We explored the experience of clinicians from the Spanish Society of Anesthesiology (SEDAR) in airway management of COVID-19 patients.
MethodsAn software-based survey including a 32-item questionnaire was conducted from April 18 to May 17, 2020. Participants who have been involved in tracheal intubations in patients with suspected or confirmed COVID-19 infection were included anonymously after obtaining their informed consent. The primary outcome was the preferred airway device for tracheal intubation. Secondary outcomes included the variations in clinical practice including the preferred video laryngoscope, plans for difficult airway management, and personal protective equipment.
Results1125 physicians completed the questionnaire with a response rate of 40,9%. Most participants worked in public hospitals and were anesthesiologists.
The preferred device for intubation was the video laryngoscope (5.1/6), with the type of device in decreasing order as follows: Glidescope, C-MAC, Airtraq, McGrath and King Vision. The most frequently used device for intubation was the video laryngoscope (70,5%), using them in descending order as follow: the Airtraq, C-MAC, Glidescope, McGrath and King Vision.
Discomfort of intubating wearing personal protective equipment and the frequency of breaching a security step was statistically significant, increasing the risk of cross infection between patients and healthcare workers. The opinion of senior doctors differed from younger physicians in the type of video-laryngoscope used, the number of experts involved in tracheal intubation and the reason that caused more stress during the airway management.
ConclusionsMost physicians preferred using a video-laryngoscope with remote monitor and disposable Macintosh blade, using the Frova guide.
Analizamos la experiencia de médicos de la Sociedad Española de Anestesiología (SEDAR) en el manejo de vía aérea de pacientes COVID-19.
MétodosSe realizó una encuesta que incluía 32 ítems (18 abril-17 mayo de 2020). Participaron de forma anónima tras aceptar el consentimiento informado médicos involucrados en intubaciones traqueales en pacientes COVID-19 confirmados o con sospecha. El resultado principal fue el dispositivo de vía aérea preferido para la intubación traqueal. Los resultados secundarios incluyeron el análisis de la práctica clínica, el videolaringoscopio preferido, manejo de vía aérea difícil y uso de equipo de protección personal.
ResultadosCompletaron el cuestionario 1125 médicos (tasa de respuesta del 40,9%) que eran mayoritariamente anestesiólogos y trabajaban en hospitales públicos.
El dispositivo preferido para intubar fue el videolaringoscopio (5.1/6) con el siguiente orden de preferencia: Glidescope, C-MAC, Airtraq, McGrath y King Vision. El dispositivo de intubación más utilizado fue el videolaringoscopio (70,5%) con el siguiente orden decreciente: Airtraq, C-MAC, Glidescope, McGrath y King Vision.
La relación de incomodidad de la intubación con equipo de protección personal y la frecuencia de incumplimiento de un paso de seguridad fue estadísticamente significativa, aumentando el riesgo de infección cruzada. La opinión de los médicos senior difería de los más jóvenes en el videolaringoscopio utilizado, número de expertos involucrados en la intubación traqueal y la razón que provocó más estrés durante el manejo de la vía aérea.
ConclusionesLa mayoría de los médicos prefirieron usar un videolaringoscopio con monitor remoto y hoja Macintosh desechable, usando la guía Frova.
Tracheal intubation, tracheostomy, and lung protective mechanical ventilation strategies are core treatments in patients infected with the new coronavirus (Severe Acute Respiratory Syndrome coronavirus-2 [SARS-CoV-2]). High risk patients with some type of comorbidity present an inherent risk of severe hypoxaemia and critical reduction in peripheral oxygen saturation, not to mention the risk of cross infection between patients and healthcare workers. Another important consideration is fear of infection among healthcare workers and the discomfort associated with the use of personal protective equipment (PPE)1.
According to official data from the National Epidemiological Surveillance Network of the Ministry of Health of Spain accessed on 21 May 2020 at 11:00 am, 40,921 cases of COVID-19 had been diagnosed among healthcare workers by 11 May 2020, with 4177 hospital admissions, 310 ICU admissions (1.1%) and 53 deaths (0.1%)2. COVID-19 infection in healthcare workers accounted for 16.3% of the 250,273 COVID-19 cases reported as of 10 May 2020. Several aerosol-generating procedures, including endotracheal intubation, manual ventilation by an assistant, tracheostomy, and non-invasive ventilation have been associated with a high risk of viral transmission3.
Clinicians can also use the latest devices to protect themselves during airway management manoeuvres in COVID-19 patients, such as the aerosol box4.
The Spanish Society of Anaesthesiology and Resuscitation (SEDAR) conducted a survey on airway management in patients with COVID-19.
Material and methodBetween 28 April and 17 May 2020, SEDAR conducted a national online survey based on a 32-item questionnaire. The survey was approved by the Clinical Research Ethics Committee (CEIm) of the Consorci Hospital General Universitari de València (registration number CPMP/ICH/135/95, approved on 24 April 2020) and conducted by the Spanish COV2-VIAEREA Network study group. The study was registered at https://clinicaltrials.gov.
The questionnaire was sent to members of SEDAR, the Spanish Society of Intensive and Critical Care Medicine and Coronary Units, the Spanish Society of Emergency Medicine, the Spanish Society of Cardiology, the Spanish Society of Pulmonology and Thoracic Surgery, and the Spanish Society of Internal Medicine who had performed tracheal intubation in patients with suspected or confirmed COVID-19, and who gave their consent to participate (Tables 1 and 2).
Survey respondent characteristics.
| Questionnaire items | Number (%) |
|---|---|
| Which of the following describes your place of work? | |
| Public hospital | 912 (81.1) |
| Private hospital | 53 (4.7) |
| Public-private hospital | 95 (8.4) |
| Out-of-hospital care | 65 (5.8) |
| Number of years as a specialist (years), mean (SD) | 13 (10) |
| In which specialist capacity have you had experience with airway management in COVID-19 patients? | |
| Anaesthesiology | 1024 (91.0)* |
| Intensive medicine | 65 (5.7) |
| Emergency medicine and emergencies | 32 (2.8) |
| Cardiology | 1 (0.08) |
| Pulmonology | 2 (0.1) |
| Internal medicine | 1 (0.08) |
| In your experience, where have you intubated most COVID-19 patients? | |
| Emergency care/Out-of-hospital emergency | 67 (5.9) |
| Hospital Emergency Department | 77 (6.8) |
| Intensive Care Unit/Resuscitation Unit | 688 (61.2) |
| Urgent surgery operating room | 228 (20.3) |
| Scheduled surgery operating room | 47 (4.2) |
| Hospital ward | 18 (1.6) |
| Have you been infected with the SARS-COVID 2 during your work as a front-line healthcare worker during the COVID-19 pandemic? | |
| Yes, I was diagnosed by PCR or serology | 132 (11.7) |
| No, my PCR or serology was negative | 731 (65.1) |
| I have never been tested because I have been asymptomatic | 224 (19.9) |
| I have never been tested, although I have had symptoms | 38 (3.4) |
A total of 2503 SEDAR members were contacted by email and through social networks. The response rate was 40.9%.
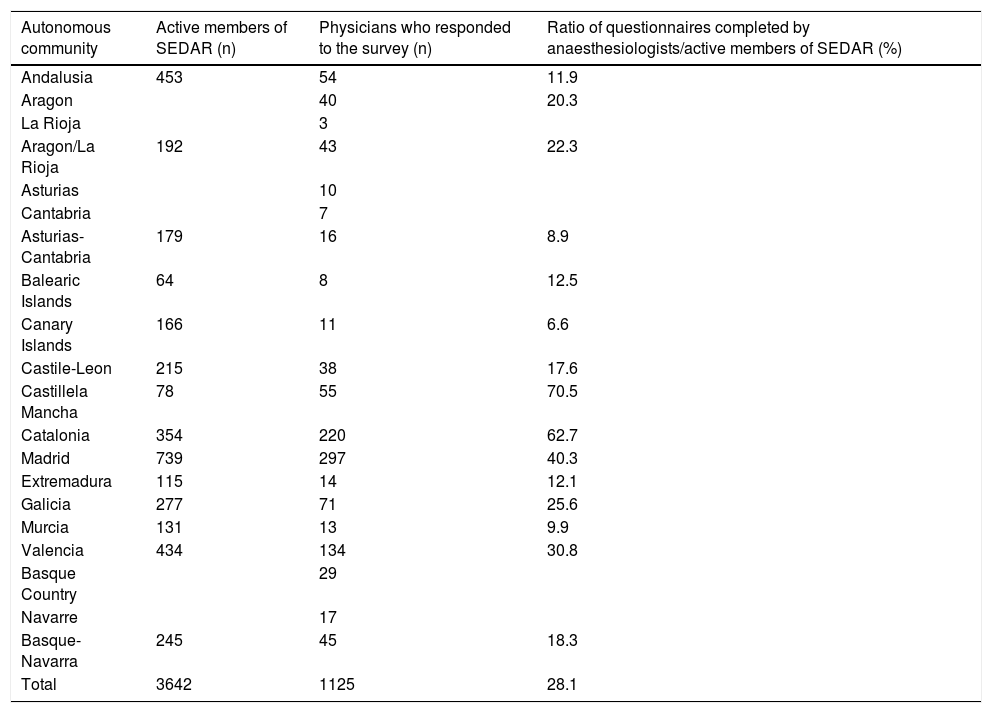
Distribution of anaesthesiologists by Spanish autonomous communities.
| Autonomous community | Active members of SEDAR (n) | Physicians who responded to the survey (n) | Ratio of questionnaires completed by anaesthesiologists/active members of SEDAR (%) |
|---|---|---|---|
| Andalusia | 453 | 54 | 11.9 |
| Aragon | 40 | 20.3 | |
| La Rioja | 3 | ||
| Aragon/La Rioja | 192 | 43 | 22.3 |
| Asturias | 10 | ||
| Cantabria | 7 | ||
| Asturias-Cantabria | 179 | 16 | 8.9 |
| Balearic Islands | 64 | 8 | 12.5 |
| Canary Islands | 166 | 11 | 6.6 |
| Castile-Leon | 215 | 38 | 17.6 |
| Castillela Mancha | 78 | 55 | 70.5 |
| Catalonia | 354 | 220 | 62.7 |
| Madrid | 739 | 297 | 40.3 |
| Extremadura | 115 | 14 | 12.1 |
| Galicia | 277 | 71 | 25.6 |
| Murcia | 131 | 13 | 9.9 |
| Valencia | 434 | 134 | 30.8 |
| Basque Country | 29 | ||
| Navarre | 17 | ||
| Basque-Navarra | 245 | 45 | 18.3 |
| Total | 3642 | 1125 | 28.1 |
A prerequisite for inclusion in the survey was access to the online Microsoft Forms platform. Participation was anonymous, voluntary and unpaid. The informed consent form was the first item in the questionnaire.
The primary conclusion was clinician preference for a specific airway device (Table 3), and the most widely-used airway device for intubation in patients with COVID-19 (Table 4).
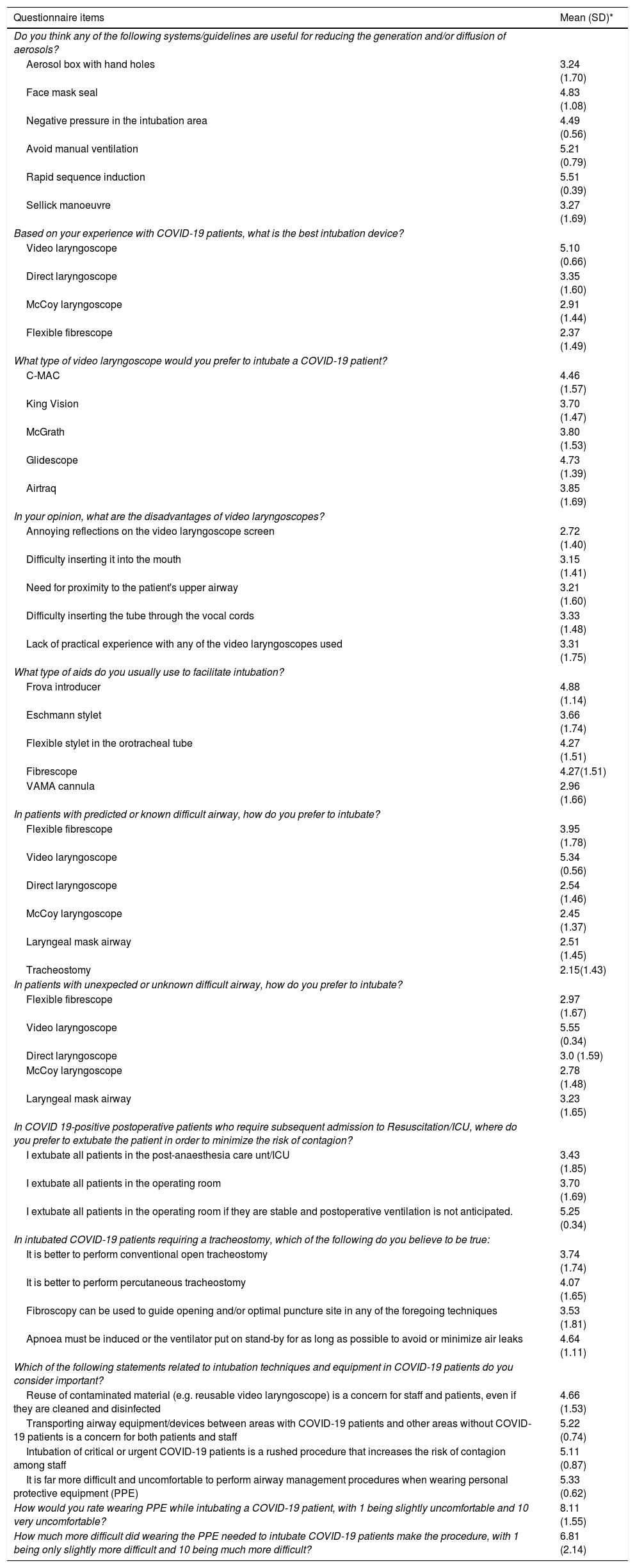
Airway management preferences.
| Questionnaire items | Mean (SD)* |
|---|---|
| Do you think any of the following systems/guidelines are useful for reducing the generation and/or diffusion of aerosols? | |
| Aerosol box with hand holes | 3.24 (1.70) |
| Face mask seal | 4.83 (1.08) |
| Negative pressure in the intubation area | 4.49 (0.56) |
| Avoid manual ventilation | 5.21 (0.79) |
| Rapid sequence induction | 5.51 (0.39) |
| Sellick manoeuvre | 3.27 (1.69) |
| Based on your experience with COVID-19 patients, what is the best intubation device? | |
| Video laryngoscope | 5.10 (0.66) |
| Direct laryngoscope | 3.35 (1.60) |
| McCoy laryngoscope | 2.91 (1.44) |
| Flexible fibrescope | 2.37 (1.49) |
| What type of video laryngoscope would you prefer to intubate a COVID-19 patient? | |
| C-MAC | 4.46 (1.57) |
| King Vision | 3.70 (1.47) |
| McGrath | 3.80 (1.53) |
| Glidescope | 4.73 (1.39) |
| Airtraq | 3.85 (1.69) |
| In your opinion, what are the disadvantages of video laryngoscopes? | |
| Annoying reflections on the video laryngoscope screen | 2.72 (1.40) |
| Difficulty inserting it into the mouth | 3.15 (1.41) |
| Need for proximity to the patient's upper airway | 3.21 (1.60) |
| Difficulty inserting the tube through the vocal cords | 3.33 (1.48) |
| Lack of practical experience with any of the video laryngoscopes used | 3.31 (1.75) |
| What type of aids do you usually use to facilitate intubation? | |
| Frova introducer | 4.88 (1.14) |
| Eschmann stylet | 3.66 (1.74) |
| Flexible stylet in the orotracheal tube | 4.27 (1.51) |
| Fibrescope | 4.27(1.51) |
| VAMA cannula | 2.96 (1.66) |
| In patients with predicted or known difficult airway, how do you prefer to intubate? | |
| Flexible fibrescope | 3.95 (1.78) |
| Video laryngoscope | 5.34 (0.56) |
| Direct laryngoscope | 2.54 (1.46) |
| McCoy laryngoscope | 2.45 (1.37) |
| Laryngeal mask airway | 2.51 (1.45) |
| Tracheostomy | 2.15(1.43) |
| In patients with unexpected or unknown difficult airway, how do you prefer to intubate? | |
| Flexible fibrescope | 2.97 (1.67) |
| Video laryngoscope | 5.55 (0.34) |
| Direct laryngoscope | 3.0 (1.59) |
| McCoy laryngoscope | 2.78 (1.48) |
| Laryngeal mask airway | 3.23 (1.65) |
| In COVID 19-positive postoperative patients who require subsequent admission to Resuscitation/ICU, where do you prefer to extubate the patient in order to minimize the risk of contagion? | |
| I extubate all patients in the post-anaesthesia care unt/ICU | 3.43 (1.85) |
| I extubate all patients in the operating room | 3.70 (1.69) |
| I extubate all patients in the operating room if they are stable and postoperative ventilation is not anticipated. | 5.25 (0.34) |
| In intubated COVID-19 patients requiring a tracheostomy, which of the following do you believe to be true: | |
| It is better to perform conventional open tracheostomy | 3.74 (1.74) |
| It is better to perform percutaneous tracheostomy | 4.07 (1.65) |
| Fibroscopy can be used to guide opening and/or optimal puncture site in any of the foregoing techniques | 3.53 (1.81) |
| Apnoea must be induced or the ventilator put on stand-by for as long as possible to avoid or minimize air leaks | 4.64 (1.11) |
| Which of the following statements related to intubation techniques and equipment in COVID-19 patients do you consider important? | |
| Reuse of contaminated material (e.g. reusable video laryngoscope) is a concern for staff and patients, even if they are cleaned and disinfected | 4.66 (1.53) |
| Transporting airway equipment/devices between areas with COVID-19 patients and other areas without COVID-19 patients is a concern for both patients and staff | 5.22 (0.74) |
| Intubation of critical or urgent COVID-19 patients is a rushed procedure that increases the risk of contagion among staff | 5.11 (0.87) |
| It is far more difficult and uncomfortable to perform airway management procedures when wearing personal protective equipment (PPE) | 5.33 (0.62) |
| How would you rate wearing PPE while intubating a COVID-19 patient, with 1 being slightly uncomfortable and 10 very uncomfortable? | 8.11 (1.55) |
| How much more difficult did wearing the PPE needed to intubate COVID-19 patients make the procedure, with 1 being only slightly more difficult and 10 being much more difficult? | 6.81 (2.14) |
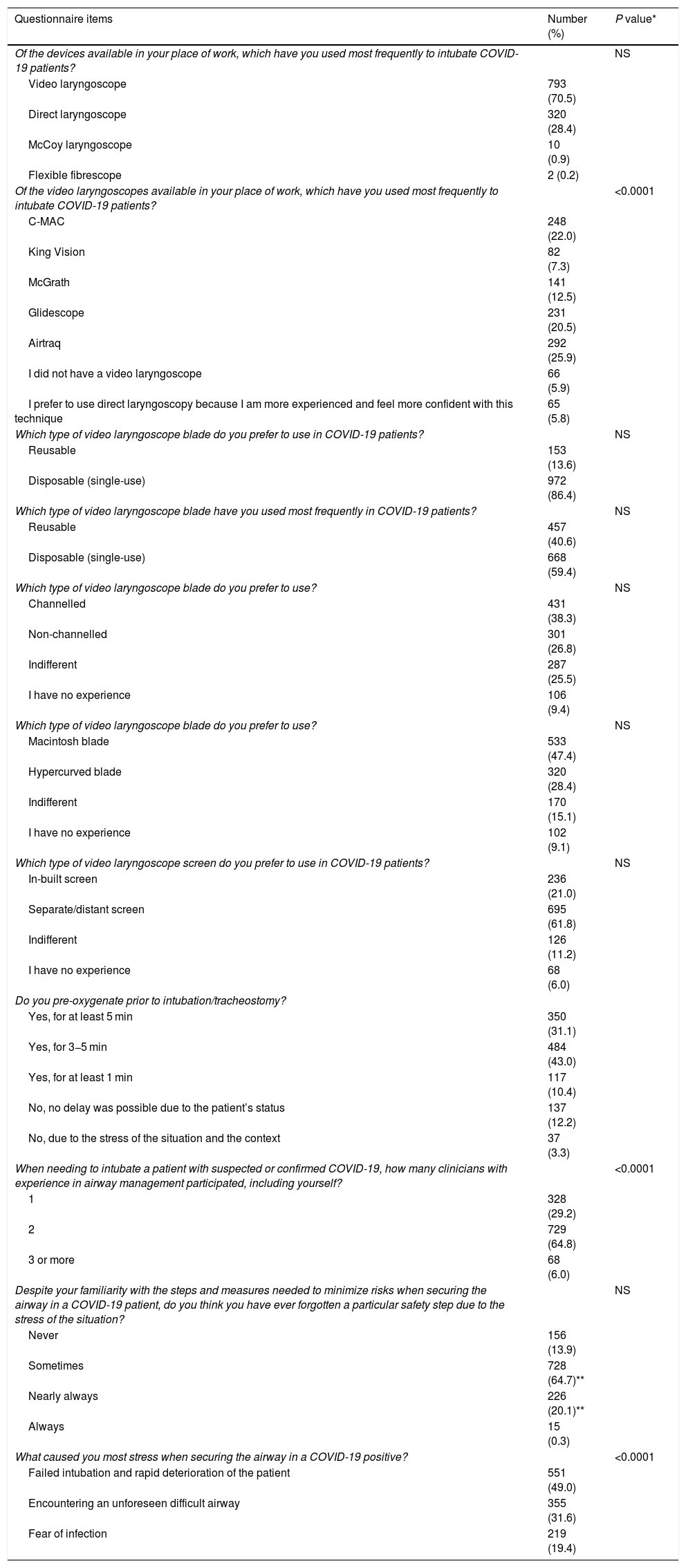
Airway management techniques in COVID-19 patients.
| Questionnaire items | Number (%) | P value* |
|---|---|---|
| Of the devices available in your place of work, which have you used most frequently to intubate COVID-19 patients? | NS | |
| Video laryngoscope | 793 (70.5) | |
| Direct laryngoscope | 320 (28.4) | |
| McCoy laryngoscope | 10 (0.9) | |
| Flexible fibrescope | 2 (0.2) | |
| Of the video laryngoscopes available in your place of work, which have you used most frequently to intubate COVID-19 patients? | <0.0001 | |
| C-MAC | 248 (22.0) | |
| King Vision | 82 (7.3) | |
| McGrath | 141 (12.5) | |
| Glidescope | 231 (20.5) | |
| Airtraq | 292 (25.9) | |
| I did not have a video laryngoscope | 66 (5.9) | |
| I prefer to use direct laryngoscopy because I am more experienced and feel more confident with this technique | 65 (5.8) | |
| Which type of video laryngoscope blade do you prefer to use in COVID-19 patients? | NS | |
| Reusable | 153 (13.6) | |
| Disposable (single-use) | 972 (86.4) | |
| Which type of video laryngoscope blade have you used most frequently in COVID-19 patients? | NS | |
| Reusable | 457 (40.6) | |
| Disposable (single-use) | 668 (59.4) | |
| Which type of video laryngoscope blade do you prefer to use? | NS | |
| Channelled | 431 (38.3) | |
| Non-channelled | 301 (26.8) | |
| Indifferent | 287 (25.5) | |
| I have no experience | 106 (9.4) | |
| Which type of video laryngoscope blade do you prefer to use? | NS | |
| Macintosh blade | 533 (47.4) | |
| Hypercurved blade | 320 (28.4) | |
| Indifferent | 170 (15.1) | |
| I have no experience | 102 (9.1) | |
| Which type of video laryngoscope screen do you prefer to use in COVID-19 patients? | NS | |
| In-built screen | 236 (21.0) | |
| Separate/distant screen | 695 (61.8) | |
| Indifferent | 126 (11.2) | |
| I have no experience | 68 (6.0) | |
| Do you pre-oxygenate prior to intubation/tracheostomy? | ||
| Yes, for at least 5 min | 350 (31.1) | |
| Yes, for 3−5 min | 484 (43.0) | |
| Yes, for at least 1 min | 117 (10.4) | |
| No, no delay was possible due to the patient’s status | 137 (12.2) | |
| No, due to the stress of the situation and the context | 37 (3.3) | |
| When needing to intubate a patient with suspected or confirmed COVID-19, how many clinicians with experience in airway management participated, including yourself? | <0.0001 | |
| 1 | 328 (29.2) | |
| 2 | 729 (64.8) | |
| 3 or more | 68 (6.0) | |
| Despite your familiarity with the steps and measures needed to minimize risks when securing the airway in a COVID-19 patient, do you think you have ever forgotten a particular safety step due to the stress of the situation? | NS | |
| Never | 156 (13.9) | |
| Sometimes | 728 (64.7)** | |
| Nearly always | 226 (20.1)** | |
| Always | 15 (0.3) | |
| What caused you most stress when securing the airway in a COVID-19 positive? | <0.0001 | |
| Failed intubation and rapid deterioration of the patient | 551 (49.0) | |
| Encountering an unforeseen difficult airway | 355 (31.6) | |
| Fear of infection | 219 (19.4) |
Secondary conclusions were clinical practice variables (use of pre-oxygenation), the use of video laryngoscopes, difficult airway approach, and the use of safety methods/procedures to prevent the risk of cross-infection between patients and healthcare workers (Tables 3–7).
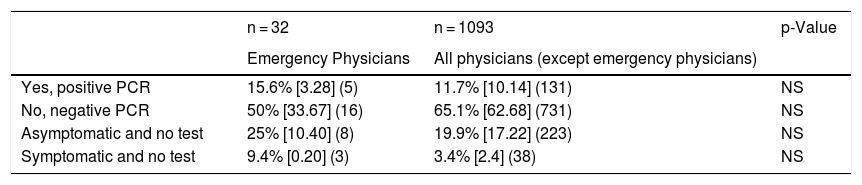
COVID-19 infection in emergency physicians vs other specialists.
| n = 32 | n = 1093 | p-Value | |
|---|---|---|---|
| Emergency Physicians | All physicians (except emergency physicians) | ||
| Yes, positive PCR | 15.6% [3.28] (5) | 11.7% [10.14] (131) | NS |
| No, negative PCR | 50% [33.67] (16) | 65.1% [62.68] (731) | NS |
| Asymptomatic and no test | 25% [10.40] (8) | 19.9% [17.22] (223) | NS |
| Symptomatic and no test | 9.4% [0.20] (3) | 3.4% [2.4] (38) | NS |
[95% confidence interval] (number).
Chi square test for independent samples.
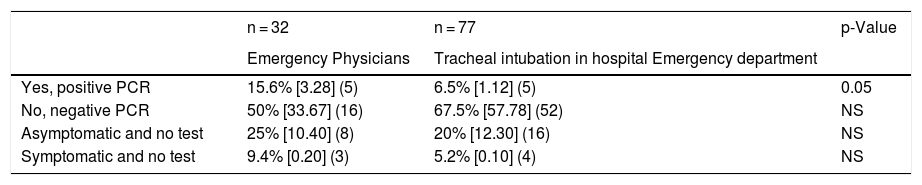
COVID-19 infection in the Emergency area.
| n = 32 | n = 77 | p-Value | |
|---|---|---|---|
| Emergency Physicians | Tracheal intubation in hospital Emergency department | ||
| Yes, positive PCR | 15.6% [3.28] (5) | 6.5% [1.12] (5) | 0.05 |
| No, negative PCR | 50% [33.67] (16) | 67.5% [57.78] (52) | NS |
| Asymptomatic and no test | 25% [10.40] (8) | 20% [12.30] (16) | NS |
| Symptomatic and no test | 9.4% [0.20] (3) | 5.2% [0.10] (4) | NS |
[95% confidence interval] (number).
Chi square test for independent samples.
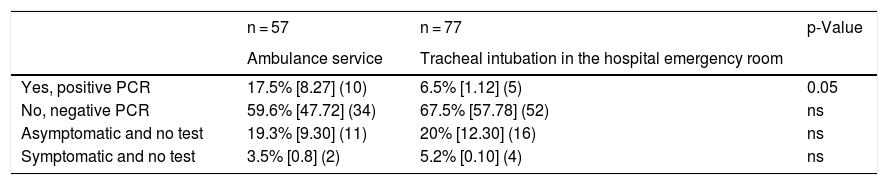
COVID-19 infection in the emergency room or out-of-hospital setting.
| n = 57 | n = 77 | p-Value | |
|---|---|---|---|
| Ambulance service | Tracheal intubation in the hospital emergency room | ||
| Yes, positive PCR | 17.5% [8.27] (10) | 6.5% [1.12] (5) | 0.05 |
| No, negative PCR | 59.6% [47.72] (34) | 67.5% [57.78] (52) | ns |
| Asymptomatic and no test | 19.3% [9.30] (11) | 20% [12.30] (16) | ns |
| Symptomatic and no test | 3.5% [0.8] (2) | 5.2% [0.10] (4) | ns |
[95% confidence interval] (number).
Chi square test for independent samples.
The first draft of the questionnaire was developed and reviewed by 4 experienced anaesthesiologists. The questionnaire was tested and validated by 9 independent physicians with at least 5 years of experience, including 2 anaesthesiologists, 2 intensivists, 2 emergency care specialists, a cardiologist, a pulmonologist, and a member of the ambulance service. Most items were single-answer questions, but 6-point Likert scale questions were also included (1 = totally disagree, 6 = totally agree). The survey was conducted on the Microsoft Forms Office 365 platform (Microsoft, Redmond, Washington, USA).
Answers to all questions had to be included in the final analysis. A link to the survey was posted on various social media platforms, including LinkedIn, Facebook, and Twitter. Participants were recruited using the snowball sampling technique.
Sample size calculationSelection bias was reduced by posting the survey mainly on social networks and collecting between 800 and 1300 completed questionnaires from at least 10 autonomous communities. This number was estimated on the basis of data from the Spanish Society of Anaesthesiology, and corresponded to 10% of physicians in each autonomous community.
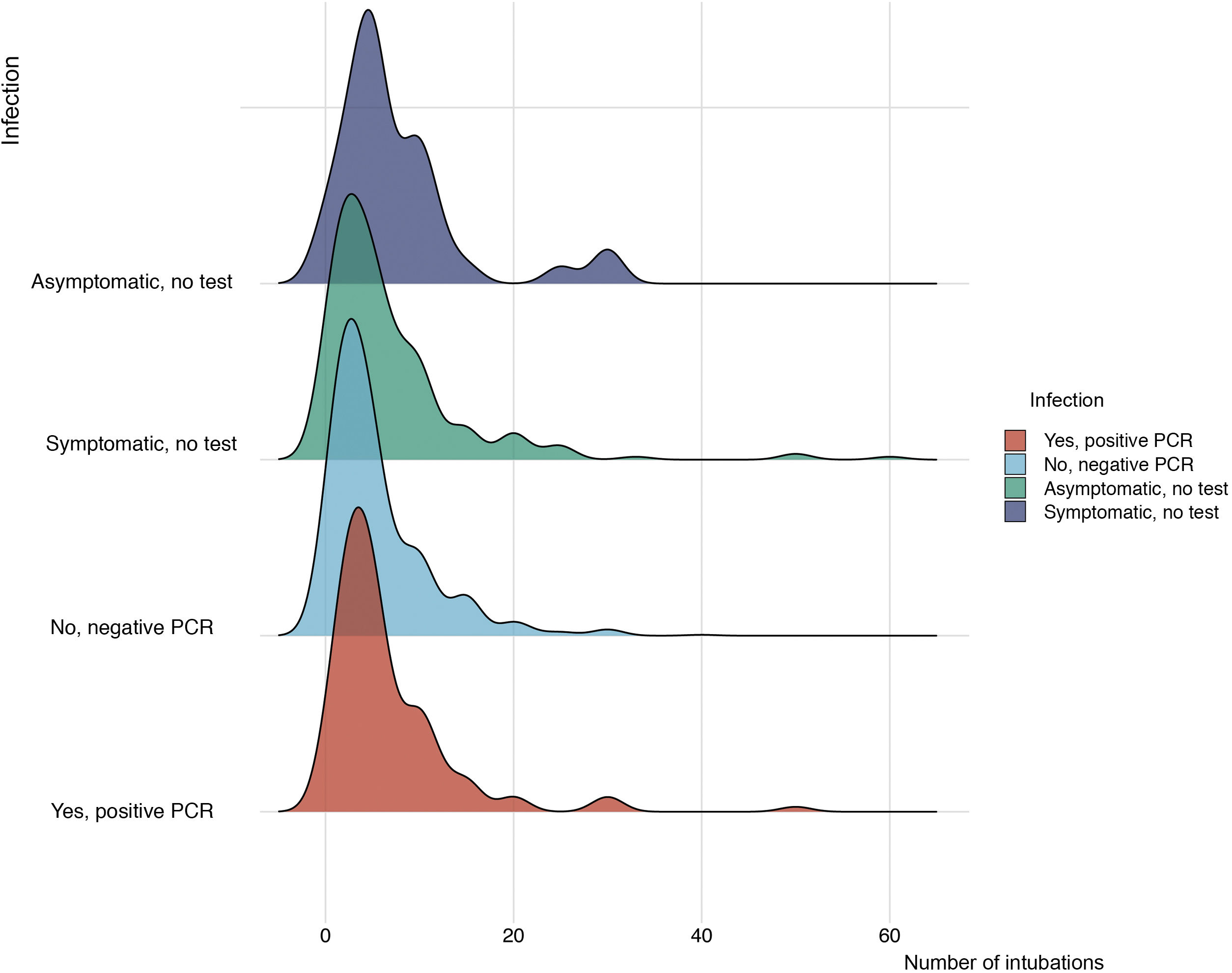
Statistical analysisCategorical variables are expressed as frequencies and percentages, and quantitative variables as mean and standard deviation (SD) or median and range. One-way analysis of variance (ANOVA) and the Tukey multiple comparison test were used to analyse the Likert categories «I never forget» and «I nearly always forget» in the Forgetting safety steps variable, and “at times” and “nearly always” for the PPE discomfort variable. As all the points on the ordinal scale were equidistant, they were analysed as a continuous variable according to Long and Freese5, who stated that an ordinal variable can be treated as though it had linear effects; doing so may be sufficiently offset any disadvantage. The variable “seniority” referred to years of experience, and was evaluated as a continuous variable for the comparison of “preferred video laryngoscope”, “most widely-used device”, “preferred blade”, “most widely-used blade” and “number of experts during intubation”. The variables “number of intubations performed” and “infection” were analysed with the Kruskal–Wallis test. Statistical significance was set at p < 0.05. The sample size was calculated for a confidence interval of 95% and a margin of error of 3%, for which a total of 1068 questionnaire respondents were needed (α = 0.05 and β = 0.80). The statistical program R (version 3.5.2) was used for data analysis6.
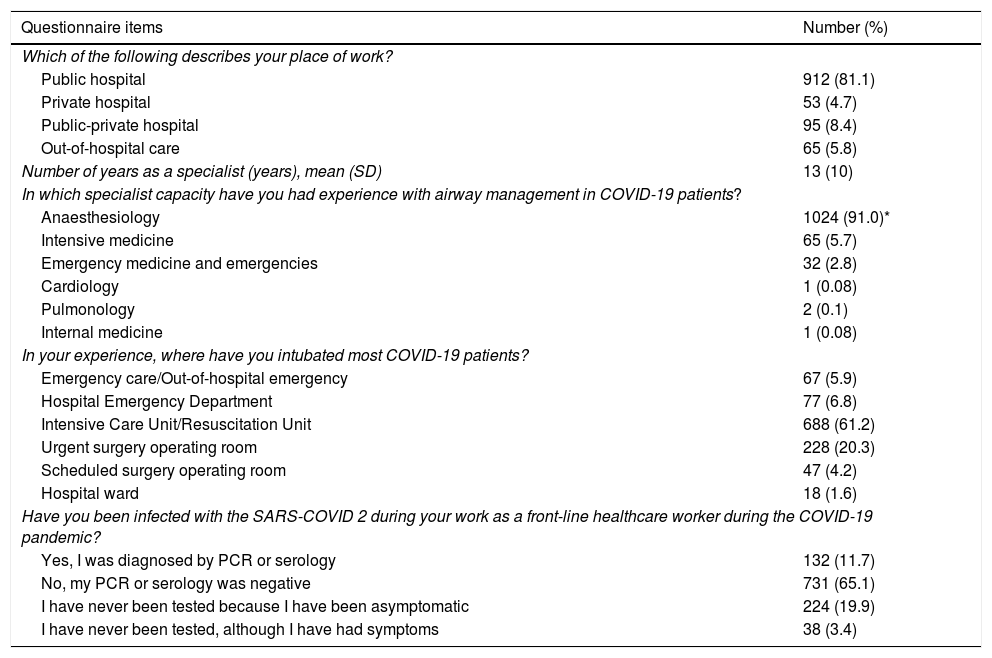
ResultsA total of 1125 physicians with a mean age (SD) of 42 (10) years and a mean of 13 (10) years’ experience in their specialties completed the questionnaire. They had performed 6,816 orotracheal intubations, with a mean of 6 procedures per physician (Table 1).
As shown in Table 1, most respondents worked in public hospitals (81.1%) and were anaesthesiologists (91.0%); 5.8% were specialists in Intensive Care Medicine and 2.8% were specialists in Emergency Medicine.
More than 60% of COVID-19 patients were intubated in the ICU, 20.3% in operating rooms when urgent surgery was required, and 6.8% in the hospital emergency department. In total, 74.1% of participants pre-oxygenated the patient for 3−5 min or more than 5 min prior to intubation compared with 10.4% who performed this manoeuvre for less than 1 min. Pre-oxygenation was not performed by 15.5% of participants due to the critical condition of the patient or a stressful personal situation (Table 4).
A total of 1125 physicians completed the entire questionnaire, with a response rate of 40.9% among the anaesthesiologists contacted (1,024 anaesthesiologists/2,503 SEDAR members contacted by email and social media). In total, 28.1% of all active SEDAR members took part in the survey, and participation rates exceeded 10% in most autonomous communities (14/17). Therefore, we believe the survey is representative of these communities and of Spain as a whole (Table 2). The autonomous communities with the highest number of participants were those with the highest incidence of COVID-19, particularly Madrid, Catalonia and Valencia.
Regarding preferences in airway management (Table 3), the preferred device for intubation was the video laryngoscope (5.10/6), followed by (in descending order of preference): Glidescope, C-MAC, Airtraq, McGrath and King Vision.
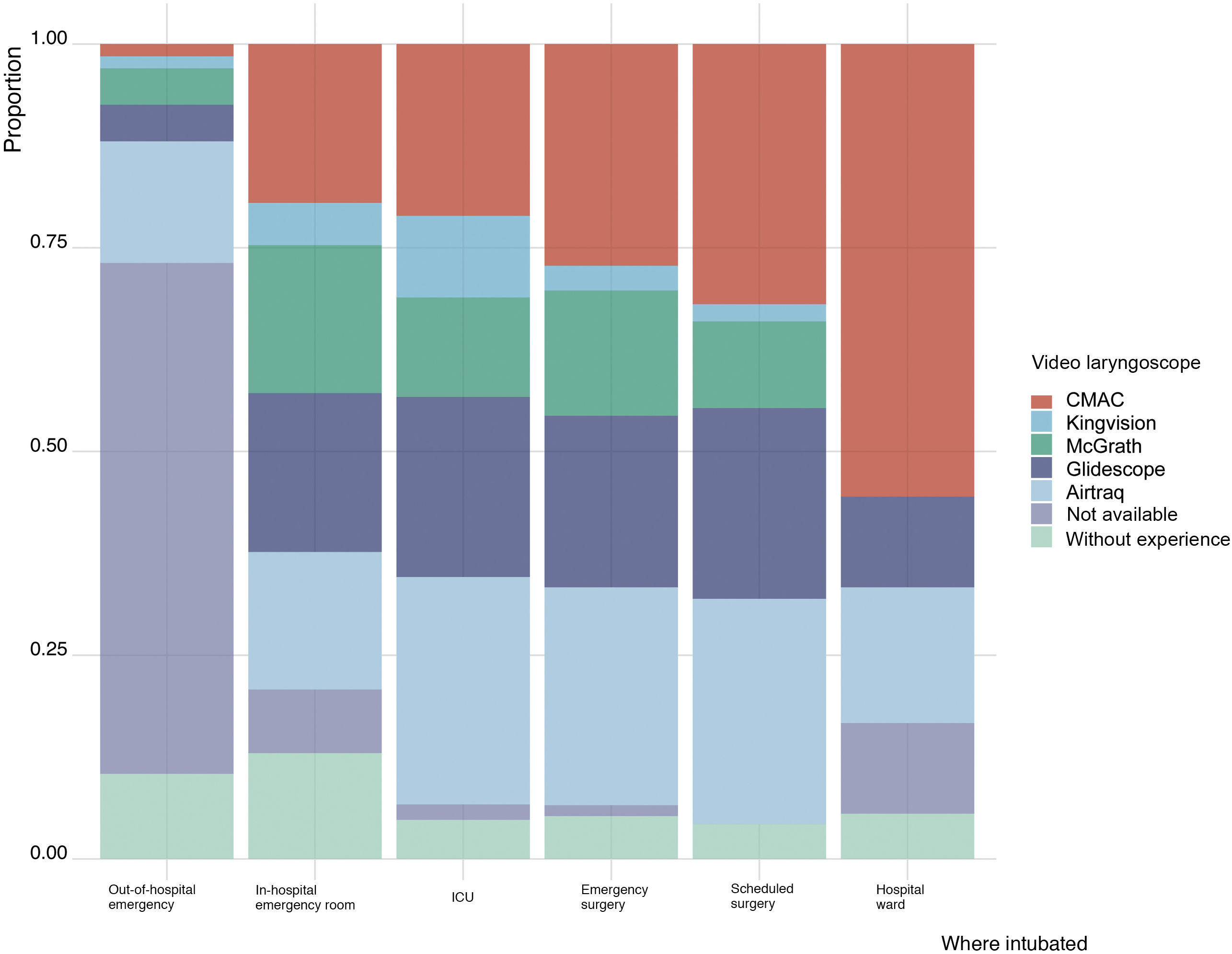
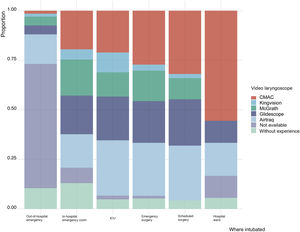
The most widely-used video laryngoscopes were the following, in descending order: Airtraq, C-MAC, Glidescope, McGrath and King Vision. The Airtraq was the most widely-used video laryngoscope in the ambulance service, in the ICU, and in patients undergoing urgent surgical procedures, while the C-MAC was the video laryngoscope most commonly used during scheduled surgery and on the hospital ward (Fig. 1).
Regarding video laryngoscope blades (Table 4), most respondents preferred video laryngoscopes with a disposable blade (86.4%), followed by curved Macintosh blade (47.4%) and channelled blades (38.3%), and most respondents preferred using a videolaryngoscope with a separate screen (61.8%). In terms of airway management devices, most respondents used disposable video laryngoscopes (70.5%) and blades (59.4%).
The video laryngoscope was the preferred intubation device in cases of suspected or unanticipated difficult airway. The Frova introducer, the flexible stylet in the orotracheal tube, and the fibreoptic bronchoscope were the preferred methods of facilitating tracheal intubation (Table 3).
A total of 131 physicians (11.6%) did not use any type of video laryngoscope (Table 4), either because they were unavailable or due to personal preference for conventional laryngoscopy. Ambulance service personnel used direct laryngoscopy in 87.5% of cases.
In 70.8% of cases, 2 or more physicians participated in tracheal intubation of COVID-19 patients. When asked to evaluate the impact of stress associated with the clinical management of COVID-19 patients, 969 physicians (86.1%) admitted they "forget one or more safety steps". For respondents, intubation failure and deterioration of the patient's status are the most stressful circumstance (49%), followed by a difficult airway (31.6%) and fear of contagion (19.4%). The variable Seniority (years of experience) correlated significantly with the type of video laryngoscope most widely used, the number of expert physicians who participated in intubation, and the most stressful circumstance (Table 3). Respondents considered PPE to be very uncomfortable and a significant hindrance for intubation. Furthermore, 64.7% of respondents stated that they were Sometimes and 20.1% that they were almost always unable to comply with safety measures due to the discomfort of wearing PPE. This difference was statistically significant (p < 0.0001).
Regarding extubation, respondents preferred to intubate in the operating room if the patient was stable and there was no need for postoperative mechanical ventilation.
In terms of tracheostomy, respondents showed a similar preference for percutaneous or open tracheostomy. They also considered fibreoptic guidance to be relatively acceptable during these techniques (3.5/6), and considered it very important to induce apnoea during the period of greatest risk of air leaks (4.6/6).
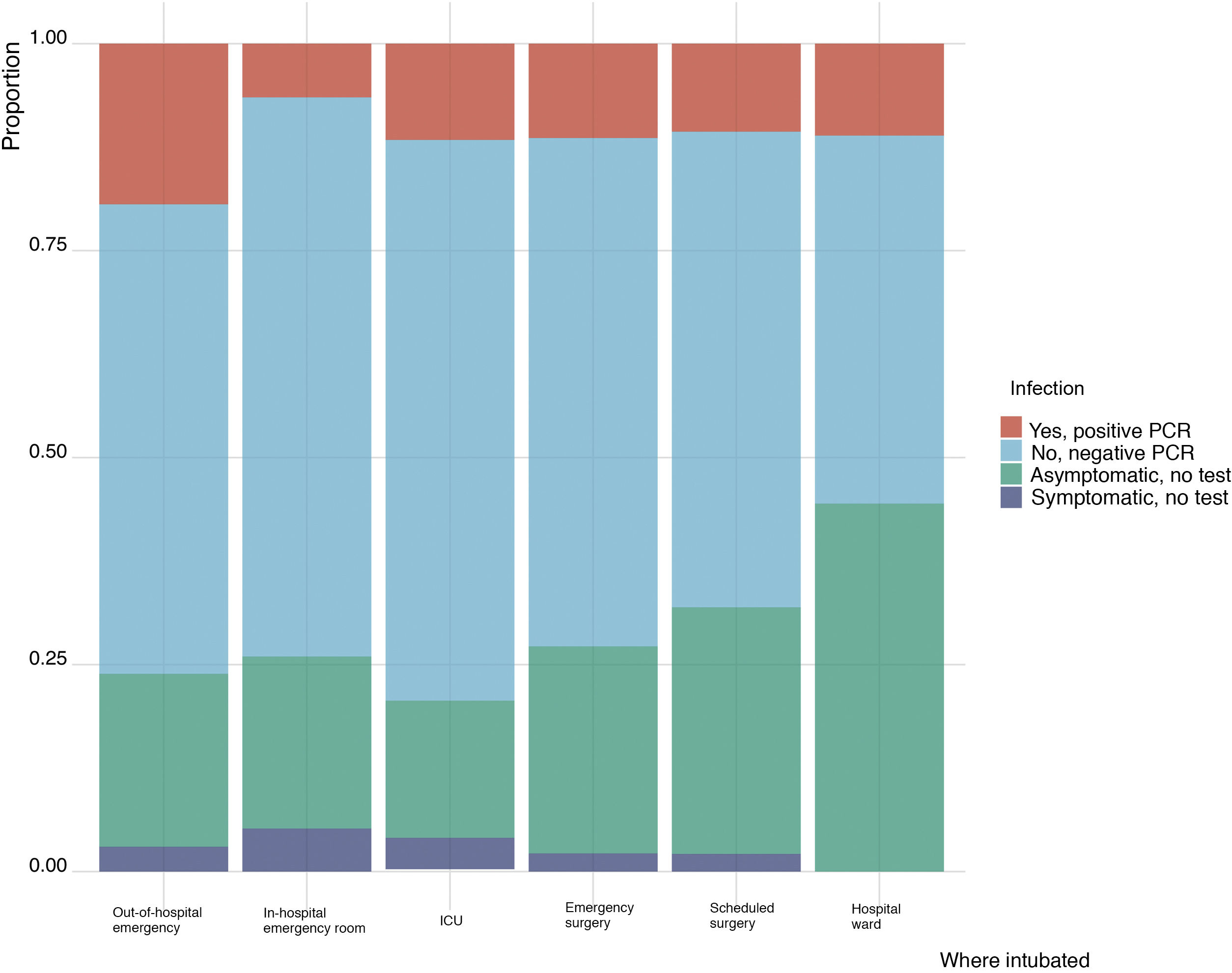
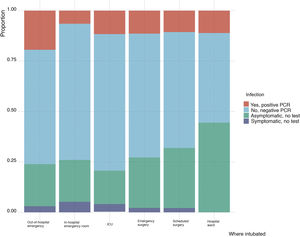
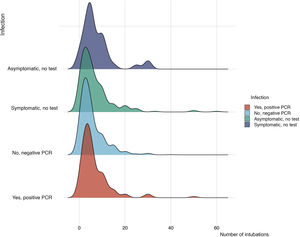
Regarding the risk of cross infection between patients and healthcare workers (Table 1), 862 physicians (76.6%) had undergone PCR testing for SARS-CoV-2 infection, which was positive in 131 cases (11.6%). Ambulance service personnel intubating patients with COVID-19 (Fig. 2) presented a statistically higher incidence of positive PCR; however, the number of intubations performed was not correlated to the frequency of COVID-19 infection (Fig. 3).
Regarding intubation in the hospital emergency department (ED) (n = 77), 4 tracheal intubations were performed per specialist (4 [3]) (Tables 5–7). Most (70%) tracheal intubations were performed by anaesthesiologists, and 30% by emergency specialists. Pre-oxygenation was applied for more than 3 min by 78% of respondents, and for less than 1 min by 9%. Pre-oxygenation was impossible in 13% of cases, due either to the patient’s status or to stressful circumstances. Video laryngoscopy was used in 61% of intubations, and the most widely-used video laryngoscope was the C-MAC (19.5%). Disposable blades were preferred (79.2%) and most widely-used (63.6%). Two physicians were present in 64.9% of intubations and 55.8% had Sometimes forgotten a safety step. According to most respondents, the most stressful situations were fear of intubation failure or deterioration of patient status.
Regarding the Ambulance/Outpatient Emergency Service area (n = 67), 3 tracheal intubations were performed per specialist (3 [2]); 97% of these respondents worked exclusively in out-of-hospital emergencies. Pre-oxygenation was applied for more than 3 min by 47% of respondents, and for less than 1 min by 12%. Pre-oxygenation was impossible in 41% of cases. Direct laryngoscopy was used in 90% of intubations. In 69% of cases, a video laryngoscope was not available. Disposable blades were preferred (84%) and most widely-used (51%). Only 1 physician was involved in 50% of intubations. Half of the respondents (51%) had sometimes forgotten a safety step, and 44% claimed that Fear of contagion was the most stressful situation. The incidence of COVID-19 infection was statistically higher among emergency medicine specialists (15.6%) and doctors working in the ambulance service (17.5%) compared to specialists who intubated patients in the hospital emergency area (6.5%), as shown in Tables 5–7.
DiscussionIn a systematic review of aerosol-generating procedures and the risk of transmission of acute respiratory infections, tracheal intubation was identified as the most high-risk technique7. Tracheal intubation also exposes healthcare workers to a high viral load and, therefore, more serious infection8. The World Health Organization has defined a series of aerosol-generating medical procedures9, but some authors consider this list to be outdated in the context of COVID-19. Many of the procedures defined as aerosol generating may pose a risk because they generate coughing, and bronchoscopy and physiotherapy would probably fit this description10.
During an epidemic, each patient can be considered a potential source of infection, and all airway/respiratory system interventions may need to be treated as high-risk11. In our survey, 862 of respondents who participated in airway management procedures underwent diagnostic tests (76.6%), which were negative in 65.1% of cases. In our survey, the infection rate found among professionals involved in intubation and airway management was 11.6%, which is in line with previous studies. However, at the time of the survey, COVID-19 screening of healthcare workers was basically limited to symptomatic individuals, probably because the healthcare service lacked the capacity to test all physicians involved in intubating COVID-19 patients. This means that the incidence observed in our survey may be underestimated, as many asymptomatic physicians were not evaluated.
The infection rate was higher among ambulance service personnel. Out-of-hospital airway management differed from in-hospital airway management, but we cannot confirm whether this is one of the reasons for the higher incidence of COVID-19 cross-infection among ambulance patients and physicians. However, no significant relationship was found between the number of intubations performed and the probability of being infected by SARS-CoV-2.
In terms of measures to prevent aerosol formation, respondents highly recommended performing rapid sequence induction, avoiding manual ventilation prior to intubation, and maintaining a good face mask seal. This is in line with other studies that also recommend avoiding cough-generating manoeuvres12–14. The methods least recommended by respondents were the Sellick manoeuvre, probably because it can hinder tracheal intubation15,16, and the use of aerosol boxes - probably because placing the device prolongs intubation, and there is a risk of breaking the protective seal.
The video laryngoscope was the preferred and most widely-used intubation device in COVID-19 patients, as reported in other studies17. This was also the most highly recommended device in previous studies in airway management in COVID-19 patients and in SEDAR protocols, since in other clinical situations it has been shown to improve visualisation of the glottis, reduce the time to successful intubation, increase the first attempt intubation success rate, increase the overall intubation success rate, reduce the need for force, and reduce intubation-related complications11,12. According to some authors, proficiency with videolaryngoscope is unlikely to be achieved if their use remains limited to predicted or unpredicted difficult intubation, and acquiring expertise in videolaryngoscopy will require frequent rather than occasional use of the device, both in operating rooms and in ICUs12. Although the availability of all types of video laryngoscopes was not specified in the questionnaire, the 3 most widely-used types of video laryngoscopes were Airtraq, C-MAC, and Glidescope. McGrath and King Vision were the least used, and a statistically significant difference was observed between preferred devices among senior and junior operators.
The 3 preferred video laryngoscopes were Glidescope, C-MAC, and Airtraq. Respondents also showed a greater preference for videolaryngoscopes with a separate screen, which enables the operator to stand further from the airway11,18.
The disposable video laryngoscope blade was both the most preferred and the most widely-used blade, although the percentage of use was lower than that of preference, probably due to the unavailability of this type of blade in some hospitals. This type of disposable blade has also been highly recommended by other authors11,12. Regarding the curvature of the blade used, the Macintosh curved video laryngoscope blade was preferred over the hyper-curved blade. In line with other studies, the most widely recommended intubation aid was the Frova introducer19. The technique of combining a video laryngoscope with an introducer/bougie has also been suggested by other authors2, and is associated with an intubation success rate of close to 98%20. Respondents were in favour of using a flexible stylet inside the orotracheal tube. Other authors have reported that the use of the flexible stylet inside the tracheal tube at an angle of 60° gave faster tracheal intubation21. The least used device was the fibreoptic bronchoscope, which is also consistent with recommendations against using this device due to the risk of generating aerosols14.
The choice of intubation device did not differ significantly between older and younger operators, showing that more experienced physicians are also interested in using the latest optical devices. According to 70.8% of respondents, 2 or more clinicians are usually involved in intubating patients during the COVID-19 pandemic. According to other authors17, the presence of 2 or more clinicians during tracheal intubation is safer for both the patient and the medical team.
An interesting finding of our survey was the correlation between the use of PPE and non-compliance with safety measures. Respondents considered PPE to be very uncomfortable, and tracheal intubation was more difficult when wearing PPE. Some authors have reported difficulties in achieving PPE compliance and in training healthcare workers to correctly prepare and don PPE22. According to other studies, first-attempt intubation success rate with direct laryngoscopy or video laryngoscope is 96% without PPE and 58% when PPE is used20.
In our opinion, based mainly on the results obtained from this survey of Spanish doctors involved in the intubation of COVID-19 patients during the first wave of the pandemic in Spain, pre-oxygenation manoeuvres and aerosol generation reduction strategies, such as rapid sequence induction, avoiding manual ventilation prior to intubation, and proper face mask sealing, are extremely important. We also believe it is advisable to use a video laryngoscope with a disposable blade and separate screen, and to facilitate intubation by using the Frova introducer or flexible stylet. Finally, it is far more uncomfortable and difficult to perform tracheal intubation while wearing PPE.
This study has some limitations. As the survey was promoted by SEDAR, most respondents were anaesthesiologists who are usually experts in airway management using different advanced airway devices. Several patients intubated on an outpatient basis had a suspected diagnosis of SARS-CoV-2 infection, but the definitive diagnosis was made later. In the questionnaire, the item enquiring about preference for disposable over reusable video laryngoscopy blades did not include “I have no experience”.
ConclusionsSpanish physicians involved in orotracheal intubation in patients with COVID-19 consider preoxygenation, aerosol generation reduction manoeuvres such as rapid sequence induction, avoidance of manual ventilation before intubation, and good face mask sealing to be essential for safe intubation. Respondents also believed the video laryngoscope with a separate screen and disposable blade, and the Frova introducer or flexible stylet to be very useful and safe tools. Most respondents thought that intubation should be performed by at least 2 experts wearing PPE, following safety standards. However, there is a certain discrepancy between respondents’ preference for disposable videolaryngoscope blades (86.4%) and their actual use (59.4%), which could well be due to the limited availability of these devices during the first wave of the pandemic in Spain.
Finally, the discomfort of performing intubation while wearing PPE was a common cause of non-compliance with some safety steps, and could increase the risk of cross infection between patients and healthcare workers. Therefore, in our opinion, urgent measures are needed to improve these weak points and optimise the protection of at-risk healthcare workers.
We believe further research is required to determine why the incidence of COVID-19 infection is higher among emergency doctors treating patients with suspected or confirmed COVID-19 infection who work under stress with limited airway management equipment. The infection rate among healthcare workers may be underestimated, since many asymptomatic physicians working in the hospital or ambulance service were not systematically tested for COVID-19 infection.
Conflict of interestsThe authors have no conflict of interest to declare.
Ferrer Gómez C, Durá Navarro R, Moliner Velázquez S, Bosch Velázquez M, Casanova Montes I, Muñoz Devesa L, Vergara Sánchez A, López Palanca S, Morales Sarabia J, Errando Oyonarte C, Vicente Fernández P, Peiró Alós CM, Briones Través A, Lacoste O y Aisa Gasca I (Consorci Hospital General Universitari de València, València); Esturi Navarro R y Sánchez García F (Hospital Universitario de la Ribera, València); Beltrán Alandí RA (Hospital de Lliria, Valéncia); Lorente García PJ (Hospital General Universitari de Castelló, Castelló); Serrano Alonso J (Hospital Vithas Rey Don Jaime, Castelló); Argente Navarro P, Vicente Guillén R, Pajares Moncho A, Aparicio Chagoyen R, Ferrer Colomer A, Carmona García P, y Pons Frigola A (Hospital Universitari i Politècnic La Fe, València); Parra González MJ, Tornero Tornero C, y Casterá Brugada MA (Hospital Clínic Universitari de València, Valéncia); Bueno Latorre N y Herrera de Pablo P (SAMU Valéncia); Cruz Pardos P, Portas González M, de Miguel Guijarro A, Barrio Saiz E, Vera Blas M, Rubio Murias P, y González Carranza JE (Hospital General Universitario Gregorio Marañón, Madrid); González Perrino C (Hospital Clínico San Carlos, Madrid); Valencia Orgaz O, García Gutiérrez AF, Adriana Calderón Z, y Real Navacerrada MI(Hospital Universitario 12 de Octubre, Madrid); Garrido Ortega P, Caldera Álvarez MV, Menéndez Gallego JA, Uña Orejón R, y Ruiz López JJ (Hospital Universitario La Paz, Madrid); Planas Roca A y Ramasco Rueda F (Hospital Universitario de la Princesa, Madrid); Abad Gurumeta A (Hospital Infanta Leonor, Madrid); Canales Corcho I, Horrillo García C, y Serrano Moraza A (SUMMA, Madrid); Almagro Vidal I (Hospital Gómez Ulla, Madrid); Valero Castell R, Ubré Lorenzo M, Bergé Ramos R, Belda Tortosa I, Perdomo Linares JM, Jacas A, y Angelès Fité GS (Hospital Clínic, Barcelona); Fábregas Blanco I y Vitale S (Consorci Sanitari del Maresme, Barcelona); Caldentey Sierra J (Hospital Universitari Vall d’Hebron, Barcelona); Roig Pineda R y Tolós París R (Hospital Universitari Germans Trias i Pujol, Badalona, Barcelona); Bermejo S y Gallart Gallego Ll (Hospital del Mar-Parc de Salut Mar, Barcelona); Marín Posada PA, Miró Bernié G, y Vives Santacana M (Hospital Universitari de Girona Doctor Josep Trueta, Girona); Sánchez López A, López-Torres López J, y de Capadocia Rosell J (Complejo Hospitalario Universitario de Albacete, Albacete); Sánchez Andrés A y Gallego Ligorit L (Hospital Universitario Miguel Servet, Zaragoza); Pastor Marcos D (Hospital Universitario Lucus Augusti, Lugo); Callado Moro FJ (Hospital Universitario de Burgos, Burgos); Hernández Martínez A (Grupo Policlínica, Ibiza); Mora Fernández C y Brogi L (Hospital Universitari Son Espases, Palma); Malo Manso A (Hospital Universitario Virgen de la Victoria, Málaga); González-Delgado A (Clínica Universidad de Navarra, Pamplona); Pernia Romero A y Torres Morera LM (Hospital Universitario Puerta del Mar, Cádiz); Cortiñas Díaz J, del Río Fernández S, y Prada Hervella G (Hospital Clínico Universitario de Santiago, Santiago de Compostela), España; and Echeverría J (University Hospitals Coventry and Warwickshire NHS Trust, Coventry), UK.
The names of the components of the COV2-VIAEREA Network Study Group are listed in the Appendix A.
Please cite this article as: Granell Gil M, Sanchís López N, Aldecoa Álvarez de Santulano C, de Andrés Ibáñez JA, Monedero Rodríguez P, Álvarez Escudero J, et al. Manejo de vía aérea en pacientes COVID-19: una encuesta sobre la experiencia de 1125 médicos en España. Rev Esp Anestesiol Reanim. 2022;69:12–24.