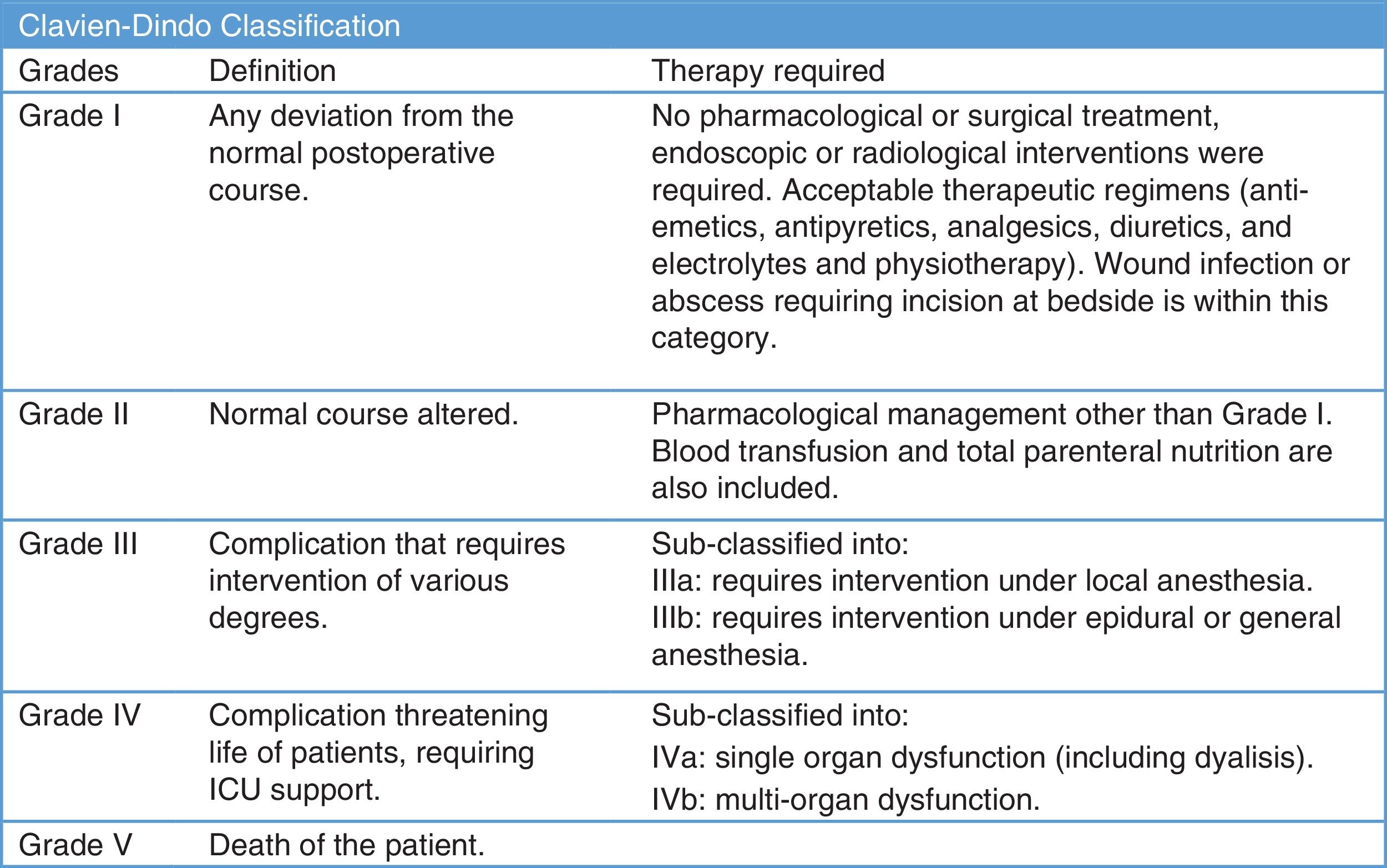
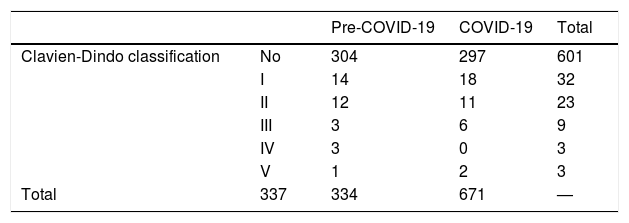
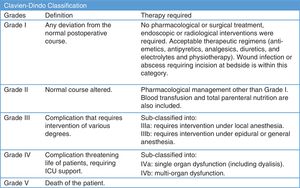
Surgical complications were monitored following the Clavien-Dindo classification7 (Fig. 2). Perioperative mortality was analysed together with COVID-19-related complications during hospitalization and also 15 and 30 days after surgery.
We compared these results with a similar sample of patients undergoing similar surgeries before the outbreak of the COVID pandemic. We also recorded the incidence of COVID-19 infection among our surgical staff.
Statistical analysisContinuous variables are presented as median and interquartile range (IQR). Categorical variables are described as numbers and percentages. Differences between categorical variables were analysed using the Chi-square test or Fisher's exact test. Differences between continuous variables were analysed using Student's t-test. A value of P < .05 was considered statistically significant. All statistical analyses were performed on SPSS® (version 25.0) (SPSS Inc., Chicago, IL, USA).
ResultsA total of 355 patients were initially included in the study. Twenty-one of these patients were excluded because they met clinical criteria for COVID-19 infection or their imaging tests were compatible with the disease (interstitial infiltrates on chest x-ray or chest CT) and they tested positive for COVID-19 on PCR testing. Therefore, a total of 334 patients were finally included in the study.
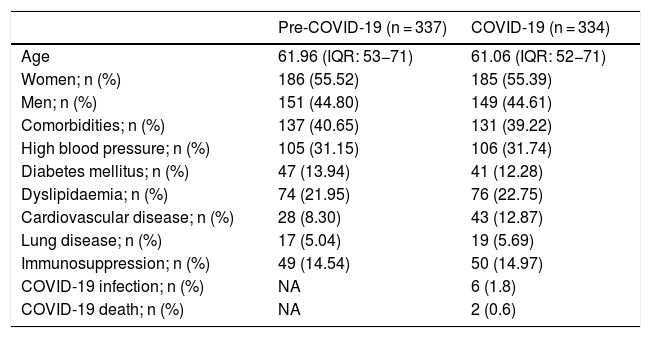
Clinical featuresThe characteristics of the study patients are shown in Table 2.
Demographic variables.
| Pre-COVID-19 (n = 337) | COVID-19 (n = 334) | |
|---|---|---|
| Age | 61.96 (IQR: 53−71) | 61.06 (IQR: 52−71) |
| Women; n (%) | 186 (55.52) | 185 (55.39) |
| Men; n (%) | 151 (44.80) | 149 (44.61) |
| Comorbidities; n (%) | 137 (40.65) | 131 (39.22) |
| High blood pressure; n (%) | 105 (31.15) | 106 (31.74) |
| Diabetes mellitus; n (%) | 47 (13.94) | 41 (12.28) |
| Dyslipidaemia; n (%) | 74 (21.95) | 76 (22.75) |
| Cardiovascular disease; n (%) | 28 (8.30) | 43 (12.87) |
| Lung disease; n (%) | 17 (5.04) | 19 (5.69) |
| Immunosuppression; n (%) | 49 (14.54) | 50 (14.97) |
| COVID-19 infection; n (%) | NA | 6 (1.8) |
| COVID-19 death; n (%) | NA | 2 (0.6) |
IQR: interquartile range.
All 334 patients included in this study lived in Madrid, at that time one of the world epicentres of the pandemic. The age range was 17–92 years, with a median age of 61 (IQR: 52−71); 55.4% of the patients were women and 41 (39.4%) were admitted to the ICU due to high-risk surgery. Their mean stay was 1.06 days.
The most frequency comorbidities were high blood pressure in106 (31.7%), diabetes mellitus in 41 (12.2%), dyslipidaemia in 76 (22.7%), and cardiovascular disease in 43 (12.8%) patients. Nineteen patients (5.6%) presented COPD, while 50 (14.9%) had some degree of immunosuppression.
Surgical outcomesOf the 334 surgeries performed, 115 were urological (34.43%), 84 corresponded to general surgery (25.14%), 76 to gynaecology (22.75%), 29 to ENT (8.68%), and 30 (8.98%) to other specialties (neurosurgery, plastic surgery, orthopaedic, and thoracic surgery. High complexity surgery was performed in 94 level 2 patients (28.14%) and 52 level 3 patients (15.56%).
Perioperative complicationsPerioperative complications were classified according to the Clavien-Dindo classification7 (Table 3). Thirty-seven patients had postoperative complications (11.07%), 29 were minor and did not require reoperation; 8 patients had to undergo surgical exploration; 5 patients (1.49%) were readmitted to the ICU and 2 of them died after surgery (0.6%) after evidence of COVID-19 infection.
Complications.
| Specialty | Number of patients (%) | Clavien-Dindo classification | Type of surgery |
|---|---|---|---|
| Urology | 7 (2.09) | I | TURP |
| 4 (1.19) | II | Radical cystectomy | |
| 1 (0.29) | IIIa | TURP | |
| 2 (0.60) | V | Radical nephroureterectomy radical cystectomy | |
| General surgery | 9 (2.69) | I | Abdominoperineal resection hemicolectomy low anterior resection |
| 5 (1.49) | II | Hemicolectomy gastrectomy | |
| 1 (0.29) | IIIa | Intestinal obstruction repair | |
| Gynaecology | 2 (0.60) | I | Breast debulking lumpectomy |
| 2 (0.60) | II | Breast lumpectomy | |
| 1 (0.29) | IIIa | Hysterectomy | |
| 1 (0.29) | IIIb | Hysterectomy | |
| ENT | 2 (0.60) | IIIb | Thyroidectomy |
| Laryngectomy |
TURP: transurethral resection of the prostate.
Two patients (ENT) underwent exploration under general anaesthesia for bleeding; another patient (gynaecology) presented symptoms of acute abdomen 11 days after surgery. Exploratory laparotomy showed no abnormalities. PCR for COVID-19 was negative. The patient subsequently recovered without incident.
Two patients (urology) died, 1 in hospital, and the other after discharge.
The first death was that of a patient who had undergone nephroureterectomy. Three days after surgery, he required urgent surgical exploration due to signs of intestinal obstruction; intraoperative findings were purulent peritoneal fluid and intestinal distention, with no clear cause. After reoperation, the patient was admitted to the ICU with respiratory distress and acute renal failure.
The postoperative chest radiograph showed bilateral interstitial infiltrate suggestive of pulmonary oedema. The patient died 3 h after admission to the ICU. The cause of death could have been confirmed with an autopsy, but unfortunately this procedure had been banned at the start of the pandemic8. Nevertheless, the patient’s respiratory symptoms and radiological findings suggested infection by COVID-19.
The second death was a patient (radical cystectomy) who developed symptoms of COVID-19 (fever, dyspnoea) 9 days after hospital discharge and was readmitted with a diagnosis of COVID-19 pneumonia. The patient died 48 h after admission to the ICU.
We also performed a retrospective cohort evaluation of 337 patients undergoing surgery in our hospital in the months prior to the COVID-19 pandemic to verify the safety and quality of our protocol (between 1 December 2019 and 17 February 2020).
We compared the variable “Clavien Dindo Complications” from our series with a sample of cancer patients who had undergone similar cancer surgery in the months prior to the pandemic. The Chi-square value (P = .339) confirms that there were no differences between the 2 samples, despite the fact that the surgeries were performed in different periods (Table 4).
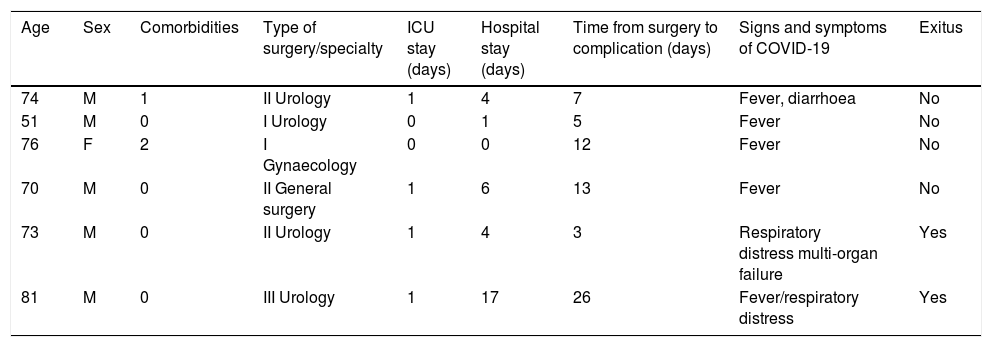
Follow-up and safetyThe mean hospital stay was 3.31 days (IQR: 2–4). The patients were followed up on an outpatient basis for an average of 10 days, with an additional follow-up visit 1 month after surgery. Six patients (1.80%) showed signs of COVID-19 infection (Table 5). Perioperative mortality was 2 patients (0.6%). Three (6.81%) out of 44 surgical suite staff involved in the protocol became infected with COVID-19.
Patients infected by COVID-19.
| Age | Sex | Comorbidities | Type of surgery/specialty | ICU stay (days) | Hospital stay (days) | Time from surgery to complication (days) | Signs and symptoms of COVID-19 | Exitus |
|---|---|---|---|---|---|---|---|---|
| 74 | M | 1 | II Urology | 1 | 4 | 7 | Fever, diarrhoea | No |
| 51 | M | 0 | I Urology | 0 | 1 | 5 | Fever | No |
| 76 | F | 2 | I Gynaecology | 0 | 0 | 12 | Fever | No |
| 70 | M | 0 | II General surgery | 1 | 6 | 13 | Fever | No |
| 73 | M | 0 | II Urology | 1 | 4 | 3 | Respiratory distress multi-organ failure | Yes |
| 81 | M | 0 | III Urology | 1 | 17 | 26 | Fever/respiratory distress | Yes |
F: female; ICU: intensive care unit; M: male.
Opinions have varied widely on cancer treatment during the COVID-19 pandemic. Most medical associations recommend the use of telemedicine, oral or subcutaneous administration of systemic treatments, and postponement of non-urgent treatment9. Cancer patients are a high risk group. Their immunosuppressive status and underlying disease makes them vulnerable to infection, and they are also at risk of serious complications when infected by COVID-1910. According to preliminary reports, between 44% and 53% of cancer patients present COVID-19-related complications, with a mortality rate of between 20%–28%.
The incidence of intrahospital COVID-19 infection among cancer patients is estimated to be as high as 28%–41%6,11,12.
These alarming data led to the suspension of cancer surgery in most countries, with medical associations and public health authorities around the world calling for these procedures to be prioritised strictly on the basis of curative intent. This prompted the United Kingdom’s National Health Service to establish 4 levels of priority: emergencies, urgent cases, elective surgery with the expectation of cure, and elective surgery that can be delayed for 10–12 weeks13. At that time, the Society of Surgical Oncology recommended postponing surgeries whenever possible and prioritising neoadjuvant therapy prior to surgery as a temporary measure14. The European Association of Urology published a clinical report that established 4 levels of priority: low, intermediate, high and emergency15, but recommended that decisions be made on a patient by patient basis.
In light of the high rate of mortality and complications previously reported, at the start of the pandemic we designed an anaesthesia-surgery protocol to identify patients infected by COVID-19 and isolate surgical patients both inside and outside the hospital as far as possible.
Early hospital discharge, with a mean hospital stay of 3.31 days, was a significant achievement considering the importance, at that time, of patients having as little contact as possible with the hospital environment. The availability of a highly trained surgical team was also key to the success of the protocol, as shown by the low (2.39%) rate of serious complications (Clavien-Dindo greater than III), length of ICU stay (1.06 days) and rate of ICU readmission (1.49%).
Our results are very similar to those obtained from a sample of 337 patients undergoing surgery between December 2019 and February 2020. Over that period, the rate of serious complications (Clavien-Dindo greater than III) was 2.07%, stay in the ICU was 1.31 days, and the rate of readmission to the ICU was 1.29%.
We believe that our “double detection” system, together with our surgical protocol, strict patient isolation, the structural modifications made to our hospital, and the use of small but highly qualified teams has played a fundamental role in avoiding infections and complications in our surgical patients.
Our study shows that surgeries performed during the COVID-19 pandemic can be performed with a reasonable incidence of complications and mortality (0.6%). However, surgery should only be indicated after a thorough risk-benefit analysis. Considering the constant exposure of surgical personnel at that stage of the pandemic, we believe that a 6.8% rate of infection among our staff, who developed only mild symptoms, is a highly positive result.
Our study has some limitationsFor example, preoperative PCR for COVID-19 was only performed in patients with compatible clinical or epidemiological risk factors and with suspicious radiological findings. RT-PCR was not performed in all patients due to the shortage of reagents in Spain at the start of the first wave (March 2020). To overcome this problem, under our protocol these reagents were only used in patients with suspected COVID-19 infection. There are now enough reagents in Spain to rule out COVID-19 infection in asymptomatic patients, so this variable has now been added to our protocol.
Another limitation is the impossibility of performing an autopsy on one of our non-survivors, as this procedures was banned at the time of the study.
We believe that our protocol has proven effective in the real world and could be useful in countries with limited access toCOVID-19 tests.
A future objective should be to measure the consequences of delaying cancer surgeries in patients with COVID-19 infection during this period, and whether this delay has clearly altered their prognosis.
Based on the largest series of surgical cancer patients during the first wave of the COVID-19 pandemic in Madrid (Spain), our results show that it is safe to perform surgery if strict isolation measures and good case detection protocols are followed. This means that the risk-benefit ratio must be calculated before postponing treatment. The combination of “double screening” and our surgical protocol have been effective in our setting. We believe that this surgical and screening protocol may be useful in countries with limited resources or limited access to COVID-19 blood tests.
Considering the highly likely scenario of further COVID-19 outbreaks this autumn and successive waves over the next 1–2 years, we believe that the results of our study are very important, and will further improve now that PCR can be performed in asymptomatic COVID-19 patients undergoing any surgery.
In conclusion, efforts must be made to rid hospitals of COVID-19 in order to perform non-deferrable surgeries in the current global health emergency, and in future pandemics.
Conflict of interestsThe authors have no conflict of interest to declare.
We would like to thank all the professionals who made this study possible: Yelo; Fernandez-Chereguini, M; Alonso S; Lista-Mateos, F; Ortega, G; Alonso, O; Conde A; Barberá, R; Delgado B; Prieto, I; Gonzalez-Moreno, S; Raboso, E; De Santiago, J; Nuñez-Mora C. Our thanks also go to all the nurses, nursing assistants, porters, cleaners, administrative staff and other staff members for their commendable work during this stage of the pandemic.
Please cite this article as: Galipienzo J, Otta-Oshiro RJ, Salvatierra D, Medrano C, López-Rojo I, Linero M. Manejo perioperatorio de cirugías oncológicas no diferibles durante la pandemia de covid-19 en Madrid, España. ¿Es seguro? Rev Esp Anestesiol Reanim. 2022;69:25–33.