Our study was planned to investigate the effect of Clinical Pilates exercises in children and adolescents with Juvenile Idiopathic Arthritis (JIA).
MethodsFifteen participants diagnosed with JIA (mean age=12.00±3.40 years) were included. The participants were randomly divided into two groups as Clinical Pilates exercise group (n=6), and home exercise group (n=9). Clinical Juvenile Arthritis Disease Activity Score (cJADAS), Wong Baker Face Scale, Brunininks-Oseretsky Test of Motor Proficiency Second Edition Short Form (BOT-2 SF), Juvenile Arthritis Biopsychosocial Scale (JAB-Q scale), and Pediatric Quality of Life Inventory (PedsQL) 3.0 Arthritis Module was used for evaluation before and after treatment. Exercises were performed by both groups 3 times a week for 6 weeks.
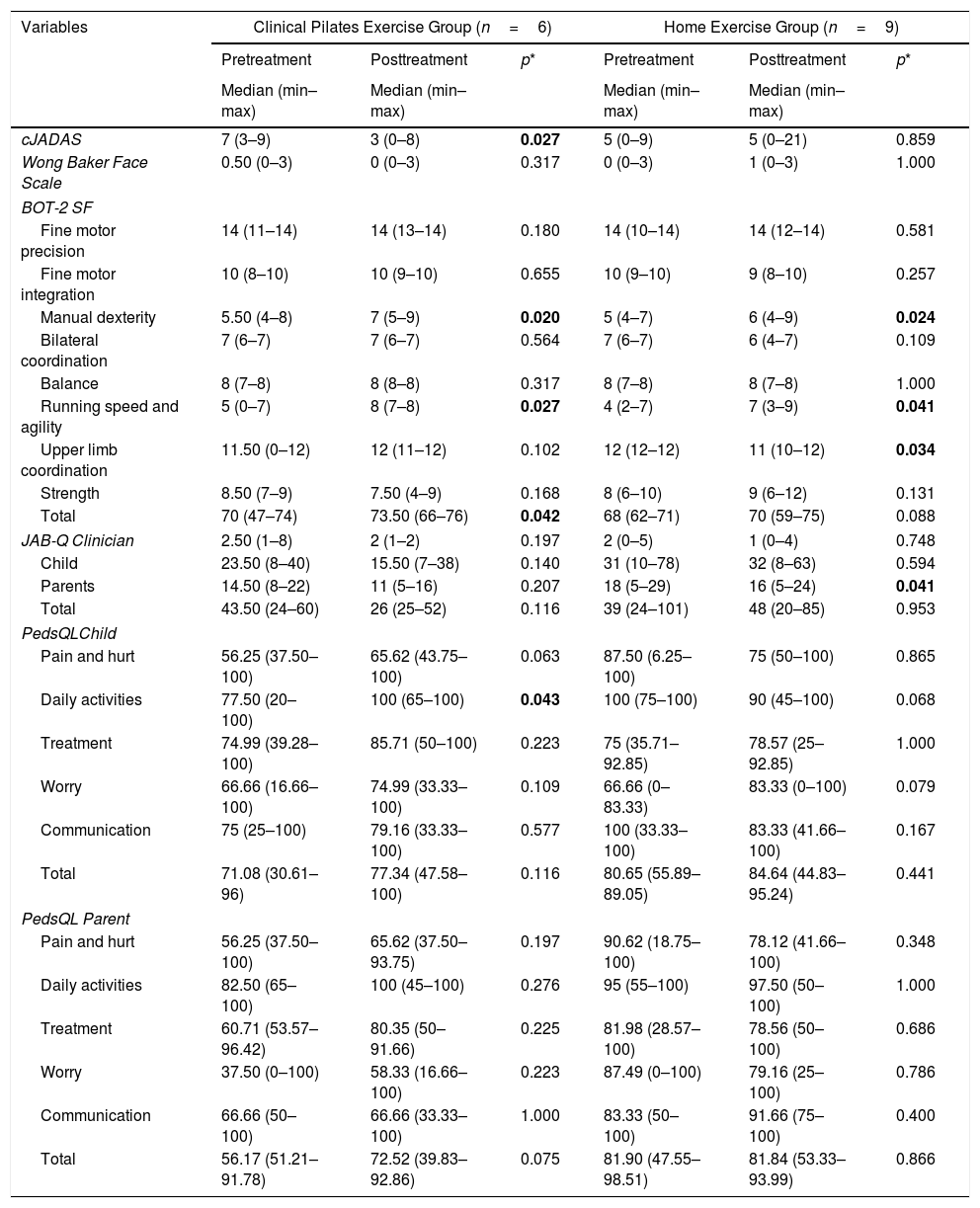
ResultsIn the analysis of the before and after treatment results, a significant difference was observed in cJADAS (p=.027), manual dexterity (p=.020), running speed and agility (p=.027) subtests of BOT-2 SF, total score of BOT-2 SF (p=.042) and daily activity (p=.043) subtests of PedsQL child form in the Clinical Pilates exercise group. While there was statistically significant differences in manual dexterity (p=.024), running speed and agility (p=.041) and upper limb coordination (p=.034) subtests of BOT-2, and parent form of JAB-Q (p=.041) in home exercise group. When the delta values were compared, the difference was significant in the upper limb coordination subtest of BOT-2 SF (p=.008), and daily activities subtest of PedsQL child form (p=.003) in favour of the Clinical Pilates exercise group.
ConclusionsClinical Pilates exercises are a safe and useful method for children/adolescent with JIA.
Nuestro estudio fue planeado para investigar el efecto de los ejercicios de pilates clínico en niños y adolescentes con artritis idiopática juvenil (AIJ).
MétodosSe incluyeron 15 participantes diagnosticados con AIJ (edad media=12,00±3,40 años). Los participantes fueron divididos al azar en 2 grupos como grupo de ejercicio de pilates clínico (n=6) y grupo de ejercicio en el hogar (n=9). Para la evaluación antes y después del tratamiento se utilizó la puntuación de actividad de la artritis juvenil clínica (cJADAS), la escala Wong-Baker FACES®, la prueba Brunininks-Oseretsky de proficiencia motora en su segunda edición (BOT-2 SF), la escala biopsicosocial de artritis juvenil (escala JAB-Q) y el inventario de calidad de vida pediátrica (módulo PedsQL® 3.0) de artritis. Se realizaron ejercicios a ambos grupos, 3 veces por semana, durante 6 semanas.
ResultadosCuando se analizaron los resultados, antes y después del tratamiento, se observó una diferencia significativa en las subpruebas de cJADAS (p=0,027), destreza manual (p=0,020), velocidad y agilidad en la carrera (p=0,027) de BOT-2 SF, puntuación total de BOT-2 SF (p=0,042) y actividad diaria (p=0,043) subpruebas de PedsQL® forma infantil en el grupo de ejercicio de pilates clínico, mientras que hubo una diferencia estadísticamente significativa en la destreza manual (p=0,024), la velocidad y la agilidad en la carrera (p=0,041) y la coordinación de las extremidades superiores (p=0,034) subpruebas de BOT-2 SF y forma parental de JAB-Q (p=0,041) en el grupo de ejercicio en casa. Cuando se compararon los valores delta, la diferencia fue significativa en la subprueba de coordinación de los miembros superiores de BOT-2 SF (p=0,008) y en la subprueba de actividades diarias de la forma infantil de PedsQL® (p=0,003) a favor del grupo de ejercicio de pilates clínico.
ConclusionesLos ejercicios de pilates clínico son un método seguro y útil para niños/adolescentes con AIJ.
Juvenile Idiopathic Arthritis (JIA); is a chronic autoimmune disease of unknown origin with arthritis in one and/or more joints for at least 6 weeks before the age of sixteen.1 JIA is chronic arthropathy with the highest prevalence in children and adolescents.2
Arthritis, pain, muscle weakness, functional novelties and inactivation are the most important problems in children with JIA. Pain, as with other rheumatic diseases, is one of the symptoms causing disability in JIA.3,4 It is stated that physical activity deficiency due to pain over time leads to fatigue, loss of function and motor control disorders.5 It is known that increasing physical activity is necessary for normal muscle and joint health and can provide protection against inflammatory conditions.6
Children and adolescents with JIA have been reported to be at risk from a psychosocial perspective as well as physical deficiencies.7,8 Since JIA gives different clinical findings, it is emphasized that the physical therapy and rehabilitation model to be applied should be holistic. In the biopsychosocial model, which has been focused on since the 1970s, a holistic approach is adopted to address the mind-body and spirit triad of the patient. Clinical pilates exercises are examples of this area. The foundations of Pilates were laid by the merger of theories of mind-body-spirit with theories of motor learning and core stabilization.7,9
Clinical Pilates exercises, which are preferred as a biopsychosocial approach in the exercise choices of adult rheumatic patients, are also fun for the JIA population, make the child active, can be done in groups and exercise habit, such as the role of positive characteristics will be considered appropriate.10
In the literature two studies examining the effectiveness of pilates exercises in children and adolescents with JIA have been found.10,11 In these studies show that, Pilates exercises can be considered as a reliable model and provides a positive physical and psychosocial effects in children with JIA and should be supported in future studies with more objective parameters.
Many studies with adult individuals have shown the antiinflammatory effects of regular exercise.12 Although, these studies have not been done in children with JIA, prevailing opinion is exercise will have similar effects in children as adults.13
Our study was planned and performed to investigate the effect of Clinical Pilates exercises on disease activity, pain, motor skills, psychosocial status and quality of life in children and adolescents with JIA.
Material and methodOur study was planned as a randomized controlled parallel group and the effects of Clinical Pilates exercise in children/adolescents with JIA were evaluated by comparison with the control group. Participants were randomly divided into Clinical Pilates exercise and home exercise groups. The Clinical Pilates exercises were conducted under the supervision of a physiotherapist. The participants in the home exercise group were told in detail about the home exercise program by the same physiotherapist and were asked to do the exercises at home.
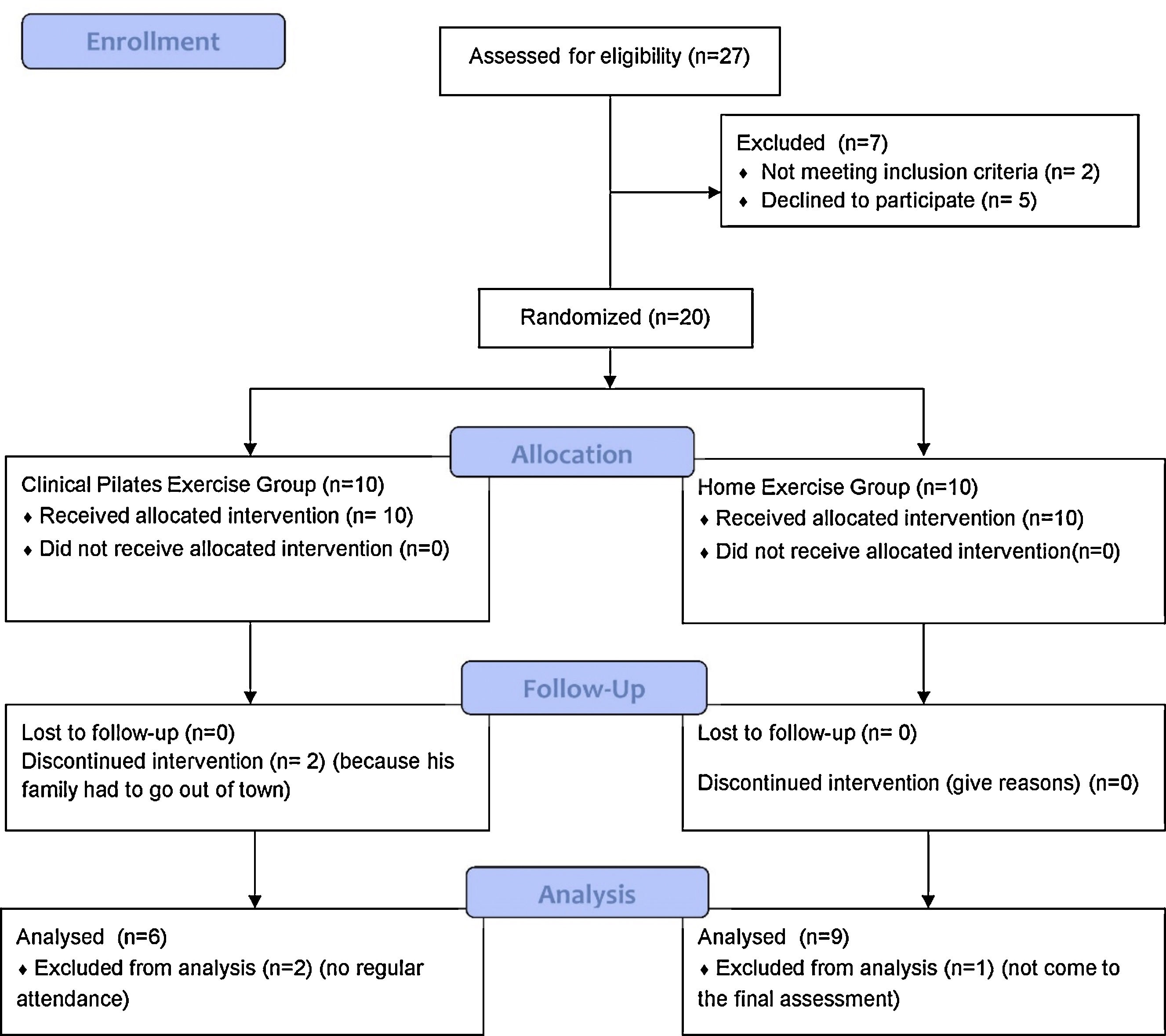
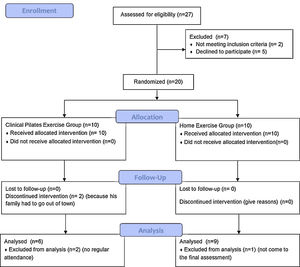
ParticipantsOf the 27 individuals diagnosed with JIA initially included, 2 individuals were excluded from the study due to intraarticularsteroid injection to the knee joint in the last 3 months, and 5 individuals refused to participate in the study. The 20 volunteer individuals who met the inclusion criteria of the study were randomly divided into two groups with the SPSS program: Clinical Pilates exercise group (n=10) and the home exercise group (n=10). From the Clinical Pilates exercise group; 2 individuals had to give up exercise because their family had to move out of the city, 2 individuals were excluded from the study because they did not come to treatment regularly. From home exercise group; 1 individual did not come to the final evaluation because his exam period began. The study was completed with a total of 15 individuals with JIA including 6 individuals (6 girls, mean age=12.50±4.03 years) in Clinical Pilates exercise group and 9 individuals (4 girls, 5 boys, mean age=11.66±3.12 years) in home exercise group. Fig. 1 shows a flow chart of the study design.
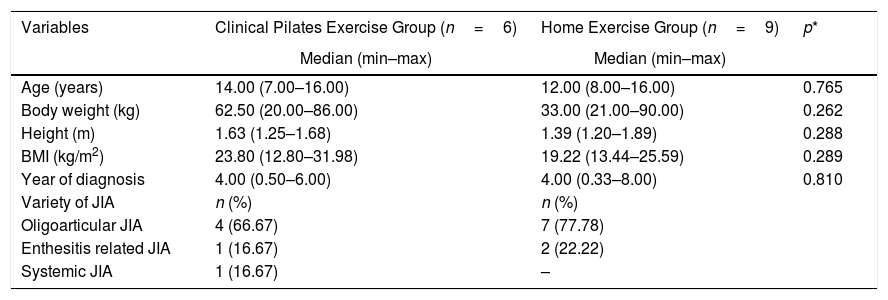
The demographic information of the participants was recorded prior to the evaluations. Demographics are shown in Table 1.
Demographic characteristics of the participants.
| Variables | Clinical Pilates Exercise Group (n=6) | Home Exercise Group (n=9) | p* |
|---|---|---|---|
| Median (min–max) | Median (min–max) | ||
| Age (years) | 14.00 (7.00–16.00) | 12.00 (8.00–16.00) | 0.765 |
| Body weight (kg) | 62.50 (20.00–86.00) | 33.00 (21.00–90.00) | 0.262 |
| Height (m) | 1.63 (1.25–1.68) | 1.39 (1.20–1.89) | 0.288 |
| BMI (kg/m2) | 23.80 (12.80–31.98) | 19.22 (13.44–25.59) | 0.289 |
| Year of diagnosis | 4.00 (0.50–6.00) | 4.00 (0.33–8.00) | 0.810 |
| Variety of JIA | n (%) | n (%) | |
| Oligoarticular JIA | 4 (66.67) | 7 (77.78) | |
| Enthesitis related JIA | 1 (16.67) | 2 (22.22) | |
| Systemic JIA | 1 (16.67) | – |
Inclusion criteria in the study: (a) To be diagnosed with JIA according to ILAR classification. (b) Being in the 6–16 age range. (c) Volunteering to participate in the study. (d) To be stable in drug use for at least 3 months or longer.
Exclusion criteria in the study: (a) Presence of active synovitis or arthritis. (b) The presence of cardiovascular, pulmonary, orthopaedic and neurological problems that may interfere with exercise. (c) Intraarticularsteroid injections to the knee and ankle joint in the last 3 months. (d) Having been exercising regularly for the last three months. (e) Having undergone any surgical operation in the last six months. (f) Not being able to participate in at least 75% of the education.
If there were participants of the child/adolescent who could not adapt to the exercise, the exercise would be terminated for these participants and these participants would be followed up in our clinic.
Outcome measuresEvaluations were done before and after the treatment. cJADAS was evaluated by the same rheumatologist blinded to all interventions. All other evaluations were performed by the same experienced physiotherapist blinded to all interventions, according to standardized testing protocols and in the same environment where the same conditions were met.
Demographic data and disease information of the participants were recorded using the face-to-face interview method. Then, disease activity was evaluated with Clinical Juvenil Arthritis Disease Activity Score (cJADAS), pain with Wong Baker Faces scale, motor skill with Brunininks-Oseretsky Test of Motor Proficiency Second Edition Short Form (BOT-2SF), biopsychosocial aspect with clinician, family and child forms of Juvenile Arthritis Biopsychosocial Scale (JAB-Q scale) and disease-related quality of life with Pediatric Quality of Life Inventory (PedsQL) 3.0 arthritis module.
Clinical Juvenil Arthritis Disease Activity Score (cJADAS)In 2009, “Juvenil Arthritis Disease Activity Score (JADAS)” was defined to assess disease activity in children. This scale consists of 4 sections: Doctor-Visual Analog Scale, Patient-Visual Analog Scale, number of active joints (71, 27, 10 joints) and evaluation of sedimentation between 0 and 10. Recently, Mc Erlane et al. developed a clinical three-point version of the score that excludes ESR.14 It is called the acronym cJADAS, i.e. clinical JADAS.15 cJADAS which used to evaluate 27 active joints were used in our study.
Wong Baker Face ScaleThis scale is rated between 0 and 10. 0 is the absence of pain, 10 is the most severe pain and the condition of pain is explained by facial expressions in response to numerical data on the scale.16
Brunininks-Oseretsky Test of Motor Proficiency Second Edition Short Form (BOT-2SF)The scale assesses motor skill and consists of 8 subtests and 14 items. Subtests were fine motor precision, fine motor integration, manual dexterity, bilateral coordination, balance, running speed and agility, upper limb coordination, and strength. Motor skill increases as score increases.17
Juvenile Arthritis Biopsychosocial Scale (JAB-Q)This is a questionnaire prepared in Turkish language with JIA children between 6 and 18 years of age in order to evaluate JIA patients biopsychosocially. It has 3 forms: child, parents and clinician. In our study, evaluation was made using this 3 questionnaire forms. The answer to each question is yes/no/sometimes. The “yes” answer to the questions is indicates a bad psychosocial situation.18
Pediatric Quality Of Life Inventory (PedsQL) 3.0 Arthritis ModuleThe PedsQL 3.0 arthritis module includes subtests; “Pain and Hurt “(4 items),” Daily activities “(5 items),” Treatment “(7 items),” Worry “(3 items), and” Communication” (3 items). It consists of a total of 22 items. High scores mean high quality of life. In this study, 5–7 years old, 8–12 years old, 12–18 years old child and parent forms were used to evaluate the quality of life of the patients.19,20
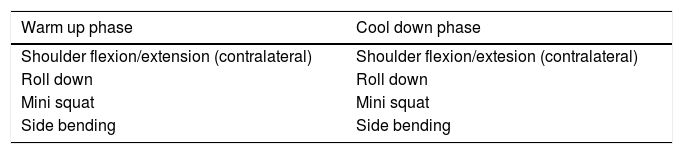
InterventionClinical Pilates ExercisesClinical Pilates training was performed 3 times a week for 6 weeks by a physiotherapist trained in clinical mat pilates and experienced in the field. Each session was contain 10min of warm-up phase, 40min of Clinical Pilates exercises and 10min of cool down phase. Before starting the clinical pilates program, a 1-hour meeting session was held to allow participants to meet each other and to have parents know about Clinical Pilates. After the meeting session, participants were taught 5 key elements of Clinical Pilates and the program was started. These key elements; respiration, focus, rib cage placement, shoulder placement, head and neck placement. Participants were encouraged to use these 5 basic elements not only during exercises but also in daily routines. It was aimed to create awareness by explaining the neutral spine position to each participant by using age-appropriate imagery methods. In addition, participants were taught the Pilates resting position before beginning to exercises. Throughout the Clinical Pilates training, exercises were repeated until correct posture was achieved in different positions in line with the elements taught on the first day. For the correct implementation of exercises, the physiotherapist did the clinical pilates exercises and asked the participants to do. In addition, the aim of each exercise was explained to the participant and it was tried to make it functional in daily life. Each exercise for the first three weeks was performed 8–10 repetitions. The exercises were performed on the mat in supine, side-lying, prone and sitting positions, respectively. The next 3 weeks, increase in the number of repetitions, a change of position to suit the level, and stabilization balls were used to for advance the exercises. Each participant's stabilization ball was personalized and 55 or 65cm in height, so as to achieve 90° flexion angle on the hips and knees.21 The details of the Clinical Pilates exercises are given in Table 2.
The details the Clinical Pilates treatment program.
| Warm up phase | Cool down phase |
|---|---|
| Shoulder flexion/extension (contralateral) | Shoulder flexion/extesion (contralateral) |
| Roll down | Roll down |
| Mini squat | Mini squat |
| Side bending | Side bending |
| Clinical pilates exercises (0–3weeks) | (3–6 weeks) |
|---|---|
| One leg stretch | Hundreds with stabilization ball |
| Scissors | Double Leg Stretch |
| Shoulder bridge | Leg Push with stabilization ball |
| Hip twist | Shoulder bridge/level 2 |
| Arm openings | Hip twist/level 2 |
| Clam | Arm openings/level 2 |
| Swimming | Clam/level 2 |
| One leg kick | Shoulder Bridge 1 with stabilization ball |
| Side kick in Lying (beginner) with stabilization ball | |
| One Leg Kick with stabilization ball | |
| Swimming 1 with stabilization ball |
A total of 12 exercises were applied to the home exercise group, consisting of stretching and strengthening exercises for the whole body, which lasted approximately 40min for 6 weeks, including 3 times a week. In patients who were eligible to participate in the study after the initial evaluation, a session was conducted together and the accuracy of movement were taught. The brochure which containing the names and descriptions of the exercises with the visual was given to the participant or parent. Follow-up of patients was provided with a home follow-up schedule and reminders were made by contacting parents over the phone. Advanced level exercises were explained to the participants in the first session and on the third week high level exercises started by the phone call.
Statistical analysisThe data was analyzed with the SPSS (version 21.0) package program. Continuous variables were given as median (minimum-maximum) and categorical variables as number and percentage. To compare independent group differences, Mann–Whitney U test was used in accordance with low sample size. Within group comparisons, Wilcoxon test was used in accordance with low sample size. The statistical significance level was considered p<0.05.
ResultsIn our study with 15 participants, no problems were reported during evaluations and training. Our study was completed with 85% continuity. There was no statistical difference between the demographic data of the groups (p>0.05, Table 1).
When before and after treatment data were compared, there was a significant improvement in, cJADAS (p=0.027), manual dexterity (p=0.020) and running speed-agility (p=0.027) subtests of BOT-2 SF, total score of BOT-2 SF (p=0.042) and daily activities (p=0.043) subtest of PedsQL child form in the Clinical Pilates exercise group. In the home exercise group, showed statistically significant differences in manual dexterity (p=0.024), running speed-agility (p=0.041) and upper limb coordination (p=0.034) subtests of BOT-2 SF and parent form of JAB-Q scale (p=0.041) (Table 3).
The comparison of pre and post treatment results within groups.
| Variables | Clinical Pilates Exercise Group (n=6) | Home Exercise Group (n=9) | ||||
|---|---|---|---|---|---|---|
| Pretreatment | Posttreatment | p* | Pretreatment | Posttreatment | p* | |
| Median (min–max) | Median (min–max) | Median (min–max) | Median (min–max) | |||
| cJADAS | 7 (3–9) | 3 (0–8) | 0.027 | 5 (0–9) | 5 (0–21) | 0.859 |
| Wong Baker Face Scale | 0.50 (0–3) | 0 (0–3) | 0.317 | 0 (0–3) | 1 (0–3) | 1.000 |
| BOT-2 SF | ||||||
| Fine motor precision | 14 (11–14) | 14 (13–14) | 0.180 | 14 (10–14) | 14 (12–14) | 0.581 |
| Fine motor integration | 10 (8–10) | 10 (9–10) | 0.655 | 10 (9–10) | 9 (8–10) | 0.257 |
| Manual dexterity | 5.50 (4–8) | 7 (5–9) | 0.020 | 5 (4–7) | 6 (4–9) | 0.024 |
| Bilateral coordination | 7 (6–7) | 7 (6–7) | 0.564 | 7 (6–7) | 6 (4–7) | 0.109 |
| Balance | 8 (7–8) | 8 (8–8) | 0.317 | 8 (7–8) | 8 (7–8) | 1.000 |
| Running speed and agility | 5 (0–7) | 8 (7–8) | 0.027 | 4 (2–7) | 7 (3–9) | 0.041 |
| Upper limb coordination | 11.50 (0–12) | 12 (11–12) | 0.102 | 12 (12–12) | 11 (10–12) | 0.034 |
| Strength | 8.50 (7–9) | 7.50 (4–9) | 0.168 | 8 (6–10) | 9 (6–12) | 0.131 |
| Total | 70 (47–74) | 73.50 (66–76) | 0.042 | 68 (62–71) | 70 (59–75) | 0.088 |
| JAB-Q Clinician | 2.50 (1–8) | 2 (1–2) | 0.197 | 2 (0–5) | 1 (0–4) | 0.748 |
| Child | 23.50 (8–40) | 15.50 (7–38) | 0.140 | 31 (10–78) | 32 (8–63) | 0.594 |
| Parents | 14.50 (8–22) | 11 (5–16) | 0.207 | 18 (5–29) | 16 (5–24) | 0.041 |
| Total | 43.50 (24–60) | 26 (25–52) | 0.116 | 39 (24–101) | 48 (20–85) | 0.953 |
| PedsQLChild | ||||||
| Pain and hurt | 56.25 (37.50–100) | 65.62 (43.75–100) | 0.063 | 87.50 (6.25–100) | 75 (50–100) | 0.865 |
| Daily activities | 77.50 (20–100) | 100 (65–100) | 0.043 | 100 (75–100) | 90 (45–100) | 0.068 |
| Treatment | 74.99 (39.28–100) | 85.71 (50–100) | 0.223 | 75 (35.71–92.85) | 78.57 (25–92.85) | 1.000 |
| Worry | 66.66 (16.66–100) | 74.99 (33.33–100) | 0.109 | 66.66 (0–83.33) | 83.33 (0–100) | 0.079 |
| Communication | 75 (25–100) | 79.16 (33.33–100) | 0.577 | 100 (33.33–100) | 83.33 (41.66–100) | 0.167 |
| Total | 71.08 (30.61–96) | 77.34 (47.58–100) | 0.116 | 80.65 (55.89–89.05) | 84.64 (44.83–95.24) | 0.441 |
| PedsQL Parent | ||||||
| Pain and hurt | 56.25 (37.50–100) | 65.62 (37.50–93.75) | 0.197 | 90.62 (18.75–100) | 78.12 (41.66–100) | 0.348 |
| Daily activities | 82.50 (65–100) | 100 (45–100) | 0.276 | 95 (55–100) | 97.50 (50–100) | 1.000 |
| Treatment | 60.71 (53.57–96.42) | 80.35 (50–91.66) | 0.225 | 81.98 (28.57–100) | 78.56 (50–100) | 0.686 |
| Worry | 37.50 (0–100) | 58.33 (16.66–100) | 0.223 | 87.49 (0–100) | 79.16 (25–100) | 0.786 |
| Communication | 66.66 (50–100) | 66.66 (33.33–100) | 1.000 | 83.33 (50–100) | 91.66 (75–100) | 0.400 |
| Total | 56.17 (51.21–91.78) | 72.52 (39.83–92.86) | 0.075 | 81.90 (47.55–98.51) | 81.84 (53.33–93.99) | 0.866 |
Significant values are shown in bold.
cJADAS=Clinical Juvenile Arthritis Disease Activity Score, BOT-2 SF=Brunininks-Oseretsky Test of Motor Proficiency Second Edition Short Form, JAB-Q=Juvenile Arthritis Biopsychosocial Scale, PedsQL=Pediatric Quality of Life Inventory 3.0 Arthritis Module.
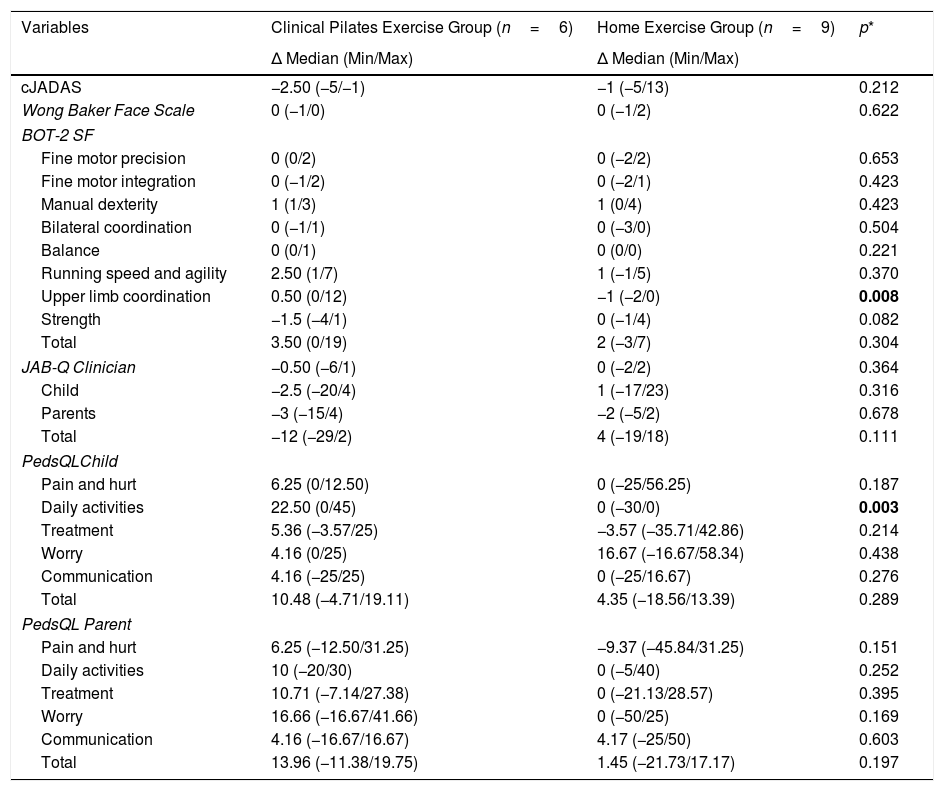
The Delta values of the participants were calculated by subtracting the pre-treatment result from the post-treatment result. When the delta values were compared, difference was significant in upper limb coordination subtest of BOT-2 SF (p=0.008) and daily activities subtest of PedsQL child form (p=0.003) in favor of Clinical Pilates exercise group (Table 4).
The comparison of delta values with groups.
| Variables | Clinical Pilates Exercise Group (n=6) | Home Exercise Group (n=9) | p* |
|---|---|---|---|
| Δ Median (Min/Max) | Δ Median (Min/Max) | ||
| cJADAS | −2.50 (−5/−1) | −1 (−5/13) | 0.212 |
| Wong Baker Face Scale | 0 (−1/0) | 0 (−1/2) | 0.622 |
| BOT-2 SF | |||
| Fine motor precision | 0 (0/2) | 0 (−2/2) | 0.653 |
| Fine motor integration | 0 (−1/2) | 0 (−2/1) | 0.423 |
| Manual dexterity | 1 (1/3) | 1 (0/4) | 0.423 |
| Bilateral coordination | 0 (−1/1) | 0 (−3/0) | 0.504 |
| Balance | 0 (0/1) | 0 (0/0) | 0.221 |
| Running speed and agility | 2.50 (1/7) | 1 (−1/5) | 0.370 |
| Upper limb coordination | 0.50 (0/12) | −1 (−2/0) | 0.008 |
| Strength | −1.5 (−4/1) | 0 (−1/4) | 0.082 |
| Total | 3.50 (0/19) | 2 (−3/7) | 0.304 |
| JAB-Q Clinician | −0.50 (−6/1) | 0 (−2/2) | 0.364 |
| Child | −2.5 (−20/4) | 1 (−17/23) | 0.316 |
| Parents | −3 (−15/4) | −2 (−5/2) | 0.678 |
| Total | −12 (−29/2) | 4 (−19/18) | 0.111 |
| PedsQLChild | |||
| Pain and hurt | 6.25 (0/12.50) | 0 (−25/56.25) | 0.187 |
| Daily activities | 22.50 (0/45) | 0 (−30/0) | 0.003 |
| Treatment | 5.36 (−3.57/25) | −3.57 (−35.71/42.86) | 0.214 |
| Worry | 4.16 (0/25) | 16.67 (−16.67/58.34) | 0.438 |
| Communication | 4.16 (−25/25) | 0 (−25/16.67) | 0.276 |
| Total | 10.48 (−4.71/19.11) | 4.35 (−18.56/13.39) | 0.289 |
| PedsQL Parent | |||
| Pain and hurt | 6.25 (−12.50/31.25) | −9.37 (−45.84/31.25) | 0.151 |
| Daily activities | 10 (−20/30) | 0 (−5/40) | 0.252 |
| Treatment | 10.71 (−7.14/27.38) | 0 (−21.13/28.57) | 0.395 |
| Worry | 16.66 (−16.67/41.66) | 0 (−50/25) | 0.169 |
| Communication | 4.16 (−16.67/16.67) | 4.17 (−25/50) | 0.603 |
| Total | 13.96 (−11.38/19.75) | 1.45 (−21.73/17.17) | 0.197 |
Significant values are shown in bold.
cJADAS=Clinical Juvenile Arthritis Disease Activity Score, BOT-2 SF=Brunininks-Oseretsky Test of Motor Proficiency Second Edition Short Form, JAB-Q=Juvenile Arthritis Biopsychosocial Scale, PedsQL=Pediatric Quality of Life Inventory 3.0 Arthritis Module, Δ=Posttreatment–pretreatment.
As a result of our study, Clinical Pilates exercises in individuals with JIA reduced disease activity and also increased dexterity, running speed-agility, upper limb coordination, general motor skills and daily activity. Home exercises, on the other hand, increased dexterity, running speed- agility, upper limb coordination and had positive effects on both the child and the family.
In the literature, few studies examined the effectiveness of pilates exercises in children with JIA.10,11 In their pilot study, Unal et al. investigated the effects of clinical pilates exercises on functional status, general health perception and pain. In addition to Clinical Pilates exercises, dance therapy and body imagery exercises are included in the treatment program. There is no control group in which the results were compared in this study. As a result of the study, the positive effects of Clinical Pilates exercises on decreased pain, improved function and overall understanding of health were recorded. Also it has been reported that Clinical Pilates exercises can be considered a reliable exercise model for children with JIA.10
The other study on clinical pilates in individuals with JIA belongs to Mendonca et al., the primary objective of the study was to determine the effect of Clinical Pilates exercises on health-related quality of life, while the secondary objective was to determine the effects of joint pain intensity, disability and joint status.11 Participants were randomized into conventional exercise or Pilates exercise groups. Both treatment methods were applied for 6 months. The Canadian Stott-Pilates method was applied to the Pilates exercise group. The method includes floor exercise, exercises with the Reformer, Stability Chair, Cadillac, and Ladder Barrel exercises. The authors concluded that the physical and psychosocial effects of pilates exercises in children and adolescents with JIA were more positive. Pilates exercises should be considered part of the rehabilitation program for patients with JIA and in the future, these positive developments should be supported with studies conducted using more objective parameters.
Disease activity scores are the most important determinants in determining whether treatments are effective on the disease. To our knowledge, this study is the first to assess the impact of Clinical Pilates exercises on disease activity in individuals with JIA and cJADAS were used in the assessment. We believe that the significant improvement in cJADAS scores in this study, will contribute significantly to the literature on the applicability of Clinical Pilates exercises as part of safe rehabilitation programs and shape the perspectives of clinicians and researchers.
It is stated that JIA leads to loss of function and motor control disorders in individuals.5 In 50% of children with JIA, muscle weakness occurs, especially in the upper extremity and most often with reduction in hand strength.22 JIA causes motor symptoms such as swelling of joints, effusion, tenderness, limitation of joint movements caused by pain, muscle weakness and atrophy, balance and gait disorders.23 In this study, individuals with JIA were evaluated with BOT-2 SF in detail in motor skills and significant improvements were obtained in both exercise groups. We believe that significant improvements in manual dexterity, running speed-agility, upper limb coordination and general motor skills are the result of increased proximal muscle strength and stabilization by exercise and this increase is reflected positively to the distal joints of the extremities. Thus, we believe that an increase in motor skills can be achieved.
In this study, we evaluated the effect of Clinical Pilates exercises on the quality of life of children/adolescents with JIA and the results we obtained from PedsQL were in line with the literature. With increased of the mobility level of the child/adolescent, the child/adolescent became more active in daily activities and this enabled us to achieve positive improvements in quality of life.
We think that there are few studies about the effectiveness of exercise in individuals with JIA in the literature and more information is needed about home exercise program which is one of the exercise methods.
Sandstedt et al. studied the effects of exercise on muscle strength, physical fitness, and well-being in children with JIA. The study included 54 JIA and the exercises were administered as a home program (exercise 3 days a week and 12 weeks as rope jumping, muscle strength exercises, body stabilization exercises and arm strengthening exercises with weights). As a result of the study, there was little change in quality of life scores as a result of exercise therapy as a home program, and significant improvement in strength of hip flexors and knee extensors. The authors reported that the given home exercise program was well tolerated by participant.24
Tarakçı et al. conducted a study to investigate the effect of home exercise program on pain, functional ability and quality of life in individuals with JIA. 81 children with JIA were included in the study, randomized in the exercise (4 days a week with 1 day in hospital for 12 weeks) or the control group (no intervention). As a result of the study, the authors reported that a 12-week individually planned home exercise program resulted in an increase in physical function and quality of life in children with JIA.25
Strengths of this study are the comparison of the effectiveness of Clinical Pilates exercises with the control group, and this is the first study to evaluate the impact of Clinical Pilates exercises on disease activity in individuals with JIA.
LimitationsLimitation of this study is small sample size.
ConclusionsAs a result, we believe that the significant improvement in cJADAS scores achieved by Clinical Pilates exercises in individuals with JIA will contribute significantly to the literature on the applicability of Clinical Pilates exercises as part of safe rehabilitation programs. In addition, we think it will shape the perspectives of clinicians and researchers. In addition, Clinical Pilates exercises made children/adolescent with JIA more active in daily activities by increasing mobility. This has enabled us to achieve positive improvements in quality of life. We believe that significant improvements of BOT-2 SF in manual dexterity, running speed-agility and upper limb coordination subtests and general motor skills are the result of increased proximal muscle stabilization through exercise and this increase is reflected positively to the distal joints of the extremities. And so we believe that an increase in motor skills has been achieved.
In these positive developments obtained with Clinical Pilates exercises, We think that it is effective to apply exercise as a supervisor and as a group. Should the practice method of Clinical Pilates exercises in children/adolescent with JIA be supervised or one-to-one? We recommend investigating which method is more effective in future studies.
Ethical approvalThe ethical approval of the study was obtained from local ethics committee at the board meeting dated 02.07.2019 and numbered 12. All individuals were informed verbally and informed consent forms were signed.
FundingNo funding was received.
Conflict of interestNo potential conflict of interest was reported by the authors.