Anaesthetic and surgical procedures in COVID-19 patients that require orotracheal intubation, extubation, secretion drainage and non-invasive mechanical ventilation are considered high risk for viral transmission. This is particularly true of anaesthesia and thoracic surgery, due to the need for frequent airway manipulation and exposure of the airway in the surgical field. This has prompted the Cardiac, Vascular and Thoracic Anaesthesia Division to review the recommendations endorsed by different international societies and the latest publications on this subject in order to advise anaesthesiologists on key aspects of thoracic surgery.
The overall rules for general anaesthesia in COVID-19 patients and patient transfers between hospital units do not differ from the general recommendations put forward by the SEDAR and other guidelines already published in specialty journals1.
The following recommendations are specifically related to thoracic surgery techniques2–4: 1) elective intubation is always preferable to emergency intubation; 2) High Efficiency Particulate Air (HEPA) antibacterial filters must always be used in the breathing circuit (inspiratory and expiratory limb and y-piece), in the lumen of the bronchial blocker (BB) or double lumen tube (DLT) placed in the surgical lung (or at both ends of the DLT if a sequential collapse is planned), when CPAP is used (limb corresponding to the collapsed lung) and/or between the chest drain and the reservoir; 3) if the patient is already intubated, prioritise BBs; 4) minimize exposure during BB or DLT insertion and/or repositioning; 5) always use closed circuit systems; 6) avoid respirator disconnections and make sure the valves are tightly sealed (prolong apnoea and clamp the endotracheal tube) when performing bronchoscopy or aspirating secretions; 7) plan for hypoxaemia management during one-lung ventilation; 8) perform a detailed evaluation of patients with moderate or severe ARDS secondary to COVID-19 based on the urgency of the surgical indication.
Intubation must be safe for the surgical team and appropriate for the patient. Avoid suboptimal, repeated attempts and innovative techniques (SAR = Safe, Adequate, Rapid). Ideally, anaesthesia should be induced in a negative pressure operating room. If this is not possible, increase and escalate safety measures. Pre-oxygenation with 100% FiO2 for at least 5 min is mandatory to avoid or at least reduce the need for manual ventilation during induction, which is performed by 2 anaesthesiologists. Premedicate with lidocaine or opioids to minimize the cough reflex, then perform rapid sequence induction for hypnosis and rapid neuromuscular relaxation (rocuronium 1.2 mg/kg).
After inserting the endotracheal tube (ETT) or TDL using a video laryngoscope, the device of choice1, the cuff must be inflated immediately, and always before starting mechanical ventilation. As many as 40% of SEDAR members participated in the CoV-2-VIAEREA study approved by the Institutional Review Board of the Valencia General University Hospital Consortium (April 24, 2020) and sponsored by SEDAR. Of these,14.4% had considerable experience in thoracic surgery, and rated their choice of video laryngoscope for DLT insertion as follows (6 top choice, 1 last choice) in descending order: C-MAC (4.1), Glidescope (4.1), Airtraq (3.4), McGrath (3.3) and King Vision (3.1).
Several guidelines on difficult airway (DA) management have been published5, but recommendations differ when treating COVID-19 patients1; awake intubation in a patient meeting DA criteria should be avoided and reserved solely for non-deferrable or emergency surgery. Administer mild intravenous sedation and avoid topical analgesics. If 3 attempts at intubation are unsuccessful in a patient with unanticipated DA, secure the airway with a 3rd generation supraglottic device and then perform intubation with a fibreoptic bronchoscope (FOB).
Regarding lung isolation and/or separation in COVID-19 patients: when only lung separation is required to optimize exposure during surgery, either DLTs or BBs can be used; when lung isolation is indicated5, use a DLT. In exceptional cases, intubate with an ETT and then exchange for a DLT.
The most obvious recommendations for lung isolation with a BB is in patients that are already intubated or that meet the criteria for DA, patients undergoing short surgical procedures, and in patients that will most likely require postoperative mechanical ventilation5. In the CoV-2-VIAEREA study, the BBs of choice for COVID-19 patients were, in descending order: Uniblocker (33.3%), Arndt (23.9%), Univent (18.1%), EZ Blocker (12.9%), Cohen (9.7%), and Coopdech (2.6%).
To verify correct placement of the DLT or BB, choose a single‐use rather than re-usable flexible bronchoscope, or a DLT or ETT with a built-in camera (Viva Sight DL® or Viva Sight SL®, respectively)2. DLTs are usually placed with the aid of FOB; however, the use of DLTs with a built-in camera has been gaining ground because they have several advantages over conventional DLTs: optimal insertion without the need for FOB in 99% of cases, shorter intubation time, and the possibility of correcting malpositioning without FOB, although FOB may be needed in 5%–15% of cases. In the CoV-2-VIAEREA study, anaesthesiologists rated pulmonary separation devices in COVID-19 patients as follows, in descending order (6 top choice, 1 last choice): Conventional DLT (4.7), DLT with built-in camera (3.9), BB through ETT with built-in camera (3.3), FOB-guided BB through ETT (3.2), UNIVENT tube and FOB (2.8) and FOB-guided endobronchial ETT (2.4).
General recommendations for the management of one-lung ventilation (ONL) in COVID-19 patients are the same as for lung protection, although patients are more prone to haemodynamic instability. It may be necessary to apply CPAP to the non-dependent lung, or extracorporeal membrane oxygenation (ECMO) might be required. There is no evidence to recommend performing thoracic surgery without intubation in patients with highly contagious diseases, so the use of non-invasive ventilation (NIV) and high flow nasal cannulas (HFNC) is not recommended during thoracic surgery2.
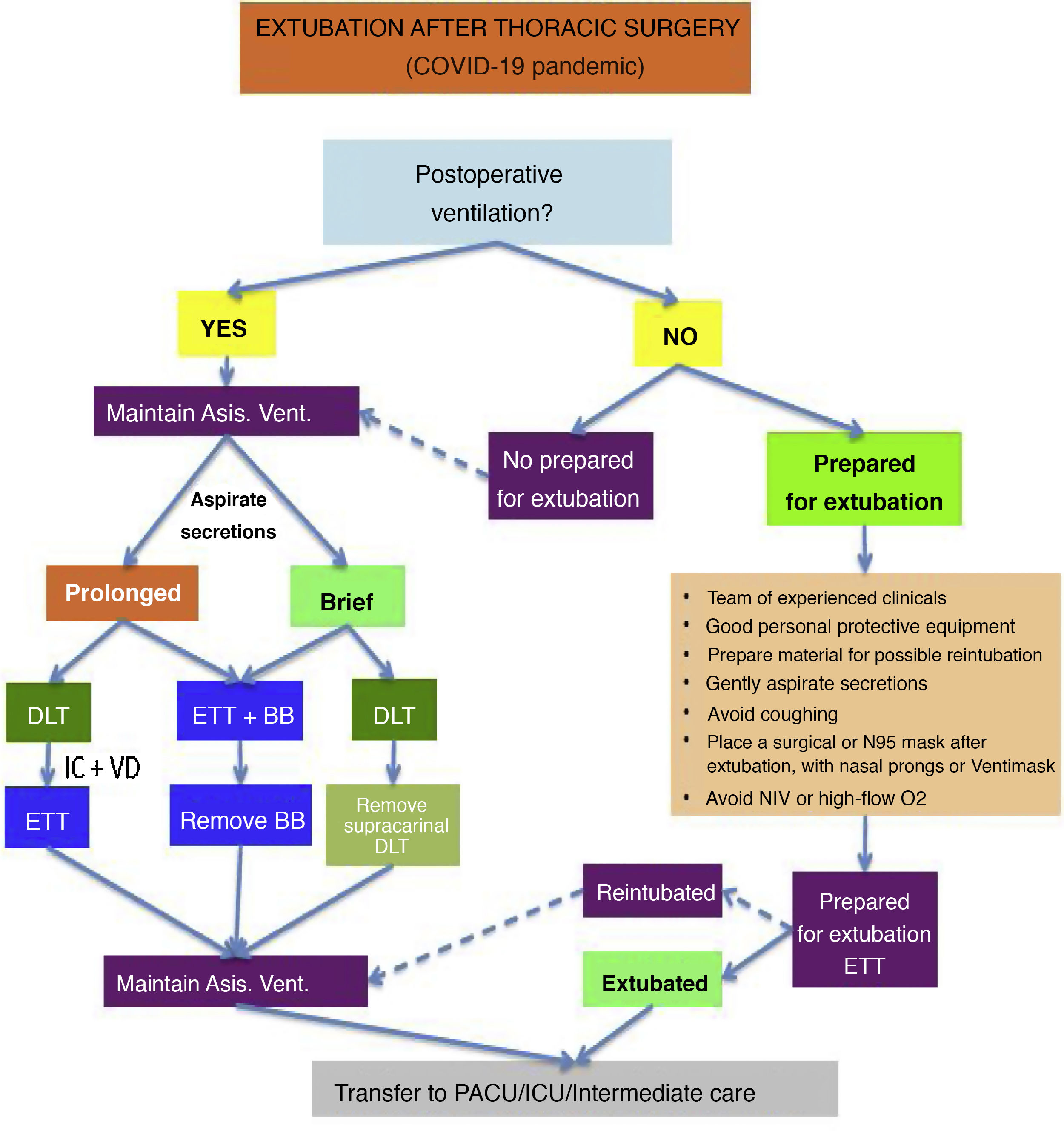
The timing of extubation must be decided on a case-by-case basis (Fig. 1), choosing the option that is safest for both the patient and healthcare workers. If the anaesthesiologist decides to extubate in the operating room due to the unlikelihood of postoperative mechanical ventilation and the patient’s stable status, the general guidelines for patients with suspected coronavirus should be followed1. In patients with DA, the recommendations provided by other authors should be followed5. When postoperative ventilation is required, proceed as follows: 1) remove any independent BBs or those attached to the Univent; 2) DLTs should be exchanged for an ETT with subglottic secretion drainage (high-risk manoeuvre); 3) if a DLT was used, but very brief postoperative ventilation is expected, the distal end of the DLT can be withdrawn as far as the trachea. Finally, in the CoV-2-VIAEREA study, anaesthesiologists rated extubation techniques as follows, in descending order: extubation in the operating room (89.5%), removal of the BB and transfer with an ETT (4.9%), exchange DLT for ETT and transfer to the ICU (4.9%), or withdraw the tip of the DLT to the trachea and transfer to the ICU (0.6%).
FundingThe authors have not received any funding.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Granell M, Sanchís N, López-Cantero M, Romero CS, Garutti I, Vicente R. Análisis y revisión del manejo perioperatorio del paciente COVID-19 en la cirugía torácica. Rev Esp Anestesiol Reanim. 2021;68:369–371.