Perioperative SARS-CoV-2 infection has been associated with increased postoperative mortality.1 This led to the cancellation of a multitude of elective surgical procedures during the Covid-19 pandemic due to lack of resources and concerns about adverse patient outcomes and the risk of nosocomial transmission.2 However, the risk of SARS-CoV-2 infection in children undergoing surgery is poorly understood. Over the past 2 years, the SARS-CoV-2 pandemic has compelled clinicians to constantly update their protocols, decision strategies, and clinical management guidelines, including the recommendation to screen patients prior to surgical procedures. Paediatric anaesthesiologists initially followed the same pre-surgical screening recommendations established for adult patients. Our hospital was no exception. But in March 2020, the Health Department of the Community of Madrid centralised paediatric emergency care, intensive care, and hospital admissions to the La Paz Hospital and in the Hospital Infantil Universitario del Niño Jesús.3 For this reason, preoperative SARS-CoV rRT-PCR tests were performed on all patients undergoing scheduled and urgent surgery between April 2020 and April 2022. The national and regional health authorities recommended postponing elective surgery in patients infected with SARS-CoV-2 to prevent potential pulmonary complications and transmission among hospital staff.
To date, studies on perioperative outcomes in paediatric patients with SARS-CoV-2 infection involving over 13,000 cases have been published. Children with perioperative SARS-CoV-2 infection do not appear to have an increased risk of postoperative pulmonary complications or mortality, and therefore delay in surgery appears to be unnecessary.4
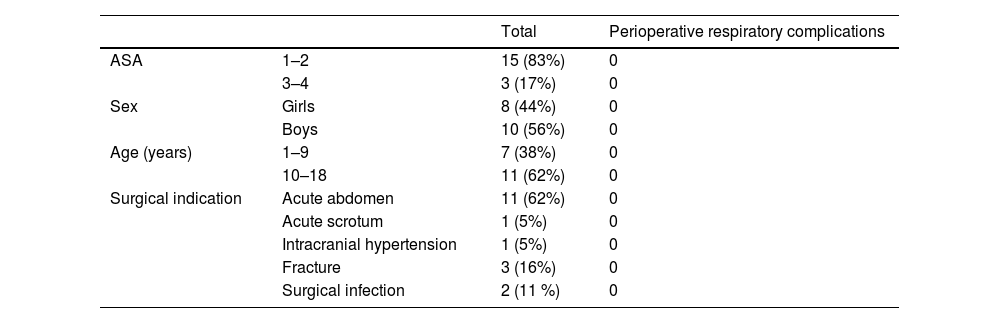
According to data provided by our hospital’s Admission Service, of the total number of patients operated on in this period, 18 had to undergo urgent surgery despite active SARS-CoV-2 infection. As shown in Table 1, the surgical indications were: appendectomy (11), upper limb fracture (3), ventriculoperitoneal shunt (1), surgical wound cleaning (1), sinus drainage (1) and acute testicular torsion (1). Fifteen of these patients were ASA (American Society of Anesthesiology) I–II and 3 were ASA III, the latter corresponding to a child with a pineal gland tumour, a child with DMID, and a child with spinal atrophy. We reviewed the perioperative evolution of all these patients, and found that none, including the ASA III patients, presented respiratory complications in either the intra- or postoperative period (pneumonia, need for mechanical ventilation, or acute respiratory distress syndrome). Our experience is consistent with that reported in other series, i.e., children with perioperative SARS-CoV-2 infection do not appear to be at increased risk of postoperative pulmonary complications, and delaying urgent surgery appears unnecessary.
Children operated on with a diagnosis of preoperative SARS-CoV-2 infection.
| Total | Perioperative respiratory complications | ||
|---|---|---|---|
| ASA | 1–2 | 15 (83%) | 0 |
| 3–4 | 3 (17%) | 0 | |
| Sex | Girls | 8 (44%) | 0 |
| Boys | 10 (56%) | 0 | |
| Age (years) | 1–9 | 7 (38%) | 0 |
| 10–18 | 11 (62%) | 0 | |
| Surgical indication | Acute abdomen | 11 (62%) | 0 |
| Acute scrotum | 1 (5%) | 0 | |
| Intracranial hypertension | 1 (5%) | 0 | |
| Fracture | 3 (16%) | 0 | |
| Surgical infection | 2 (11 %) | 0 |
After the recommendations for detecting active COVID-19 infection prior to hospitalisation, diagnostic testing, and surgery were published in March 2022, our protocols were updated and rRT-PCR for SARS-CoV-2 was no longer requested in all patients prior to diagnostic and/or therapeutic tests and surgical procedures. In paediatric patients, the perioperative risk is determined by the symptoms of active infection, and on this basis the surgical team may consider cancelling and rescheduling the procedure.
In conclusion, this is yet another example of the need to adapt perioperative care to paediatric patients. Hospitals have already reduced the number of routine preoperative laboratory tests, and this strategy should be extended to systematic rRT-PCR screening for SARS-CoV-2, which can cause unnecessary surgery delays, add to the burden of already overloaded laboratory services, and increase care costs. Finally, we remind our colleagues of the importance of maintaining personal protective measures to reduce the risk of transmitting nosocomial infections.
FundingThis work has not been funded.
Conflict of interestsThis work does not imply any conflict of interest on the part of the authors.