Patients with SARS-CoV-2 infection may present cardiovascular involvement including myocarditis, arrhythmias and QT interval prolongation. Our objective was to evaluate the impact of COVID-19 and its treatment on ventricular repolarization and development of arrhythmias in critically ill patients.
MethodsRetrospective cohort study of critically ill COVID-19 patients during a 3-month period in whom at least one ECG was available. Relevant clinical data and specific treatment administered for COVID-19 were recorded. Prolonged QTc was considered prolonged when it measured ≥ 460 ms in women and ≥450 ms in men. The incidence and type of arrhythmias during the same period were recorded.
ResultsA total of 77 patients with a mean age of 62 ± 13 years, 20 women and 57 men, were evaluated. Sixty percent of the patients were hypertensive, 52% had a BMI > 30, and 70% developed acute renal failure during admission. Some 56% of the patients presented QTc prolongation. Forty-four percent presented some type of arrhythmia during their stay in the ICU, 21% of which were atrial arrhythmias. Overall mortality was 53%, with no differences between patients with or without prolonged QTc.
ConclusionsIn our series, a high proportion of critical patients with COVID-19 presented prolonged QTc and arrhythmias. The factors involved have been related to the elevation of cardiac biomarkers, the myocardial involvement of the virus and concomitant medication received in the ICU.
Los pacientes con infección por SARS-CoV-2 pueden presentar afectación cardiovascular incluyendo miocarditis, arritmias y prolongación del intervalo QT. Nuestro objetivo fue evaluar el impacto del COVID-19 y su tratamiento en la repolarización ventricular y desarrollo de arritmias en pacientes críticos.
Material y métodosEstudio de cohortes retrospectivo de pacientes críticos con infección confirmada por SARS-CoV-2 durante un periodo de 3 meses. Se registraron datos clínicos relevantes y tratamiento específico administrado para el COVID-19. Se consideró QTc prolongado cuando medía ≥460 ms en mujeres y ≥450 ms en hombres. Se registró la incidencia y tipo de arritmias durante el mismo periodo.
ResultadosSe evaluaron 77 pacientes con una edad media de 62 ± 13 años, 20 mujeres y 57 hombres. Un 60% de los pacientes era hipertenso, un 52% presentaban un IMC > 30, y el 70% desarrollaron fracaso renal agudo durante el ingreso. Un 56% de los pacientes presentó prolongación del QTc. El 44% presentaron algún tipo de arritmia durante su estancia en la UCI, siendo en un 21% arritmias auriculares. La mortalidad global fue del 53%, sin diferencias entre los pacientes con o sin QTc prolongado.
ConclusionesEn nuestra serie, una elevada proporción de pacientes críticos con COVID-19 han presentado QTc prolongado y arritmias. Los factores implicados se han relacionado con la elevación de biomarcadores cardiacos, la propia afectación miocárdica del virus y a la medicación concomitante recibida en la UCI.
Cardiovascular involvement in patients with SARS-CoV-2 infection is one of the complications associated with coronavirus disease 2019 (COVID-19).1–4
Myocardial involvement may be related to the disease itself, with specific treatments for COVID-19 infection or the presence of previous cardiovascular pathology. Treatments for COVID-19 infection such as hydroxychloroquine, azithromycin, lopinavir/ritonavir, widely used during the early phases of the pandemic, have been associated with an increased risk of QT prolongation. Likewise, the association of COVID-19 with the appearance of cardiac arrhythmias has been described, these being more prevalent in patients admitted to intensive care units (ICU).5,6 In critically ill patients, there are additional factors such as electrolyte alterations, sepsis and the administration of concomitant drugs with the capacity to prolong the QT interval.7,8 All of these circumstances can alter cardiac electrophysiology, favour prolongation of the QT interval and facilitate the appearance of arrhythmias. The objective of the present study was to evaluate the impact of COVID-19 disease and its treatment on ventricular repolarisation, evaluated by measuring the QTc interval, and on the incidence of arrhythmias in critically ill patients during the first phase of the COVID pandemic.
Patients and methodsRetrospective cohort study of adult patients with a diagnosis of COVID-19 admitted to critical care units from March 9 to May 1, 2020. The study was approved by the ethics committee on May 7, 2020 (minutes 13/2020) and registered at ClinicalTrials.gov (NCT04422535). Given the nature of the study, the ethics committee waived the need to obtain informed consent from the patients.
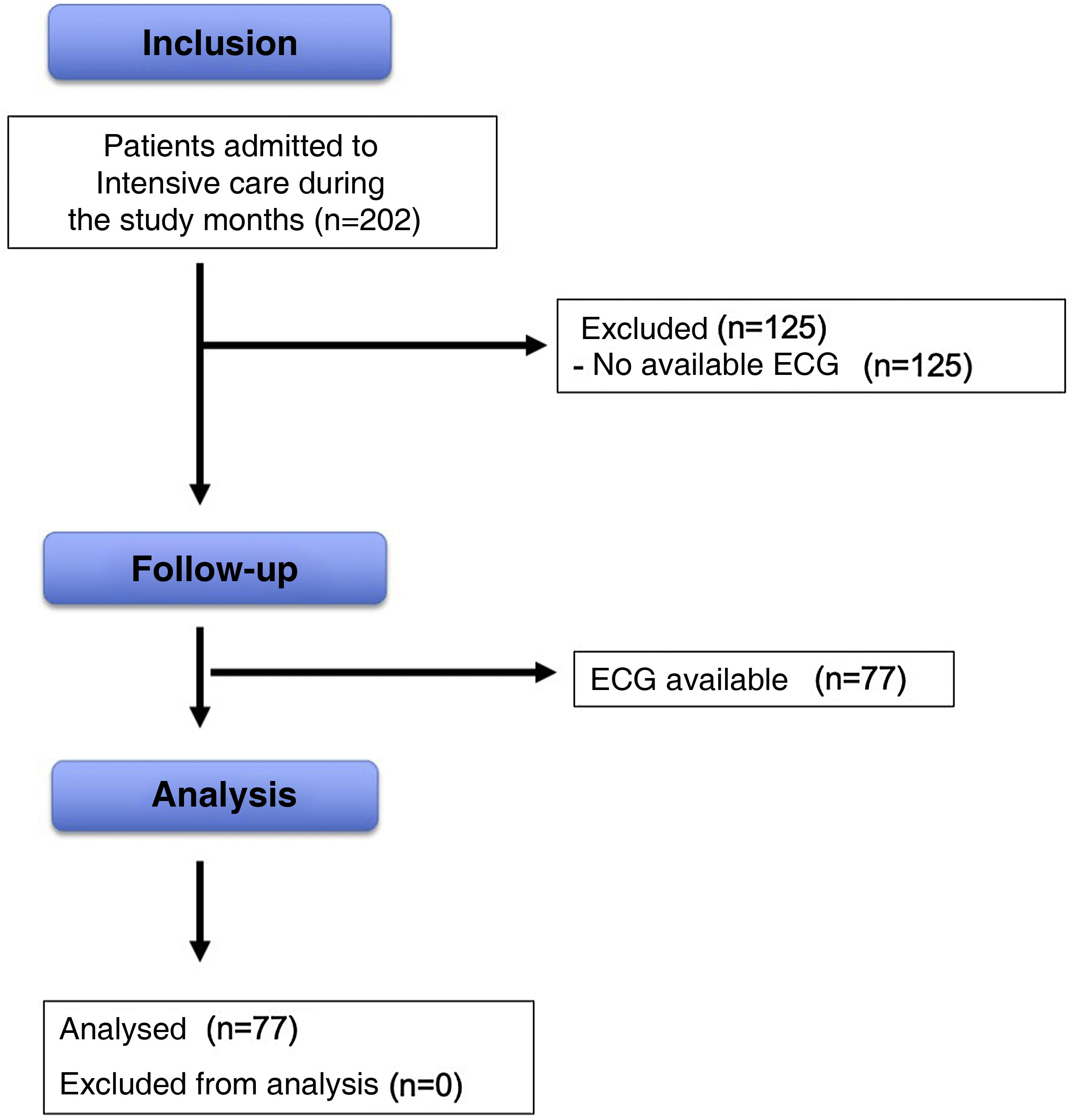
The inclusion criteria were adult patients admitted to the ICU over 18 years of age and diagnosed with COVID-19, confirmed by the RT-PCR (reverse transcriptase polymerase chain reaction) technique of nasopharyngeal samples, sputum or bronchoalveolar lavage. All patients with ECG recording available on paper were analysed. Fig. 1 describes the patient flow. The ECGs were collected individually and stored anonymised for subsequent analysis.
Variables analysedDemographic parameters, clinical evolution, analytical profile, including cardiac biomarkers, treatment instituted, complications, renal failure, potential factors associated with QT prolongation, arrhythmias during admission and mortality were recorded. Data were collected from the patients' electronic medical records.
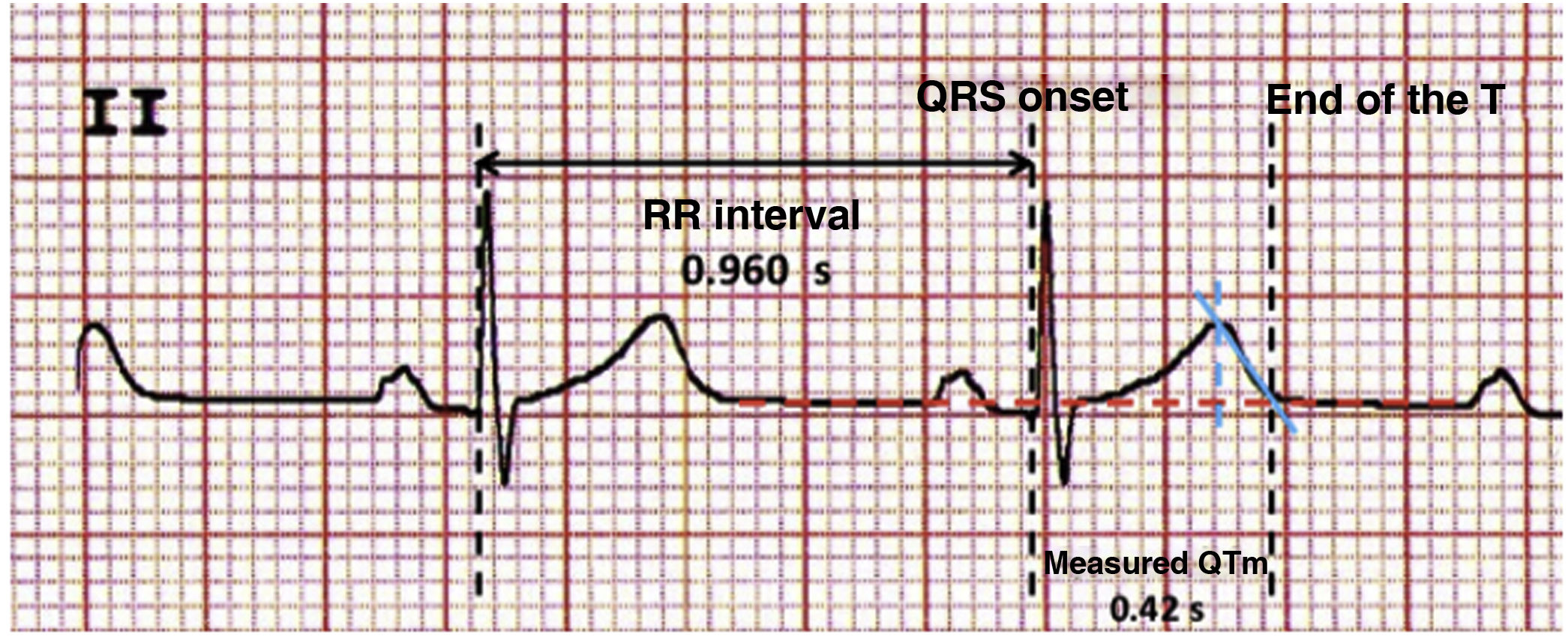
Electrocardiographic parameters and methodology for measuring the QT intervalFollowing the recommendations of the scientific societies of cardiology, the measurement of the QT interval was performed on the available 12-lead ECG, selecting leads II and V5 or V6 in which it best showed the end of the T wave.9,10
The QT interval was measured from the beginning of ventricular myocardial activation to the end of its repolarisation, represented by the beginning of the QRS and the end of the T wave (Fig. 2).
To determine the end of the T wave, a line was drawn from its vertex (dashed blue line) following the slope of its descending inscription (solid blue line) to where it intersects the baseline (red dotted line). The average QT value of 3 cardiac cycles (beats) was considered.
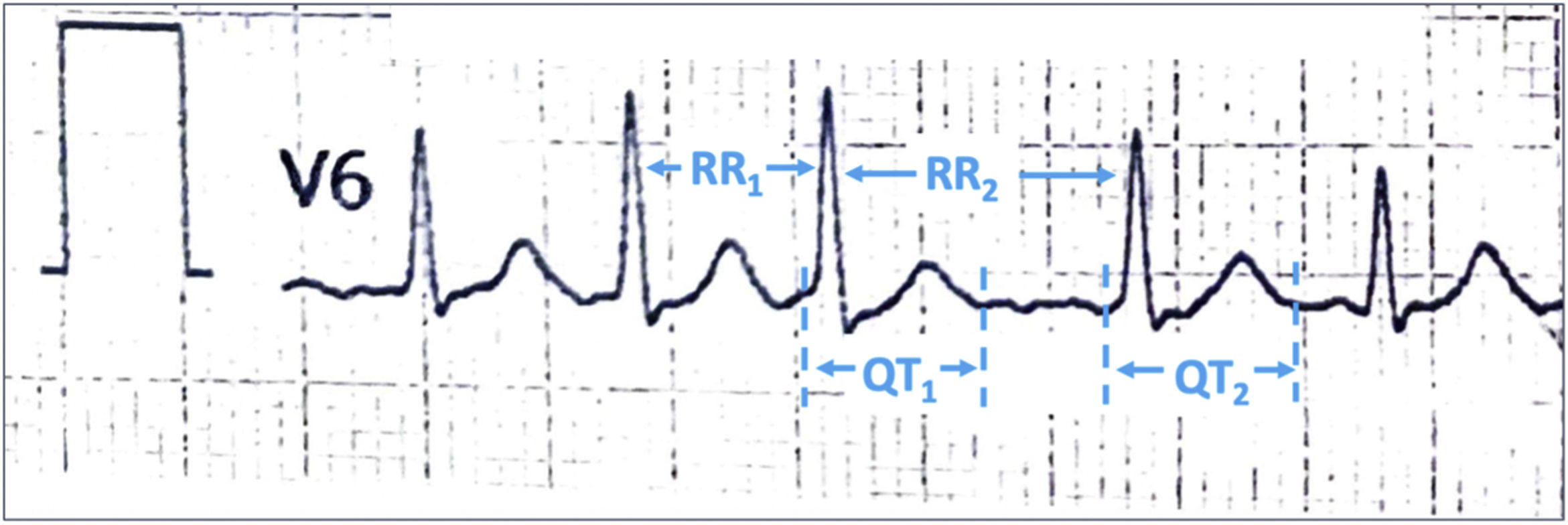
In cases of atrial fibrillation (AF), the measurement was performed in the QT intervals after the shortest and longest R-R intervals and each was divided by the square root of the preceding R-R interval (Bazett's formula). The average of these intervals was used as the corrected QT interval (Fig. 3).
The Bazett’s formula (QT corrected [QTc] = QT/√ RR) was used to determine the corrected QT intervals. A QTc length was considered when it was greater than ≥460 ms in women and ≥450 ms in men.11 The increase in the QTc interval was analysed in patients with two ECG records available.
ArrhythmiasThe presence of arrhythmias was identified if patients documented: AF, supraventricular tachycardia (SVT), non-sustained ventricular tachycardia, monomorphic or polymorphic ventricular tachycardia, ventricular fibrillation (VF) or sinus bradycardia (heart rate <50 bpm).
Statistical analysisThe normality of the continuous variables was previously checked using the Kolmogorov-Smirnov test. Continuous variables with normal distribution were compared using the Student’s t test for independent data or for paired data when necessary. The Mann–Whitney U test was used for independent data or the Wilcoxon test for paired data if the distribution was not normal. Categorical variables were compared using the Chi-square test and Fisher's test. Data are presented as mean ± standard deviation, median and interquartile range or numbers and percentiles.
ResultsOf a total of 202 patients admitted to the ICU during the study period, the electrocardiographic records of 77 patients could be analysed. The median (IQR) length of stay on the ward before ICU admission was 2 days (1–4). Ninety-seven per cent of patients required invasive mechanical ventilation.
The demographic and clinical data are reflected in Table 1. The data of patients who presented significant prolongation of the QT interval and those who did not present it are shown differently.
Demographic and clinical characteristics of patients with QTc interval ≥450 ms (men) and 460 ms (women) and QTc ≤450 (men) and 460 ms (women).
| QTc ≥450/460 N = 43 | QTc <450/460 N = 34 | P | |
|---|---|---|---|
| QTc (ms)(mean ± DS) | 486 ± 29 | 426 ± 25 | .001 |
| Age (years) (mean ± DS) | 63 ± 12 | 61 ± 14 | .47 |
| Weight (Kg) (mean ± DS) | 85 ± 21 | 84 ± 15 | .69 |
| Height (m) (mean ± DS) | 165 ± 28 | 164 ± 8 | .95 |
| Sex, male, n (%) | 37 (48) | 20 (26) | .007 |
| High blood pressure, n (%) | 24 (44) | 22(35) | .42 |
| Diabetes, n (%) | 7 (9) | 4 (5) | .57 |
| Obesity, BMI > 30 kg/m2, n (%) | 22 (29) | 18 (23) | .87 |
| Chronic kidney failure, n (%) | 7 (9) | 4 (5) | .57 |
| Heart disease, n (%) | 8(10) | 7(9) | .82 |
| COPD, n (%) | 8(10) | 7(9) | .82 |
| Hepatopathy, n (%) | 6 (8) | 1(1) | .09 |
| ACEI/ARAII | 17(22) | 17 (229 | .44 |
| QT prolonging COVID medications, n (%) | 43 (56) | 32 (44) | .10 |
| Lopinavir/ritonavir + hydroxychloroquine, n (%) | 40 (52) | 32 (42) | .80 |
| Azithromycin + hydroxychloroquine, n (%) | 20 (26) | 13 (17) | .46 |
| Lopinavir/ritonavir + hydroxychloroquine + azithromycin | 19 (25) | 13 (17) | .38 |
| Azithromycin + Lopinavir/ritonavir, n (%) | 1 (1,3) | 0 | .38 |
| Potassium (mEq/L)a (mean ± DS) | 4,03 ± .87 | 4,09 ± .79 | .74 |
| Ionic calcium (mmol/L)a (mean ± DS) | 1,15 ± .08 | 1,14 ± .11 | .50 |
| Magnesium (mg/dl)a (mean ± DS) | 2,21 ± .55 | 2,30 ± .48 | .45 |
| Creatinine upon admission mg/dl(mean ± DS) | .92 ± .23 | .91 ±.30 | .90 |
| Peak creatinine mg/dl(mean ± DS) | 1,60 (1,04−3,46) | 1,93 (1,2−3,11) | .84 |
| Acute kidney failure, n (%) | 29 (38) | 25(32) | .56 |
| AKI 1 n (%) | 11 (14) | 6 (8) | .50 |
| AKI 2 n (%) | 6 (8) | 9 (11) | |
| AKI 3 n (%) | 12 (16) | 10 (13) | |
| NT Pro-BNP, pg/mL (maximum concentration)(median, IQR) | 2.796 (973−7.666) | 2.973 (796−4836) | .38 |
| NT Pro-BNP > 5.000 pg/mL, n(%) (median and IQR) | 16 (21) | 5 (6) | .03 |
| Maximum Troponin T (ng/dL) (median, IQR) | 51 (6,4−126) | 11 (4−46) | .076 |
| Troponin >50 ng/dL, n (%) | 18 (23) | 6 (8) | .01 |
| Days of admission to the ICU (median, IQR) | 29 (12−38) | 25 (13−37) | .35 |
| Death in ICU, n (%) | 24 (31) | 17 (22) | .61 |
ACEI, angiotensin-converting enzyme inhibitor; ARA II, angiotensin II receptor antagonist; AKI, Classification of renal failure according to the KDIGO11 guidelines. AKI 1, (baseline Cr increase × 1.5−1.9); AKI 2, (baseline Cr increase × 2–2.9); AKI 3, (basal Cr increase × 3). The percentages have been made based on the total number of patients evaluated; BMI, body mass index.
56% of patients presented prolongation of the QTc interval (≥460 ms in women and ≥450 ms in men). Fifteen point six per cent of patients had a QTc greater than ≥500 ms. The percentage of men with prolonged QTc was higher than that of women: 65% vs. 30%, p = .007. There was no relationship between a history of HTN, obesity, chronic renal failure (CKD), diabetes or structural heart disease and the presence of prolonged QTc.
Ninety-nine per cent of patients were being treated with one of the COVID-19 treatment drugs with QT interval prolonging effects: hydroxychloroquine, azithromycin or lopinavir/ritonavir. This treatment had been instituted an average of 2.8 ± 3.2 days before the recording of the ECGs. Fifty-four point five per cent of the patients were treated with 2 drugs and 42% with three drugs. The most common two-drug combination was hydroxychloroquine plus lopinavir/ritonavir (Table 1). Patients on three drugs had longer QTc values than patients on two drugs, 451 ± 42 ms vs. 435 ± 40 ms, p = .08.
There were no significant differences in demographic and clinical parameters, COVID-19 treatment drugs, analytical patterns of ions, potassium, ionic calcium, magnesium, or in the incidence of acute kidney injury (AKI) in patients with or without interval prolongation QTc (Table 1).
In relation to cardiac biomarkers, troponin T levels were higher in the group that developed prolongation of the QTc interval, as well as the percentage of patients with troponin T levels above 50 ng/dL, 23% vs. 8%, p = .01. Regarding NT-proBNP, no differences were observed in absolute values between patients with or without prolonged QTc. However, there was a higher percentage of patients in the upper tertile (NT-proBNP ≥ 4,873 pg/mL) in the group of patients with prolonged QTc: 23% vs. 9%, at the limit of statistical significance, p = .06.
Changes in QTc intervalChanges in the QTC interval were analysed in cases in which 2 ECGs were available (39 patients) and it was observed that 38% had prolonged QTc in the first ECG and in the second ECG this percentage was 26%. Mean increase in QTc was 21 ± 57 ms, 95% CI (2.45–39.28). Twelve patients (15.58%) had an increase of more than 60 ms in the QTc interval during their admission. Overall, 25% of patients had a QTc greater than ≥500 ms or an increase in QTc ≥ 60 ms.
ArrhythmiasTable 2 shows the results of the arrhythmias that the patients presented during their stay in the ICU. Some type of arrhythmia developed in a total of 34 (44.2%) patients, the most common being AF. Within the group of patients with arrhythmias, 5 (6.5%) had a known history of rhythm disorders before admission. There was no relationship between the appearance of arrhythmias with previous diseases, nor with the values of the maximum QTc interval achieved. Patients who developed arrhythmias had higher NT-proBNP levels: median (IQR): 4,610 pg/mL (1,608–6,799) vs. 1,486 (618–4,869), p = 0.007. There were no differences in troponin T levels between patients who developed arrhythmias versus those who did not. Survival in patients who presented arrhythmias was 41.2%.
Frequency and type of arrhythmias in critically ill COVID-19 patients.
| Arrhythmias, n (%) | 34 (44.2) |
| Sinus bradycardia, n (%) | 7 (9) |
| Atrial fibrillation/Atrial flutter, n (%) | 16 (21) |
| Supraventricular tachycardia, n (%) | 7 (9) |
| Ventricular extrasystole, n (%) | 2 (2.6) |
| Non-sustained ventricular tachycardia, n (%) | 1 (1.3) |
| Torsade of points, n (%) | 1 (1.3) |
Percentages have been made based on the total number of patients evaluated.
A male patient presented a “torsade de pointes” (TdP) ventricular arrhythmia type, after an episode of bradycardia and hypotension. When analysing the ECG recordings, an increase in the QTc of 70 ms was found from the baseline ECG to the ECG prior to the arrhythmia, with the QTc value that preceded the arrhythmia episode being 450 ms. The patient had received treatment with hydroxychloroquine, azithromycin, and lopinavir/ritonavir.
MortalityOverall mortality during ICU admission was 53%. 67% of patients who developed AKI died in the ICU compared to 22% of those who did not, p = .001. Patients who developed AKI had higher NT-proBNP levels than those who did not develop AKI, median (IQR): 4,066 pg/mL (1,161–6,998) vs. 1,249 (570–3,968), p = .01. There was no association between the presence of prolonged QTc or arrhythmias with mortality.
DiscussionThe main findings of this study were: first, that a high percentage of COVID-19 patients admitted to the ICU had prolonged QTc; second, that QTc prolongation was related to elevated troponin T levels; third, that QTc prolongation occurred in a greater proportion in men; fourth, that COVID19-critical patients had a high incidence of arrhythmias during their stay in the ICU and finally that patients with arrhythmias had higher levels of NT-proBNP.
A study carried out in 40 critically ill COVID-19 patients showed that 36% presented prolongation of the QTc interval, which the authors defined as a QTc greater than ≥500 ms or an increase in QTc ≥60 ms after treatment with azithromycin plus hydroxychloroquine.12 These figures are higher than ours, which were 25% following the same value and QTc increase criteria defined in said study. Likewise, the proportion of patients who received azithromycin plus hydroxychloroquine was similar, 45% vs. 43% in our study. Unlike our series, the authors did not report arrhythmias or any TdP episodes. One reason that may explain these differences is that, in the aforementioned study, treatment with these drugs was suspended in 42.5% of the patients when it was detected that said limits in the QTc interval had been reached. However, in our series, the limits of withdrawal of these drugs due to prolongation of the QTc interval are not reflected in the clinical history data.
Mercuro et al. evaluated the impact of COVID treatment drugs (hydroxychloroquine with/without azithromycin) on the QTc interval in 90 patients.13 The study showed that 11% of the patients presented an increase in the QTc interval greater than 60 ms and patients on two drugs experienced a greater increase in QTc interval. The study included 30 critically ill patients who had a non-significant higher increase (26 ms) in the QTc interval compared to non-critically ill patients (16 ms). Our results have also shown a greater increase in the QTc interval in patients treated with more drugs.
Nekidy et al., in 111 critically ill COVID-19 patients, observed a prevalence of prolongation of the QTc interval of 77.5% following the same criteria defined in our study, and of QTc above 500 ms of 42%.14 These data contrast with our lower prevalence, even though patients had similar characteristics in terms of age, comorbidity, and proportion of patients on QTc-prolonging COVID-19 treatment drugs.14 The authors included the longest QTc interval observed during patient stay, which could increase the proportion of cases diagnosed with prolongation of the QTc interval. However, we cannot rule out that our series was affected by bias due to the low proportion in the recruitment of patients with available ECG.
It has recently been reported that prolongation of the QTc interval (above 440 ms in men and 450 ms in women) in 355 patients with COVID-19 was related to an increase in mortality at one year, with a hazard ratio of 1.69.15 This study included 55 critically ill patients in whom the proportion of QTc prolongation was around 45%. These values are higher than those observed in our series, although the limits of prolonged QTc values were wider in our study (450 ms in men and 460 ms in women). The authors related the presence of prolonged QTc with myocardial injury evaluated by cardiac biomarkers or echocardiographic alterations. We have found this association with both troponin T levels and the presence of elevated levels of NT-proBNP. The increase in troponin T suggests injury myocardial also described by other authors, especially in the most severe COVID-19 patients.4 On the other hand, the elevation of the NT-proBNP biomarker in critical care units is relatively frequent and is not necessarily associated with the presence of heart disease.16–18
In critically ill patients, multiple risk factors for presenting a prolonged QTc interval usually coexist due to both their concomitant diseases (heart disease, electrolyte abnormalities) and treatment with QT interval-prolonging drugs. Previous studies in critically ill patients show an incidence of prolonged QTc interval around 24%–28%.19–21 In patients with COVID-19, a higher incidence is described, suggesting a relevant role of the pro-inflammatory state in severe SARS-CoV-2 infection, and myocarditis associated with elevated troponins, which can also manifest with a prolongation of the QTc interval among other clinical signs.4,6,22,23
In our cohort, a significant percentage of patients developed arrhythmias. A large international study that evaluated the incidence of arrhythmias in patients with COVID-19, including critically ill patients, showed an incidence of around 12.9%.24 Similarly to our series the most frequently described arrhythmia was AF. The authors described that in patients on mechanical ventilation the incidence of arrhythmias was 43%, coinciding with our data. The survival of patients who developed arrhythmias was 51.4% in the international series, higher than that of our series of 41%, probably related to the differences in patients evaluated, considering that our population was exclusively critically ill patients. The incidence of arrhythmias has been reported since the first series of patients with COVID-19, with higher percentages in critical patients.5 Recently, the presence of atrial arrhythmias has been related to an increase in mortality in COVID-19 patients.25 We found no association between the presence of arrhythmias and mortality. The incidence of arrhythmias in non-COVID critical patients has been described as around 12%, with atrial tachyarrhythmias being the most frequently described.26,27 Again, the results in critical COVID-19 patients show higher rates of arrhythmic events, suggesting greater cardiovascular involvement in this population.
Mortality during ICU admission in our series was significant, 53%, in a range similar to that reported both by other groups in Spain and in a recent meta-analysis (43–83% in patients on mechanical ventilation).28,29 This disparity in mortality may be related to a great heterogeneity of patients with different morbidity and prognosis. In our series, although mortality was higher in patients with prolonged QTc (59% vs. 41%), it did not reach statistical significance. The observations shown in our study suggest the importance of actively monitoring the QTc interval and cardiac biomarkers to facilitate the establishment of protective measures in patients with severe COVID-19 infection.
LimitationsThis study has some limitations. Firstly, due to logistical limitations at the beginning of the pandemic, the ECG recording could not be recovered in all patients, which limits the determination of the real incidence in critical COVID-19 patients of prolonged QTc and arrhythmias. However, our data are in line with those reported by other authors in the same context. Another limitation refers to the fact that it is a retrospective and monocentric study that may involve relevant biases. However, the information provided is relevant, showing the involvement of ventricular repolarisation parameters and the association of arrhythmias in a population of critically ill patients with COVID-19.
ConclusionsIn our sample, a high proportion of critically ill patients with COVID-19 presented prolonged QTc and arrhythmias. The factors involved were related to the elevation of cardiac biomarkers, the myocardial involvement of the virus itself, and the concomitant medication received in the ICU.
Conflict of interestsThe authors declare that they have no conflict of interest with the contents of the manuscript.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.