Granulomatosis with polyangiitis (Wegener) is considered as a systemic, non-infectious granulomatous disease, histologically noted for its small vessel necrotizing vasculitis. The upper and lower respiratory tracts are the most frequently affected, in association with renal manifestations. However, the isolated involvement of a single organ, such as the eyeball and the orbit are also described. The case is presented of a woman whose main manifestation was an inflammatory process of periorbital tissue and proptosis of the left eyeball. The patient was evaluated jointly with eye plastic surgery, and the ear, nose and throat, and rheumatology departments.
A literature review was carried out, looking for case reports and case series that allowed comparisons to made between the clinical manifestations and the most frequent outcomes.
La granulomatosis con poliangeítis (Wegener) es considerada como una enfermedad granulomatosa sistémica, no infecciosa, caracterizada histológicamente por una vasculitis necrosante de pequeño vaso. El tracto respiratorio superior e inferior son los más frecuentemente afectados, en asociación a manifestaciones renales. Sin embargo, también se describe el compromiso aislado de un solo órgano, como es el caso del globo ocular y la órbita. Presentamos el caso de una mujer cuya principal manifestación consistió en un proceso inflamatorio de tejido periorbitario y proptosis del globo ocular izquierdo. La paciente fue valorada en manejo conjunto con el servicio de plástica ocular, otorrinolaringología y finalmente se derivó a reumatología para inicio de terapia inmunosupresora.
Se realizó una revisión de la literatura, en búsqueda de reportes de caso y series de caso que permitieran comparar las presentaciones clínicas y desenlaces más frecuentes.
Granulomatosis with polyangiitis (GPA)1,2 is a systemic, non-infectious granulomatous disease, histologically characterized by small vessel necrotizing vasculitis.3 The upper and lower respiratory tracts are the most frequently affected and usually it is associated with pauci-immune glomerulonephritis.4 Among the isolated manifestations over the course of the disease, 52% of the patients with GPA present ocular manifestations,5 primarily necrotizing nodular episcleritis, scleritis and corneal ulcerations.4 Recent reviews estimate that the orbital involvement is more frequent than expected,6 which becomes a serious challenge due to impaired eyesight secondary to optic nerve compression, if it is not timely detected and managed.
There are a few cases of the disease reported in Colombia; however, there are yet no official figures regarding the incidence and prevalence of orbital pseudotumor secondary to this systemic disease. Moreover, the Latin American literature in quite sparse in terms of the isolated orbital involvement as the initial manifestation.
Following is a discussion of a case of a female patient with proptosis who was treated in several occasions as preseptal cellulitis, neglecting the clinical history that could have guided the practitioner toward an accurate diagnosis, and turned it into a multidisciplinary challenge.
Clinical case54-Year old female patient original from Bogotá. History of weekly alcohol abuse since she was 15 years old until she became intoxicated. She smoked half a pack of cigarettes per day also since she was 15. The patient presented with upper respiratory symptoms in December 2016, due to nasal congestion, purulent post-nasal drip, epistaxis on one occasion and frontal headache, associated with erythema and left eyeball edema, leading to a diagnosis of maxillary sinus sinusitis and periorbital cellulitis. These episodes (approximately 8) experienced periods of improvement, with partial response until February 2017.
The patient received several cycles of broad-spectrum antibiotics, including metronidazole, clindamycin, ciprofloxacin, amoxicillin piperacillin/tazobactam and vancomycin.
In August 2017 she comes to the clinic with a 6-month proptosis, and is assessed by ENT and the decision was made to perform canthopexy, maxillary antrostomy and anterior ethmoidectomy. A biopsy is collected from the mucosa which reported an acute and chronic inflammatory process with granulation tissue, soft tissues with abundant foamy histiocytes; the special stains failed to identify any microorganisms. An extra-institutional culture and hemoculture was performed prior to administering the antibiotic and it came out negative for microorganisms. However, based on the clinic, antibiotic therapy was initiated with cefepime for 7 days, leading to hospital at home care.
The doctors advised to refer the patient to ophthalmology due to the suspicion of orbital pseudotumor versus infiltrative process of the lacrimal gland. In view of the delay to authorize the patient's referral for assessment, the patient comes to the emergency department of our institution in October 2017, because she was experiencing photophobia, diplopia, reduced visual acuity, severe left ocular proptosis, blepharoptosis, associated with subjective vertigo and hearing loss.
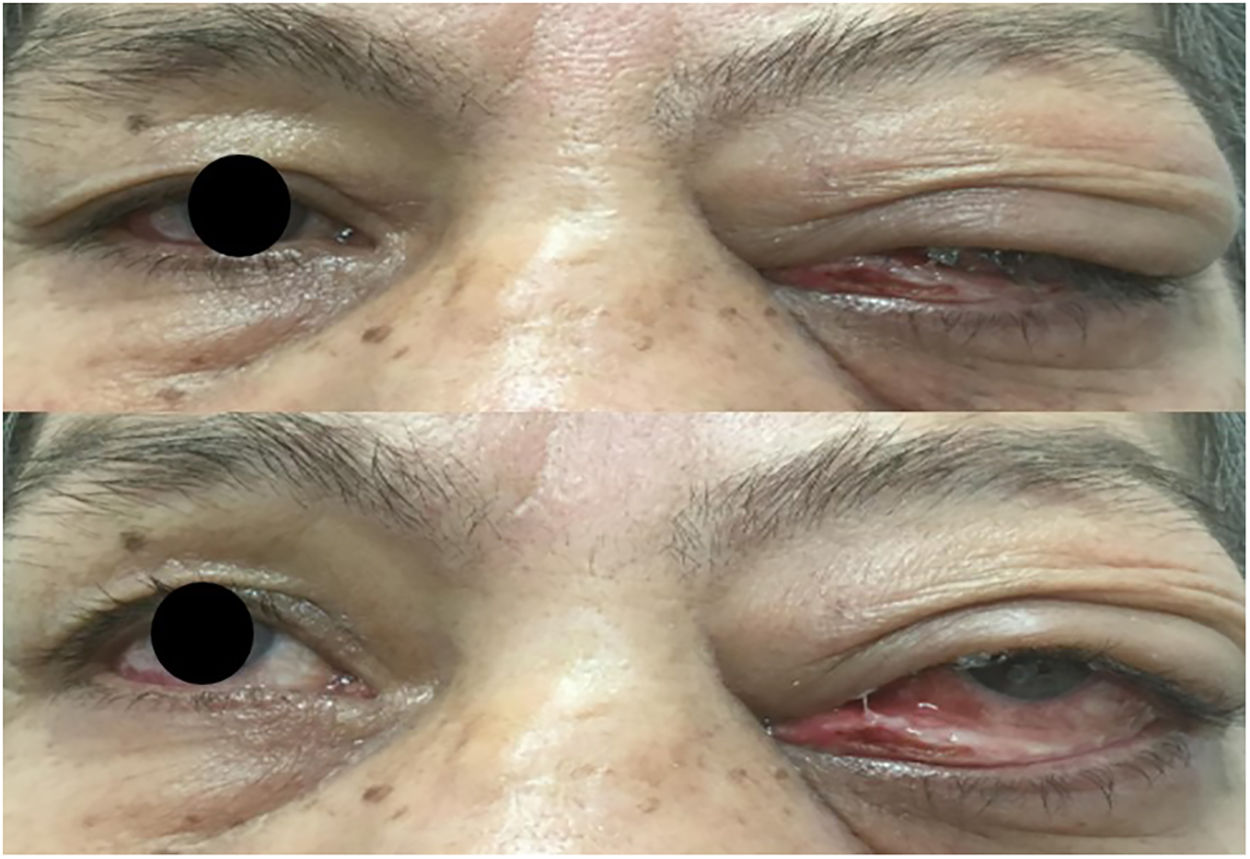
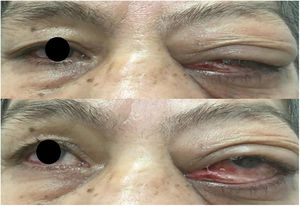
The ophthalmological examination revealed a 20/20 right eye visual acuity; left eye: 20/40, edema and periorbital induration more predominant in the upper lid, and restricted lateral eye movements (Fig. 1). The biomicroscopy resulted in preserved pupillary reflexes, healthy anterior segment of the right eye, left eye with 2mm lagophthalmos, hyperemic conjunctiva and chemosis, mucopurulent secretion, intraocular pressure and eye fundus within the normal limits.
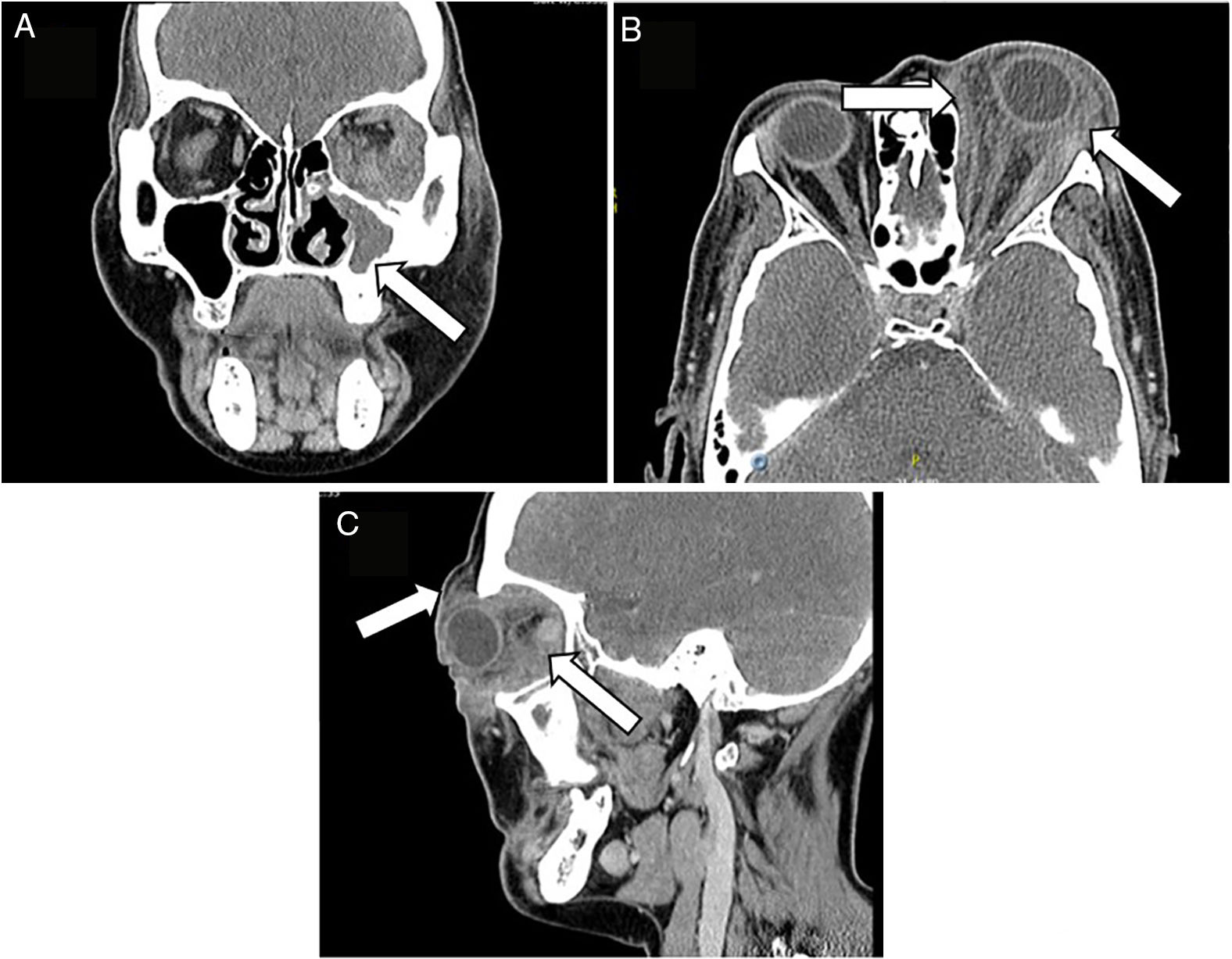
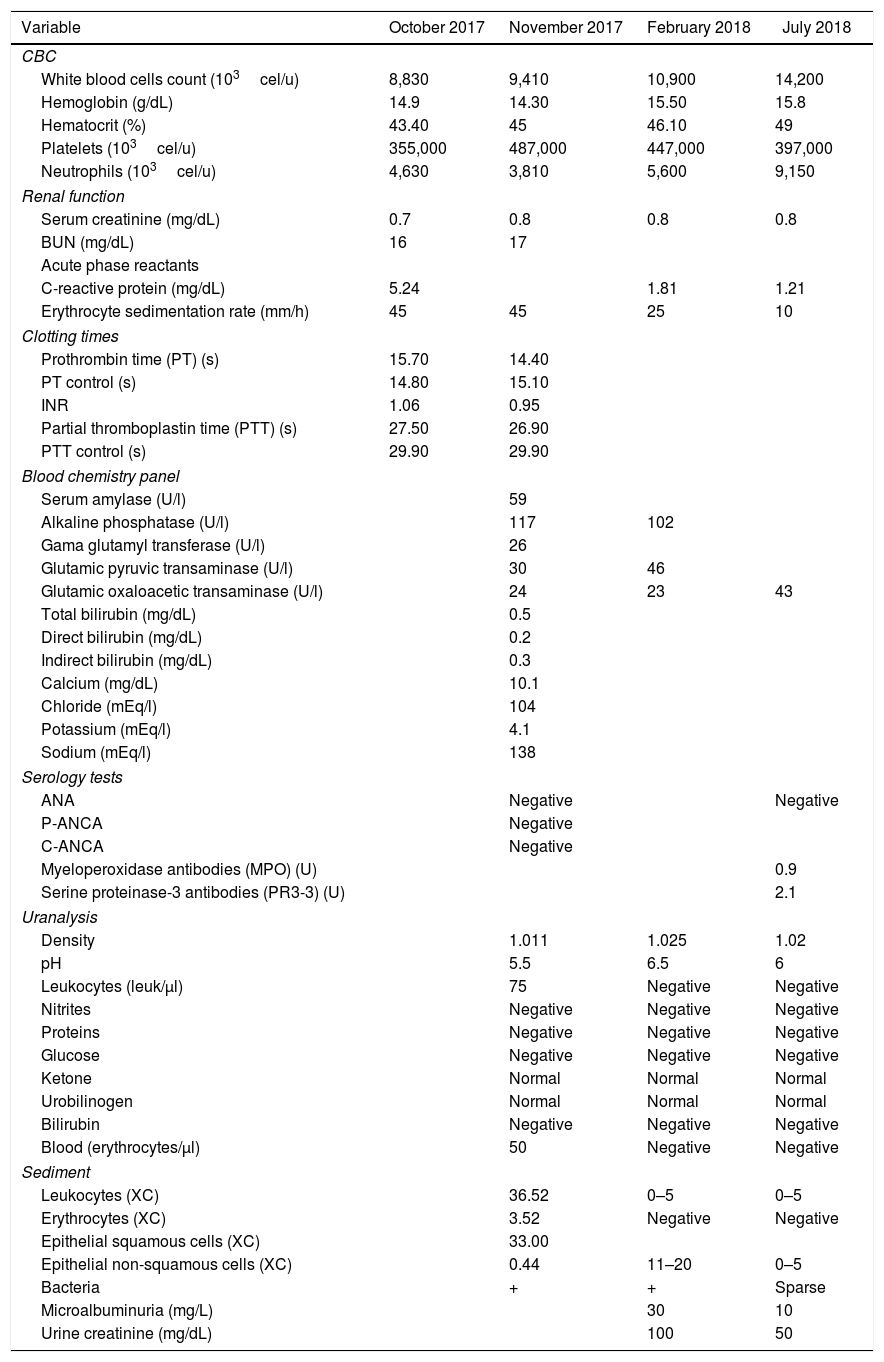
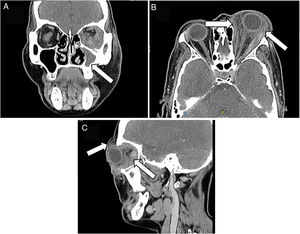
A face CT-scan was ordered which showed as the primary diagnostic probability an orbital pseudotumor, lymphoproliferative disease or chronic mycotic process (Fig. 2). Joint management with ENT was advised and the ENT specialists prescribed audiometry which documented left ear neurosensorial hearing loss. A nuclear magnetic resonance of the cerebellopontine angle was indicated, which showed absence of lesions, presence of otomastoiditis and left maxillary sinusitis. The blood chemistry panel (Table 1) was normal and urinary sediment reporting isolated microhematuria, probably associated with asymptomatic bacteriuria.
CT-scan of the face: (A) the left maxillary sinus is completely occupied, with soft tissue density associated with thickening of the adjacent bone cortex, relating to chronic inflammatory changes. (B and C) Diffuse alteration of the left periorbital soft tissues, with heterogeneous density enhancement of the pre and post-septal segment, with extension into the soft intra and extraconal tissues, promoting secondary proptosis without developing a definite mass; such inflammatory changes extend into the supraorbital, palpebral and malar region, with no evidence of organized fluid collections.
Laboratory results.
| Variable | October 2017 | November 2017 | February 2018 | July 2018 |
|---|---|---|---|---|
| CBC | ||||
| White blood cells count (103cel/u) | 8,830 | 9,410 | 10,900 | 14,200 |
| Hemoglobin (g/dL) | 14.9 | 14.30 | 15.50 | 15.8 |
| Hematocrit (%) | 43.40 | 45 | 46.10 | 49 |
| Platelets (103cel/u) | 355,000 | 487,000 | 447,000 | 397,000 |
| Neutrophils (103cel/u) | 4,630 | 3,810 | 5,600 | 9,150 |
| Renal function | ||||
| Serum creatinine (mg/dL) | 0.7 | 0.8 | 0.8 | 0.8 |
| BUN (mg/dL) | 16 | 17 | ||
| Acute phase reactants | ||||
| C-reactive protein (mg/dL) | 5.24 | 1.81 | 1.21 | |
| Erythrocyte sedimentation rate (mm/h) | 45 | 45 | 25 | 10 |
| Clotting times | ||||
| Prothrombin time (PT) (s) | 15.70 | 14.40 | ||
| PT control (s) | 14.80 | 15.10 | ||
| INR | 1.06 | 0.95 | ||
| Partial thromboplastin time (PTT) (s) | 27.50 | 26.90 | ||
| PTT control (s) | 29.90 | 29.90 | ||
| Blood chemistry panel | ||||
| Serum amylase (U/l) | 59 | |||
| Alkaline phosphatase (U/l) | 117 | 102 | ||
| Gama glutamyl transferase (U/l) | 26 | |||
| Glutamic pyruvic transaminase (U/l) | 30 | 46 | ||
| Glutamic oxaloacetic transaminase (U/l) | 24 | 23 | 43 | |
| Total bilirubin (mg/dL) | 0.5 | |||
| Direct bilirubin (mg/dL) | 0.2 | |||
| Indirect bilirubin (mg/dL) | 0.3 | |||
| Calcium (mg/dL) | 10.1 | |||
| Chloride (mEq/l) | 104 | |||
| Potassium (mEq/l) | 4.1 | |||
| Sodium (mEq/l) | 138 | |||
| Serology tests | ||||
| ANA | Negative | Negative | ||
| P-ANCA | Negative | |||
| C-ANCA | Negative | |||
| Myeloperoxidase antibodies (MPO) (U) | 0.9 | |||
| Serine proteinase-3 antibodies (PR3-3) (U) | 2.1 | |||
| Uranalysis | ||||
| Density | 1.011 | 1.025 | 1.02 | |
| pH | 5.5 | 6.5 | 6 | |
| Leukocytes (leuk/μl) | 75 | Negative | Negative | |
| Nitrites | Negative | Negative | Negative | |
| Proteins | Negative | Negative | Negative | |
| Glucose | Negative | Negative | Negative | |
| Ketone | Normal | Normal | Normal | |
| Urobilinogen | Normal | Normal | Normal | |
| Bilirubin | Negative | Negative | Negative | |
| Blood (erythrocytes/μl) | 50 | Negative | Negative | |
| Sediment | ||||
| Leukocytes (XC) | 36.52 | 0–5 | 0–5 | |
| Erythrocytes (XC) | 3.52 | Negative | Negative | |
| Epithelial squamous cells (XC) | 33.00 | |||
| Epithelial non-squamous cells (XC) | 0.44 | 11–20 | 0–5 | |
| Bacteria | + | + | Sparse | |
| Microalbuminuria (mg/L) | 30 | 10 | ||
| Urine creatinine (mg/dL) | 100 | 50 | ||
The patient was discharged since this was a chronic process with no systemic involvement and was scheduled for ambulatory biopsy and establish the diagnosis of pseudotumor versus a malignant process.
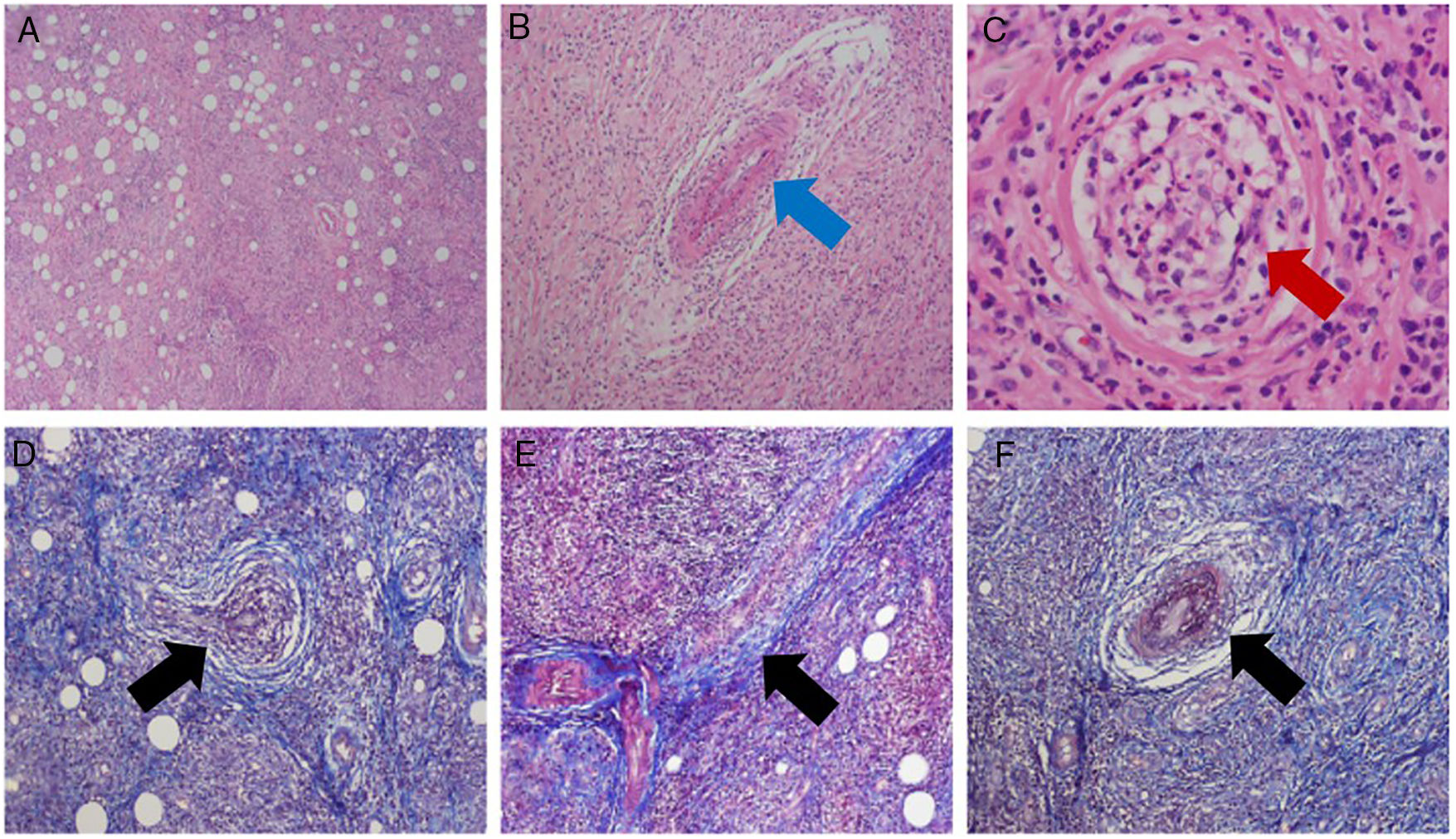
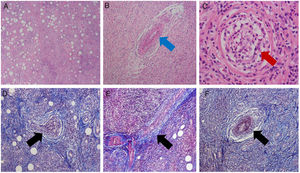
The patient was readmitted to the ED due to persistent ophthalmological symptoms and with the histopathology results. The new report submits negative stains for microorganisms, evidence of chronic and acute inflammatory infiltrate, granulomatous reaction with giant cells and the presence of vasculitis in the arterioles and venules (Fig. 3). An interconsultation with internal medicine and rheumatology asked for further studies (Table 1), chest X-ray with no pulmonary involvement. A diagnosis of GPA was finally concluded due to the findings in the biopsy and the clinic. Methylprednisolone IV pulses 500mg/day, were prescribed for 3 days following parasite cleanse, switch to oral administration with prednisone 1mg/kg/day. The clinical evolution of the patient improved and tolerance was adequate.
Histopathological study. Upper: H&E stain. Lower: Masson trichrome stain. (A) General view: connective and adipose tissue with abundant acute and chronic inflammatory infiltrate (lymphocytes and polymorphic nuclear neutrophils) forming stem centers, with con eosinophilia and focal necrosis. (B–F) Granulomatous reaction with giant cells and the presence of vasculitis of the muscle arteriolar vessels (red arrow) and venules (blue arrow), due to hyperplasia of the vascular walls, vascular occlusion and fibrinoid necrosis (black arrow).
Finally, the patient was discharged with a regimen based on cyclophosphamide 750mg/month for 6 months, steroids 1mg/kg/day until further notice, and prophylactic trimethoprim/sulfamethoxazole 160mg/800mg Monday, Wednesday and Friday.
Currently, because of insurance authorization delays, the patient has been unable to complete her treatment and hence the response has been partial, with persistent proptosis and compromised visual acuity.
DiscussionGPA is a small vessel vasculitis associated with the presence of antineutrophil cytoplasmic antibodies7; however, their positivity is not essential for a clinical diagnosis. This disease is mainly characterized by compromised upper and lower respiratory tract, associated with renal manifestations.7 It should be highlighted that the literature describes the isolated involvement of other anatomic structures, such as the orbit, which was the principal manifestation in this particular patient, in whom the diagnosis was established based on the criteria of the American College of Rheumathology,7 in the light of the findings of the biopsy and the purulent nasal discharge.
With regards to the ocular involvement, it is estimated to range between 14 and 60% of the patients diagnosed with GPA, mainly necrotizing nodular episcleritis, scleritis, corneal ulcers and retinal vasculitis4; the orbital manifestations are present in 45–60% of the patients with the disease,6 and it is estimated to be the primary target, prior to the development of systemic manifestations.6,8 In more than 10% of the patients with this isolated involvement, the antineutrophil cytoplasmic antibodies result negative,9 as is actually this case.
The presentation of the retroorbital granulomatous pseudotumor is usually unilateral and compromises the intra- and extraconal space; only 5% of the masses are limited to the intraconal space,10 meaning due to a primary or secondary origin after the underlying sinus inflammation.4 GPA with orbital involvement is clinically expressed as proptosis and the subsequent mechanical compression leading to atrophy of the optic nerve and blindness in 17% of the cases11; enophthalmos, in the late phase of the pseudotumor due to contracture of the orbital cavity6,10; epiphora, due to obstruction of the nasolacrimal ducts and infiltration of the lacrimal gland (dacryoadenitis); diplopia, due to direct compression of the eye globe, infiltration of the extraocular muscles, vasculitis that compromises the vasa vasorum of the extraocular muscles; ophthalmoplegia dolorosa, due to cranial nerve involvement (Tolossa-Hunt syndrome).6,10 The concomitant involvement of both branches of the VIII nerve – auditory and vestibular – is striking, due to a left otomastoiditis which was the culprit of the left ear neurosensory hearing loss and of the subjective vertigo.
In contrast to the literature review,12–45 all of these manifestations were present in the case reports and case series; of the 67 patients diagnosed with GPA and some kind of ocular involvement, 63 had orbital disease, around 25 patients had paranasal sinus involvement or clinical manifestations of sinusitis. The most frequent ocular symptoms and findings were impaired visual acuity, diplopia, proptosis, and extraocular movement limitations. The common denominator for treatment was cyclophosphamide, oral methylprednisolone pulses, methotrexate or azathioprine; in 25 patients their ocular symptoms improved without relapses, 10 patients were refractory to treatment and 9 of them required management with rituximab and 1 with infliximab; at least 6 experienced progressive visual acuity decline and finally became blind, around 7 underwent orbital decompression due to severe pain and significant visual acuity impairment, 2 required enucleation, one due to severe ocular pain and the second one due to non-response to corticoids or radiotherapy. With regards to gender, women were more affected.
With regards to the development of vasculitis and paranasal sinus-related periorbital cellulitis,11 these two may co-exist, as it was the case with this patient; this explains the periods of partial improvement with antibiotic therapy administered on several occasions. Nevertheless, considering the natural history of the underlying disease, it is necessary to add immunosuppressive therapy11 and cytotoxic agents (cyclophosphamide, azathioprine or methotrexate)6 to modulate the immune system. In case of relapse or refractory response to treatment, second line biologic therapy shall be required such as rituximab or infliximab.45 In terms of severe cases compromising the orbit and adjacent structures, ENT and ophthalmology shall be required to perform orbital decompression,9 in order to lower the risk of optic nerve ischemia and progression to blindness.
In this case, not all the differential diagnoses could be ruled out, but just the most frequent ones such as thyroid disease and infectious processes; this is a common pattern in all case reports. In this regard, the physician must keep in mind IgG4-related disease, thyroid disease (thyroid orbitopathy or Graves’ disease), sarcoidosis, temporal arteritis, polyarteritis nodosa, Kawasaki, histiocytosis, xanthogranuloma, cavernous hemangioma, lymphatic venous malformations, infection (post-septal cellulitis, mycobacteria infection, invasive fungal sinusitis due to Mucor or Aspergillus sp.), neoplastic processes such as lymphoma (predominantly B cells) and metastatic disease.6,8,10
ConclusionOn the basis of this clinical case, one may conclude that sound communication and doctor–patient relationship is essential, in addition to adequate communication among the healthcare practitioners for interdisciplinary management. Remember the importance of a detailed medical history and comprehensive physical examination, since any upper and lower respiratory tract disease-associated proptosis, or renal involvement as an isolated manifestation, represents a diagnostic aid for suspicious GPA, without ruling out the pathology, notwithstanding the non-positive antineutrophil cytoplasmic antibodies. Additionally, the clinician should be aware of the direct impact of a compromised orbit on optic nerve ischemia and the subsequent irreversible blindness, if timely intervention is not offered.
Patient perceptionDuring the ophthalmology clinical interview, the patient and her relative expressed their concern over the recurrence of the clinical situation, despite the multiplicity of treatments received. They also expressed their uncertainty about the long-term visual prognosis, since that could affect her daily life performance.
FundingNone declared.
Conflict of interestsThe authors have no conflict of interests to disclose.
Please cite this article as: Zea Durán M, Martínez-Ceballos MA. Proptosis ocular como una manifestación de la granulomatosis con poliangeítis (Wegener): Reporte de un caso y revisión de la literatura. Rev Colomb Reumatol. 2020;27:123–129.