COVID-19 became a threat to the public health system, compromising the health of the population. Patients with hip fractures, due to their age and comorbidity, were high-risk patients in this pandemic. The purpose of this study was to observe how the pandemic affected the management of hip fractures in elderly patients.
MethodsThis is a descriptive, retrospective study of all patients over the age of 65 diagnosed with a hip fracture that came to the emergency room of Vall d’Hebron University Hospital in the COVID-19 pandemic period, from the 11th of March to the 24th of April 2020. They were followed up during their hospital stay and 30 days after the fracture.
ResultsA total of 63 patients were included, 18 (28.6%) of whom had a positive RT-qPCR for COVID-19. Four could not be operated on due to the severity of the disease they presented with upon admission, dying a few days afterwards. Three of these patients had COVID-19. The 83.3% of the patients with positive RT-qPCR presented respiratory symptoms during their hospitalization. The length of hospital stays of patients with a positive RT-qPCR (18.25±8.99 days) was longer than that of patients that were RT-qPCR negative (10.9±4.52 days) (p=.01). In-hospital mortality in operated patients was 20% in patients with a positive RT-qPCR, compared with 2.3% in the group of patients who tested negative (p=.018). Mortality at 30 days was 40% in the group with positive RT-qPCR vs 6.8% in patients not infected by SARS-CoV-2 (p=.002).
ConclusionSARS-CoV-2 infection in elderly patients with hip fractures increases both the length of hospital stay, as well as in-hospital and 30-day mortality.
La COVID-19 se convirtió en una amenaza para el sistema de salud público, comprometiendo la salud de la población. Los pacientes con fractura de cadera, debido a su edad y comorbilidad, fueron pacientes de alto riesgo en esta pandemia. La finalidad de este estudio fue observar cómo afectó la pandemia al manejo de las fracturas de cadera del paciente anciano.
MétodosSe trata de un estudio descriptivo, retrospectivo de todos los pacientes mayores de 65 años diagnosticados de fractura de cadera que acudieron a urgencias del Hospital Universitario Vall d’Hebron en el periodo de pandemia COVID-19 comprendido entre el 11 de marzo y el 24 de abril de 2020. Fueron seguidos durante su ingreso hospitalario y a los 30 días de la fractura.
ResultadosSe incluyeron un total de 63 pacientes, 18 (28,6%) de los cuales tenían una RT-qPCR positiva para COVID-19. Cuatro no pudieron ser operados debido a la gravedad que presentaban al ingreso, falleciendo a los pocos días. Tres de estos pacientes tenían la COVID-19. El 83,3% de los pacientes con RT-qPCR positiva presentaron clínica respiratoria durante su hospitalización. La duración de la estancia hospitalaria de los pacientes con RT-qPCR positiva (18,25±8,99 días) fue mayor que los pacientes no COVID (10,9±4,52 días) (p=0,01). La mortalidad intrahospitalaria de los pacientes intervenidos fue del 20% en los pacientes con RT-qPCR positiva en comparación con el 2,3% del grupo de pacientes que testaron negativo (p=0,018). La mortalidad a los 30 días fue del 40% en el grupo con RT-qPCR positiva vs. el 6,8% de los pacientes no infectados por SARS-CoV-2 (p=0,002).
ConclusiónLa infección por SARS-CoV-2 en pacientes ancianos con fractura de cadera aumenta tanto el tiempo de ingreso hospitalario como la mortalidad intrahospitalaria y a los 30 días.
In December 2019, the city of Wuhan, capital of China's Hubei Province, became the centre of an outbreak of pneumonia of unknown cause. On 7 January 2020, Chinese scientists had isolated a new coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; formerly known as 2019-nCoV), which causes the disease that the World Health Organization later called coronavirus disease 2019 (COVID-19).1,2 On 11 March 2020, the World Health Organization declared the COVID-19 pandemic. The first Spanish case was diagnosed on January 31.3 On 14 March 2020, Spain declared a State of Alarm. COVID-19 became a threat to the public health system, compromising the health of the population, especially the most vulnerable.
Due to the exceptional situation produced by the pandemic, on 14 March scheduled surgery in our hospital was suspended and anaesthesiologists began to treat critically ill COVID-19 patients. Because of the exponential increase in cases with respiratory symptoms and patients needing critical care, the resuscitation and postanaesthesia care units (PACU) in the Orthopaedic Area of the Vall d’Hebron University Hospital were turned over to COVID-19 patients on 25 March. At the height of the pandemic, there were 178 mechanically ventilated patients admitted to COVID-19 critical care units in our hospital, 58 of which were cared for in the Orthopaedic Area. The PACU only returned to the postoperative care of non-COVID-19 patients on 20 April.
Around 1.6 million osteoporotic hip fractures occur annually worldwide.4 The 12-month mortality rate for these patients is estimated to be approximately 30%,5,6 while 30-day mortality is 7%–9%.6–8 Conservative treatment9 and a delay in surgery of more than 48h are associated with an increase in mortality.6,8,10 At the same time, due to their age and comorbidities, elderly patients with hip fracture have been classed as a vulnerable group during this pandemic.1 The first published scientific data from China reported high mortality among surgical patients,11 and conservative treatment was even recommended in proximal femur fractures.12
The aim of this study is to evaluate the impact of the COVID-19 pandemic on the perioperative management of patients aged over 65 years admitted for hip fracture.
Material and methodStudy design and participantsThis is an observational, retrospective, descriptive study of all patients aged over 65 years diagnosed with hip fracture who presented at the emergency department of the Vall d’Hebron University Hospital in the period between 11 March and 24 April 2020.
During the study period, the resuscitation unit and the PACU of the Orthopaedic Area had been turned over to the treatment of critical patients with COVID-19. In order to evaluate how this situation affected compliance with the recommendation to perform hip fracture surgery in elderly patients during the first 48h, we divided the patients into 3 stages, according to the day of their admission: Stage 1: prior to conversion to COVID units (from 11 to 24 March). Stage 2: during conversion to COVID units (25 to April 19 March). Stage 3: after reconversion of the PACU to non-COVID postoperative care (20–24 April).
The study adhered strictly to the ethical principles of biomedical research and was approved by the Clinical Research Ethics Committee of the Vall d’Hebron University Hospital, waiving the need for informed consent.
The clinical, demographic, laboratory data, type of treatment and radiological findings were extracted from each patient's electronic medical records using SAP software (SAP SE, Walldorf, Germany).
VariablesThe demographic variables were sex, age, address (private home, retirement home, or other institution) and history of contact with a patient diagnosed with COVID-19. The clinical variables reported were: type of femur fracture, symptoms compatible with COVID-19 on admission (heart rate, dyspnoea, cough, body temperature, oxygen saturation, oxygen therapy requirements, and chest X-ray on admission), prior ambulation, comorbidities, and American Society of Anesthesiologists (ASA) class. The Charlson comorbidity index was also calculated. The laboratory data correspond to tests performed on admission. The diagnosis of COVID-19 was determined by nasopharyngeal swab real-time reverse transcriptase polymerase chain reaction (RT-qPCR) test. The RT-qPCR test protocol in patients admitted to the hospital during the study period was modified as our knowledge of COVID-19 increased. Initially, RT-qPCR was only performed in patients who presented symptoms or chest radiograph compatible with COVID-19 and/or epidemiological criteria. Subsequently, as of 20 March, RT-qPCR was performed indiscriminately on all admitted patients. Regardless of the protocol followed, the RT-qPCR test was repeated if a patient presented symptoms suggestive of COVID-19 during hospitalization. Medical records were reviewed to determine whether the patient had presented respiratory symptoms (oxygen saturation less than 90%, dyspnoea) and temperature higher than 38°C during their hospital stay, and whether they presented any complications during admission. Surgical variables were type of surgical treatment and type of anaesthesia received. The date and destination at discharge, in-hospital death, and 30-day mortality were recorded.
Statistical analysisStatistical analysis was performed using the SPSS 22 statistical program (IBM Corp.). We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies.13
Continuous variables are presented as mean and standard deviation, ordinal variables as median and interquartile range, and categorical variables as number and percentage. Continuous variables were analysed using the Student's t test, categorical variables were analysed using the Chi-square test, and ordinal variables (ASA and Charlson comorbidity index) were analysed using the U-Mann–Whitney test.
ResultsBetween 11 March and 24 April, a total of 67 patients diagnosed with hip fracture were admitted to our hospital. RT-qPCR testing was not performed in 4 cases, so they were subsequently eliminated from the study, leaving a total of 63 patients for analysis. Of these, the RT-qPCR of 45 (71.4%) patients was negative and 18 (28.6%) obtained a positive result. Of the COVID-19 positive patients, 7 tested positive after 1 or more previous negative RT-qPCR results. An analysis of the prevalence of infection during the 3 aforementioned stages showed that in the first stage, 61.1% of patients admitted had a positive RT-qPCR, while in the second and third these percentages were 15.4% and a 16.7% respectively.
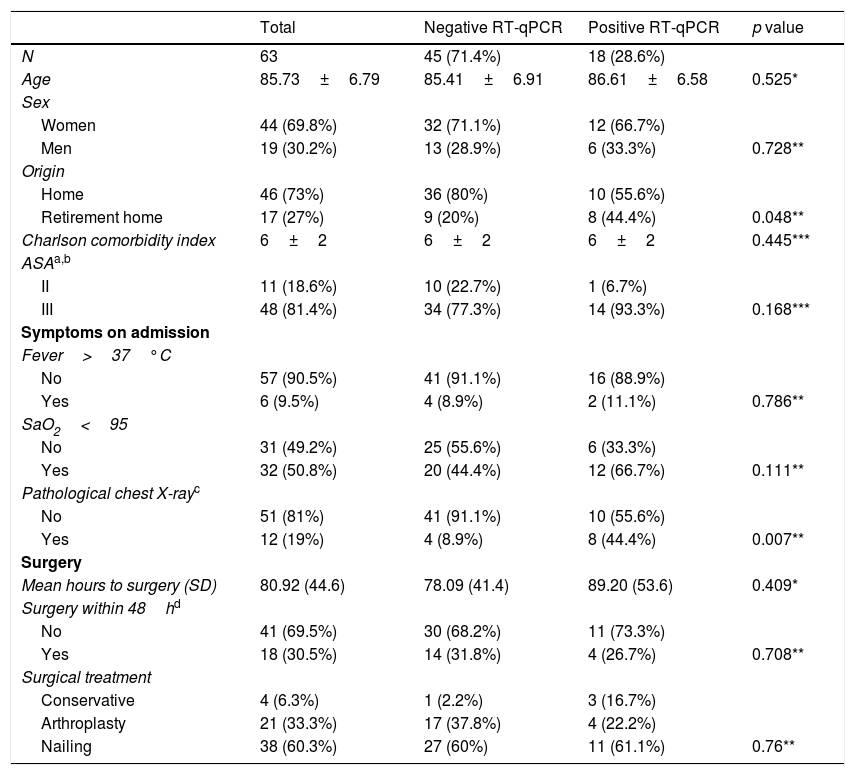
Table 1 shows a summary of the data from all patients included in the study. The variables are grouped by the total number of patients and by the result of the RT-qPCR.
Description of the sample and inferential statistics.
| Total | Negative RT-qPCR | Positive RT-qPCR | p value | |
|---|---|---|---|---|
| N | 63 | 45 (71.4%) | 18 (28.6%) | |
| Age | 85.73±6.79 | 85.41±6.91 | 86.61±6.58 | 0.525* |
| Sex | ||||
| Women | 44 (69.8%) | 32 (71.1%) | 12 (66.7%) | |
| Men | 19 (30.2%) | 13 (28.9%) | 6 (33.3%) | 0.728** |
| Origin | ||||
| Home | 46 (73%) | 36 (80%) | 10 (55.6%) | |
| Retirement home | 17 (27%) | 9 (20%) | 8 (44.4%) | 0.048** |
| Charlson comorbidity index | 6±2 | 6±2 | 6±2 | 0.445*** |
| ASAa,b | ||||
| II | 11 (18.6%) | 10 (22.7%) | 1 (6.7%) | |
| III | 48 (81.4%) | 34 (77.3%) | 14 (93.3%) | 0.168*** |
| Symptoms on admission | ||||
| Fever>37°C | ||||
| No | 57 (90.5%) | 41 (91.1%) | 16 (88.9%) | |
| Yes | 6 (9.5%) | 4 (8.9%) | 2 (11.1%) | 0.786** |
| SaO2<95 | ||||
| No | 31 (49.2%) | 25 (55.6%) | 6 (33.3%) | |
| Yes | 32 (50.8%) | 20 (44.4%) | 12 (66.7%) | 0.111** |
| Pathological chest X-rayc | ||||
| No | 51 (81%) | 41 (91.1%) | 10 (55.6%) | |
| Yes | 12 (19%) | 4 (8.9%) | 8 (44.4%) | 0.007** |
| Surgery | ||||
| Mean hours to surgery (SD) | 80.92 (44.6) | 78.09 (41.4) | 89.20 (53.6) | 0.409* |
| Surgery within 48hd | ||||
| No | 41 (69.5%) | 30 (68.2%) | 11 (73.3%) | |
| Yes | 18 (30.5%) | 14 (31.8%) | 4 (26.7%) | 0.708** |
| Surgical treatment | ||||
| Conservative | 4 (6.3%) | 1 (2.2%) | 3 (16.7%) | |
| Arthroplasty | 21 (33.3%) | 17 (37.8%) | 4 (22.2%) | |
| Nailing | 38 (60.3%) | 27 (60%) | 11 (61.1%) | 0.76** |
Mean age was 85.73±6.79 years, with a maximum of 100 years and a minimum of 70 years. Age did not differ significantly between groups. Most patients were women (69.8%). Less than half (44.4%) of all patients with positive RT-qPCR came from a retirement home compared to 20% of patients with negative RT-qPCR; this difference was statistically significant (p=0.048).
In total, 63.5% of patients had 2 or more comorbidities prior to admission. The median Charlson Comorbidity Index score was 6, with a maximum of 12 and a minimum of 3; there were no statistically significant difference between groups. To facilitate comparisons among groups, only the patient's prior medical history, not their current COVID-19 status, was factored in when determining their ASA class. Observing that 81.4% of patients undergoing surgery were ASA III, a statistically significant difference was not obtained between groups.
Of the 6 patients admitted with a temperature higher than or equal to 37°C, only 1 had a temperature higher than 38°C (38.4°C). This patient died 6 days after admission, before surgery could be performed. The remaining patients were discharged from the hospital without incident. The other patient with positive RT-qPCR who was admitted with a temperature of 37.2°C underwent surgery on the second day and was discharged 12 days after admission.
In the group with positive RT-qPCR, 44.4% of patients presented pathological chest X-ray (unilateral or bilateral infiltrate) on admission compared to 8.9% in the other group; this difference was statistically significant (p=0.007).
Of the 63 patients with a diagnosis of proximal femur fracture (Table 1), 4 could not undergo surgery due to their severity on admission, and died after a few days. Three of these patients had a positive RT-qPCR; the cause of death was severe SARS-CoV-2 pneumonia. The other patient was negative on RT-qPCR, but presented highly advanced dementia and a Charlson comorbidity index of 10. This patient died due to worsening of renal failure with progressive worsening of vital functions.
In total, 60.3% of patients underwent intramedullary nailing of the proximal femur and 33.3% underwent hip hemiarthroplasty. All surgical procedures were performed under spinal anaesthesia. The anaesthetic used in all cases was bupivacaine, administering doses that ranged from 8 to 10mg with 10μg fentanyl. Femoral and femorocutaneous nerve blocks were performed in 73.3% of patients with positive RT-qPCR and in 61.7% with negative RT-qPCR (p=0.403). In the COVID-19 patient group, surgery was delayed by a mean of 89.20 (53.6) hours from admission, while in the non-COVID-19 group mean delay was 78.09 (41.4); these differences were not statistically significant (p=0.409). After analysing the different stages, we observed that in stage 1 surgery was delayed by 65.31 (46.5) hours, in stage 2 by 89.76 (45.2) hours, and in stage 3 by 68 (17.3) hours. Our operational capacity decreased to 30.5% during the first 48h for all patients with proximal femur fracture, with no statistically significant differences between groups.
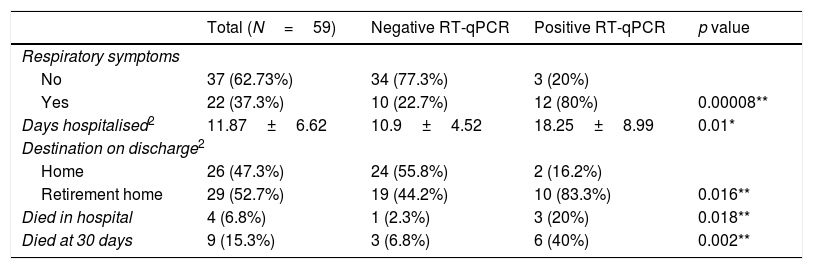
Table 2 analyses the evolution of the 59 patients who underwent surgery; 12 (80%) patients with positive RT-qPCR presented respiratory symptoms compared to 10 (22.7%) patients with negative RT-qPCR (p=0.00008). In the group with positive RT-qPCR, the hospital length of stay was almost twice that of the non-COVID-19 group: 18.25±8.99 vs. 10.9±4.52 (p=0.01). In-hospital mortality was 20% in patients with positive RT-qPCR compared to 2.3% in uninfected patients (p=0.018). After 30-day follow-up, a further 6 (40%) patients in the group with positive RT-qPCR died vs. 3 (6.8%) in the non-COVID-19 group (p=0.002). In-hospital causes of death in the 3 patients with positive RT-qPCR who received surgical treatment were SARS-CoV-2 pneumonia; one of them presented concomitant acute renal failure. The cause of in-hospital death of the patient with negative RT-qPCR who underwent surgery was decompensation of his congestive heart failure.
Evolution of patients undergoing surgery.
| Total (N=59) | Negative RT-qPCR | Positive RT-qPCR | p value | |
|---|---|---|---|---|
| Respiratory symptoms | ||||
| No | 37 (62.73%) | 34 (77.3%) | 3 (20%) | |
| Yes | 22 (37.3%) | 10 (22.7%) | 12 (80%) | 0.00008** |
| Days hospitalised2 | 11.87±6.62 | 10.9±4.52 | 18.25±8.99 | 0.01* |
| Destination on discharge2 | ||||
| Home | 26 (47.3%) | 24 (55.8%) | 2 (16.2%) | |
| Retirement home | 29 (52.7%) | 19 (44.2%) | 10 (83.3%) | 0.016** |
| Died in hospital | 4 (6.8%) | 1 (2.3%) | 3 (20%) | 0.018** |
| Died at 30 days | 9 (15.3%) | 3 (6.8%) | 6 (40%) | 0.002** |
a Non-survivors were not included in the calculation.
Three (6.5%) of the 46 patients who lived at home died; 37% of patients who lived at home were discharged to a nursing home. Of the 17 patients who lived in retirement homes, 5 (29.4%) died.
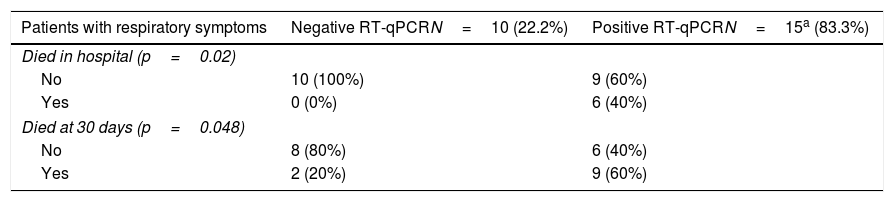
Of the 63 patients who were admitted, 25 (39.7%) developed respiratory symptoms during their hospital stay. In Table 3, these patients are classified according to the result of the RT-qPCR and the number of deaths. None of the patients with negative RT-qPCR and respiratory symptoms died during their hospital stay vs. 6 (40%) patients with positive RT-qPCR (p=0.02). After 30-day follow-up, a further 3 patients with positive RT-qPCR died, resulting in a total of 9 deaths. In the group with negative RT-qPCR, 2 patients died. Our results show a higher mortality rate in patients with respiratory symptoms and positive RT-qPCR compared with patients with only respiratory symptoms.
Mortality among patients with respiratory symptoms according to the result of the RT-qPCR test.
| Patients with respiratory symptoms | Negative RT-qPCRN=10 (22.2%) | Positive RT-qPCRN=15a (83.3%) |
|---|---|---|
| Died in hospital (p=0.02) | ||
| No | 10 (100%) | 9 (60%) |
| Yes | 0 (0%) | 6 (40%) |
| Died at 30 days (p=0.048) | ||
| No | 8 (80%) | 6 (40%) |
| Yes | 2 (20%) | 9 (60%) |
Shows in-hospital and 30-day mortality of the 25 patients who presented respiratory symptoms according to the PCR.
The exceptional situation produced by the COVID-19 pandemic put considerable pressure on the healthcare system and stretched the capacity of Spanish hospitals to the limit. The Vall d’Hebron University Hospital is divided into 3 areas, each one located in a separate building: the General Area, the Maternity Area and the Orthopaedics Area. Patients with COVID-19 were initially admitted to the General Area and later to the Orthopaedic Area. The anaesthesiology service of our hospital had to adapt to the situation imposed by the COVID-19 pandemic. Scheduled surgery was postponed during stage 1, and only non-deferrable interventions continued to be performed in the Orthopaedic Area (fractures, oncological surgery, sepsis and burns). Some anaesthesiologists from the Orthopaedic Area were transferred to the COVID-19 groups in the General Area. In stage 2, the remaining anaesthesiologists from the Orthopaedic Area were divided into 3 teams that rotated in 3-day shifts to care for critical COVID-19 patients admitted to the unit. One member of the team was assigned to multiple trauma patients and other emergency surgeries, and 2 anaesthesiologists were assigned every day of the week to surgeries in patients with fractures and patients in the burn unit. During this stage, since there was no PACU, the patients received post-anaesthesia care in the operating room. Patients requiring longer postoperative monitoring were admitted to the burn unit, which had been adapted to non-COVID-19 critical patients, those with positive RT-qPCR were admitted to COVID-19 critical care units. In stage 3, the reconversion of the PACU and the return of part of the anaesthesia staff facilitated patient care. However, hip fracture patients diagnosed with COVID-19 continued their post-anaesthesia recovery in the operating room.
In this study, the model hip fracture patient is a woman (69.9%) with a mean age of around 85 years, ASA III (82.5%) who lives at home (73%). Our demographics are very similar to those found in the National Hip Fracture Registry.14
From time COVID-19 was first declared a pandemic by the World Health Organization up to 20 March that year, only patients who met epidemiological criteria (having been in a risk area or in contact with a patient diagnosed with COVID-19), presented respiratory symptoms, or an X-ray suggestive of COVID-19 infection underwent RT-qPCR testing. This is why 4 of the 67 patients who were admitted during the study period were not tested for COVID-19 during their hospital stay, and were excluded from the study. After this date, RT-qPCR testing was performed in all patients admitted because 3 patients who had been admitted without clinical or epidemiological criteria for RT-qPCR presented respiratory symptoms after a few days. A subsequent RT-qPCR test showed they were positive for COVID-19.
Up 20 March, patients who underwent RT-qPCR under the aforementioned criteria were admitted to isolation rooms until the result was obtained. However, patients not tested for COVID-19 on admission were sent to non-COVID-19 wards, thereby risking the spread of the disease to both patients admitted for other reasons and to healthcare workers if they were asymptomatic or later developed symptoms. The RT-qPCR test may be less efficient in detecting infections early due to the low viral load, and the incubation period of the virus can be highly variable.15 Therefore, a patient testing positive after testing negative during the first week of hospitalization was probably due to a false negative. However, if the patient tested positive more than 7 days after hospitalisation, the source was probably nosocomial infection. In our study, 4 patients tested positive during the first week of hospitalization and 3 patients tested positive more than 7 days after admission.
Chest X-ray on admission was pathological in 8 of the 18 patients with positive RT-qPCR – a low sensitivity of 44.4%. For this reason, we believe that chest X-ray has little value as a screening method for SARS-CoV-2 RT-qPCR testing. Initial chest X-ray sensitivity for detecting COVID-19-induced pneumonia is also low.16 Only 8 of the 15 COVID-19 patients who presented respiratory symptoms during hospitalization had a pathological X-ray at the time of admission. Computerized axial tomography, unlike chest radiography, is sensitive enough to reveal pathological findings even before symptoms appear, and is diagnostic in patients with initial false negatives in RT-qPCR testing.16
Analysing mortality among patients undergoing surgery for hip fracture showed that in-hospital mortality among patients with negative RT-qPCR was 2.3%, the same proportion found in the National Registry of Hip Fractures.14 Among patients with positive RT-qPCR, however, mortality was 20%, that is, 8.7 times higher than in non-COVID-19 patients. Mortality at 30 days in the group with negative RT-qPCR was 6.8%, a rate very similar to that reported in other studies.6–8,14 However, 30-day mortality in COVID-19 patients was 40% – 5.9 times higher. Chlebeck et al.9 compared mortality in patients with proximal femur fracture according to whether they were treated surgically or not. They observed a 28.6% rate of in-hospital mortality in non-operated patients, a 63.6% rate at 30 days, and an 84.4% rate at 1 year. As our mortality rates, like those of other authors,17,18 are lower, we believe it is appropriate for them to undergo surgery as soon as the infection is clinically stable.
Hospital length of stay in patients with negative RT-qPCR was 10.9±4.52 days, similar to that reported in the National Registry of Hip Fractures.14 In the group of patients with positive qPCR-RT, however, mean hospital stay was almost twice as long (18.25±8.99 days). This was only to be expected, since they were not discharged until their respiratory symptoms improved and the RT-qPCR was negative.
Table 3 shows that 10 (22.2%) patients with negative RT-qPCR presented respiratory symptoms. This is one of the most frequent complications in this type of pathology.19,20 None of these 10 patients died in hospital, but 2 died within 30 days. This complication increases to 83.3% (15 of 18 patients) in patients with COVID-19, and mortality is also higher.
The National Registry of Hip Fractures14 reports a mean delay in surgery of 75.7 (63.6) hours, while in our cohort surgery delay was 80.92 (44.6) hours on average for all patients. When this average surgery delay was analysed by stage, we observed that stages 1 and 3 remained below the National Registry of Hip Fractures,14 with a delay of 65.31 (46.5) and 68 (17.3), respectively. However, delays increased significantly to a mean of 89.76 (45.2) hours when both our resuscitation units were occupied by COVID-19 patients. In 2019, 87.88% of patients in our hospital with proximal femur fracture underwent surgery within the first 48h of admission. During the study period, our ability to operate within the first 48h was reduced to 30.5% for all patients. This is probably due to several factors: the initial confusion caused by the pandemic; a positive RT-qPCR rate of 61.1% in stage 1; uncertainty surrounding the prognosis of these patients, which, according to the literature available at that time12 was very poor; and more importantly, most of our staff were assigned to the care of COVID-19 patients. We gradually modified our action protocol and tried to operate as soon as possible, only delaying surgery in patients with comorbidities that would have led to postponement even before the pandemic (such as severe respiratory failure). Authors such as Catellani et al.21 report that surgery in patients with COVID-19 may contribute to their overall stability, mobilisation, and may improve respiratory mechanics. In our series, we did not find that delaying surgery worsened prognosis, particularly in patients with negative RT-qPCR, although this is probably due to the small number of patients.
This study has several limitations: non-randomized, small sample size, and retrospective data analysis. This latter limitation has led to a lack of consistency in our data and in the analytical and blood gas follow-up in our patients. Nevertheless, we believe it is interesting to highlight the importance of operating on patients with a proximal femur fracture with or without a diagnosis of COVID-19 as soon as possible, once the patient is clinically stable.
The results of our study show that, despite the high rate of mortality in patients with hip fracture and COVID-19, the usual surgical treatment guidelines should be followed in this group of patients. Delay, or even suspension, of surgery in patients with COVID-19 would only be justified if they present high fever, severe respiratory failure or haemodynamic alterations.17.
- •
Eighteen (28.6%) of the 63 patients studied had positive RT-qPCR for COVID-19.
- •
In the first few days following the declaration of the state of alarm, 61.1% of hip fracture patients at the Vall d'Hebron University Hospital tested positive for COVID-19.
- •
The hospital length of stay was longer in patients with positive RT-qPCR (18.25±8.99 days) than non-COVID patients (10.9±4.52 days) (p=0.01).
- •
In-hospital mortality was 20% in patients with positive RT-qPCR compared to 2.3% in uninfected patients (p=0.018).
- •
Thirty-day mortality of patients undergoing surgery was 40% in the group with positive RT-qPCR vs. 6.8% in patients not infected by SARS-CoV-2 (p=0.002).
The authors have no conflict of interest to declare.
Please cite this article as: Biarnés-Suñé A, Solà-Enríquez B, González Posada MÁ, Teixidor-Serra J, García-Sánchez Y, Manrique Muñóz S. Impacto de la pandemia COVID-19 en la mortalidad del paciente anciano con fractura de cadera. Rev Esp Anestesiol Reanim. 2021;68:65–72.