To analyze initial and follow-up features of patients with systemic lupus erythematosus (SLE) diagnosed during hospitalization.
MethodsRetrospective analysis of medical records: two groups were studied, a) SLE diagnosed during hospitalization (SLEin), b) SLE diagnosed on an outpatient basis (SLEout).
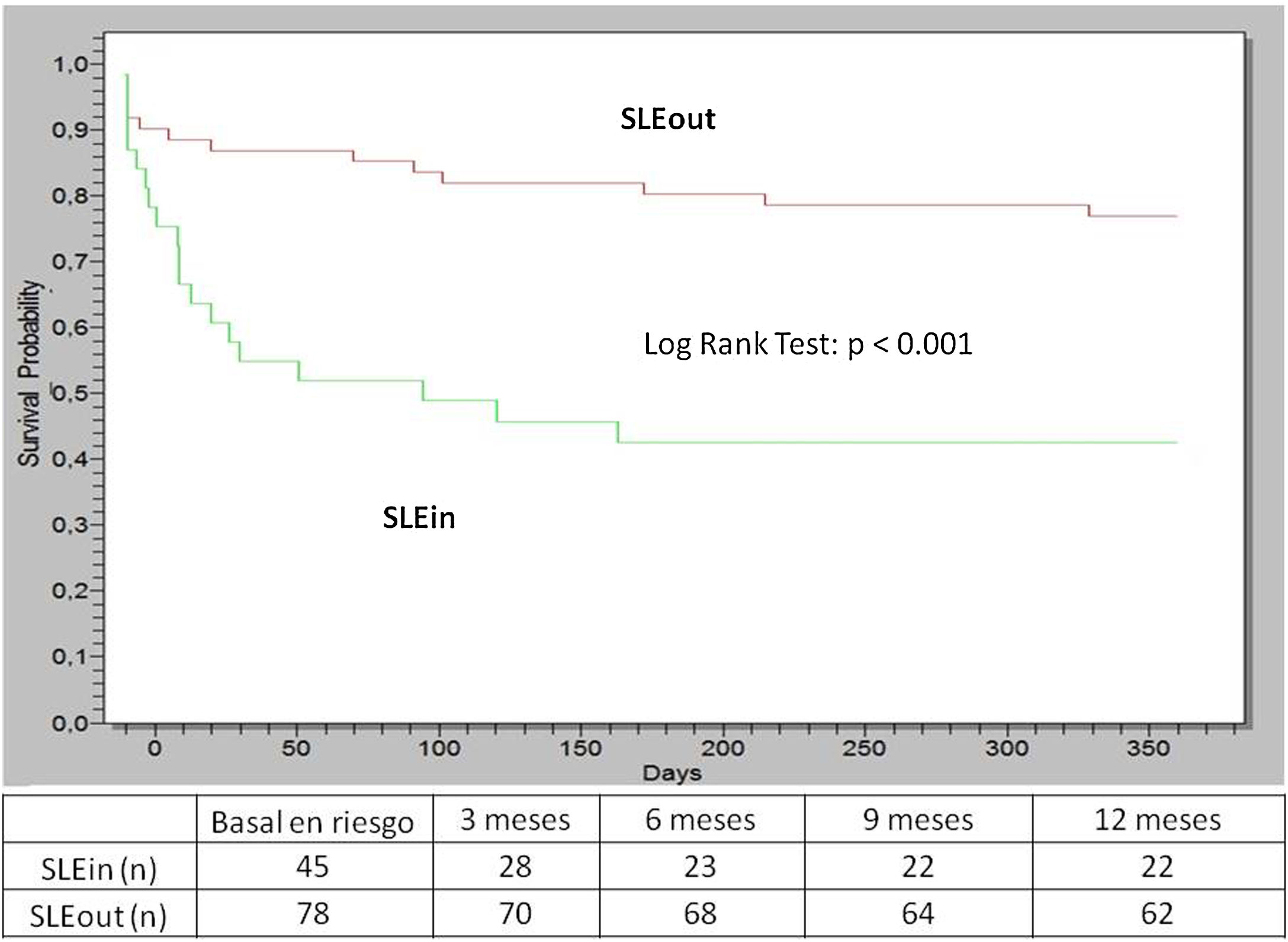
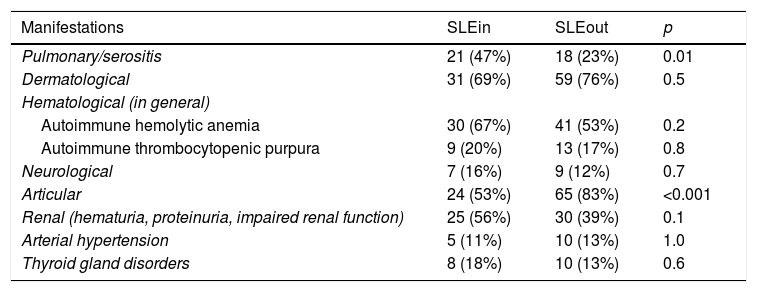
Results123 patients were assessed, 87% female, mean age at diagnosis was 34 years and 45 (37%) of them were SLEin. Patients in the SLEin group had a median of 144 days from the onset of symptoms to diagnosis of SLE vs. 287 days in the SLEout group (p = 0.04). Initially, SLEin had an average SLEDAI of 10 vs. 8 in SLEout (p = 0.004) and anti-dsDNA was positive in 71% vs. 53% in SLEout (p = 0.07). Within the first 6 months, the average cumulative glucocorticoid dose was 6493 mg in SLEin patients vs. 3563 mg in SLEout (p < 0.001) and immunosuppressant usage was higher in SLEin: 62% vs. 26% in SLEout (p < 0.001). Within the first year, SLEin’s kidney biopsies showed lupus nephritis III or IV in 31% vs. 12% in SLEout (p = 0.003, log-rank test). Within the first 2 years, 6 SLEin patients died vs. 1 SLEout patient (p = 0.02) and SLEin patients had more damage as measured by SLICC/ACR Damage Index (median 0, range 25%–75% 0–1 vs. median 0, range 25%–75% 0–0 in SLEout; p = 0.04).
ConclusionsSLEin are initially more active, require higher doses of glucocorticoids and immunosuppressants, have more significant kidney involvement, and present more damage and greater mortality in the short term.
Analizar las características de los pacientes con lupus eritematoso sistémico (LES) diagnosticados durante una hospitalización.
MétodosAnálisis retrospectivo de historias clínicas. Se estudiaron dos grupos: a) LES diagnosticado durante la hospitalización (SLEin) y b) LES diagnosticado de forma ambulatoria (SLEout).
ResultadosSe evaluaron 123 pacientes (87% mujeres); edad promedio al diagnóstico 34 años; el 37% de ellos era SLEin. Los pacientes del grupo SLEin tuvieron una mediana de 144 días desde el inicio de los síntomas hasta el diagnóstico, vs. 287 días en SLEout (p = 0,04). Inicialmente, los pacientes SLEin tenían un SLEDAI promedio de 10, vs. 8 en SLEout (p = 0,004) y anti-dsDNA positivo en el 71%, vs. el 53% en SLEout (p = 0,07). A los 6 meses, la dosis acumulada de glucocorticoides (promedio) fue de 6.493 mg en SLEin vs. 3.563 mg en SLEout (p < 0,001), y el uso de inmunosupresores fue mayor en SLEin: 62% vs. 26% en SLEout (p < 0,001). Al año se halló nefritis lúpica clase III o IV en el 31% de SLEin vs. el 12% en SLEout (Log Rank Test: p = 0,003). A los 2 años, 6 pacientes de SLEin murieron, vs. un paciente de SLEout (p = 0,02). Los pacientes con SLEin tuvieron más daño (índice de daño SLICC/ACR: mediana 0, rango 25–75%: 0-1, vs. mediana 0, rango 25–75%: 0–0 en SLEout; p = 0,04).
ConclusionesLos pacientes SLEin fueron inicialmente más activos, requirieron mayores dosis de glucocorticoides e inmunosupresores, tuvieron una afectación renal más significativa y presentaron más daño y mayor mortalidad a corto plazo.