To describe the frequency of extra-glandular cutaneous manifestations in patients with primary Sjögren's syndrome. To determine the clinical and laboratory profile of patients who present with these manifestations compared to those who do not.
Materials and methodsA study was made of patients included in GESSAR database (Sjögren Syndrome Society of Argentina Rheumatology Study Group) were analyzed. For the comparison between groups, the controls were randomly selected, with a case:control ratio of 1:4. Patients with purpura were compared with controls.
ResultsA total of 67 (14.1%) of the 474 patients included in the database had extra-glandular cutaneous manifestations. Of them, 58% had purpura. Arthritis, neuropathy, a decrease in C3 and C4 levels, and the presence of cryoglobulins, were statistically more frequent in cases compared to controls, although there was no independent association found with any of these variables. As regards purpura, arthritis, peripheral neuropathy, anemia, decrease in C3 and C4, anti-La, and cryoglobulinemia were statistically more frequent compared to controls. Only the decrease in C4, and the presence of cryoglobulins were independently associated with the presence of purpura.
ConclusionExtra-glandular cutaneous manifestations were observed in 14% of the patients. Purpura was the most frequent cutaneous manifestation. This was independently associated with decreased C4 and the presence of cryoglobulins.
Describir la frecuencia de manifestaciones cutáneas extraglandulares en pacientes con síndrome de Sjögren primario. Determinar el perfil clínico y de laboratorio de los pacientes que presentan estas manifestaciones en comparación con aquellos que no las presentan.
Materiales y métodosSe analizaron los datos de los pacientes incluidos en la base GESSAR (Grupo de Estudio Síndrome de Sjögren de la Sociedad Argentina de Reumatología). Para la comparación entre grupos, los controles se seleccionaron en forma aleatoria con una relación casos:controles de 1:4. A su vez, se compararon los pacientes con púrpura con los controles.
ResultadosSesenta y siete (14.1%) de los 474 pacientes incluidos en la base de datos tuvieron manifestaciones cutáneas extraglandulares. De ellos, el 58% tuvo púrpura. La artritis, la neuropatía, el descenso de C3 y de C4, y la crioglobulinemia fueron estadísticamente más frecuentes en los casos en comparación con los controles; sin embargo, no se encontró asociación independiente con ninguna de estas variables. En lo que respecta a púrpura, la artritis, la neuropatía periférica, la anemia, el descenso de C3 y de C4, anti-La y crioglobulinemia fueron estadísticamente más frecuentes en comparación con los controles. Solo el descenso de C4 y la positividad de crioglobulinas se asociaron en forma independiente a la presencia de púrpura.
ConclusiónEl 14% de los pacientes presentaron manifestaciones cutáneas extraglandulares. La púrpura fue la manifestación más frecuente. Esta se asoció en forma independiente con el descenso de C4 y la presencia de crioglobulinas.
Primary Sjögren's syndrome (pSS) is a systemic autoimmune disease characterized by the presence of xerophthalmia and xerostomia, due to the infiltration of the lacrimal and salivary glands by lymphoplasmacytic cells, which may affect other organs, such as the skin.1–3 Even though the most common cutaneous involvement is xeroderma, the extra-glandular commitment of the skin is a distinctive manifestation of the disease. Entities such as vasculitis, erythema annulare, Sweet's syndrome and erythema nodosum have been described. Among them, cutaneous vasculitis is of particular relevance given its frequency and prognostic value. The appearance of purpuric lesions in the lower extremities shows the existence of a vasculitic process associated with Sjögren's syndrome (SS); although vasculitis can also occur as cutaneous nodules, ulcers or urticariform lesions. Small vessel vasculitis mainly affects the skin and is histologically characterized by neutrophilic (leukocytoclastic vasculitis) or lymphocytic infiltrate.1,2,4–7 Purpura was reported in approximately 10% of patients with pSS and different studies have shown that its presence, at the time of diagnosis, carries a higher risk of switching into lymphoma.2–5,8,9 In different studies it has been observed that the cutaneous manifestations predominate in female patients, associated with other clinical or laboratory manifestations, such as peripheral neuropathy, presence of anti-Ro/SSA and anti-La/SSB antibodies, monoclonal gammopathy, cryoglobulinemia and hypocomplementemia.2–7,10
Given the absence of data reported in the literature regarding this manifestation in patients with pSS in Argentina, the primary objective of this study was to describe the frequency of extra-glandular cutaneous manifestations in a cohort of patients with pSS included in the database of the Sjögren Syndrome Society of Argentina Rheumatology Study Group (GESSAR). The secondary objective was to determine the clinical and laboratory profile presented by patients with these manifestations compared to those who do not exhibit them.
Materials and methodsPatientsPatients over 18 years of age with a diagnosis of pSS according to the 2002 American-European classification criteria, who are registered in the GESSAR database, were included in the study. Patients with other connective tissue diseases: rheumatoid arthritis, systemic lupus erythematosus, scleroderma, polymyositis, dermatomyositis, overlapping syndrome and mixed connective tissue disease were excluded.
Type of study and designAn observational, descriptive and longitudinal study was conducted to meet the primary objective. A case–control design was used to meet the secondary objective. The controls (patients without extra-glandular cutaneous manifestations) were randomly selected and compared with the cases (patients with extra-glandular cutaneous manifestations), with a case/control ratio of 1:4.
Data collectionIt was used the GESSAR multicenter database, whose primary objective is to estimate the frequency of glandular and extra-glandular manifestations of the pSS in Latin American population and also to estimate the percentage of patients with type I and type II pSS. This database was developed with the advice of national and international professionals, with broad experience in SS. The register and storage of the data is carried out in electronic format through a computer application. This application contains filters and help dialog boxes to optimize the reliability of the data. Physicians belonging to centers specialized in Rheumatology, both public and private, of different provinces of the country participate in it. To be included, the patients must meet the 2002 American-European criteria for pSS and be under active follow-up by the treating physician. The data of all the secondary manifestations of the disease that the patient presents during the course therein are incorporated and updated every 12 months, including the new manifestations that have arisen during this period of time. Patients must sign their informed consent prior to the inclusion of the information. The database is incorporated into the National Registry of Personal Data Protection.
To carry out this study, the following information was collected from the database: demographic characteristics (age, gender and time of evolution of the disease). The presence of extra-glandular cutaneous manifestations was considered as the dependent variable (purpura, urticarial vasculitis, petechiae, cutaneous ulcers, erythema multiforme, erythema nodosum and erythema annulare) and the clinical and serological manifestations detailed below, as independent variables: parotidomegaly, musculoskeletal involvement (arthralgias, arthritis, myositis), cardiovascular manifestations (Raynaud's phenomenon, pericarditis, myocarditis), respiratory manifestations (interstitial pneumonitis, lymphocytic alveolitis, pulmonary fibrosis, pleural effusion), gastrointestinal manifestations (esophageal dysmotility, chronic atrophic gastritis, Crohn's disease, ulcerative colitis, primary biliary cirrhosis, autoimmune hepatitis, sclerosing cholangitis), renal manifestations (renal tubular acidosis, glomerulonephritis), neurological manifestations (neuropathy, meningitis, neurocognitive compromise, transverse myelitis, vasculitis of the central nervous system), hematological manifestations (anemia, leukopenia, thrombocytopenia, lymphoma). The presence of mono, oligo and polyclonal hypergammaglobulinemia, rheumatoid factor, antinuclear factor, anti-Ro/SSA, anti-La/SSB antibodies, cryoglobulins, and decrease in complement (C3–C4) was investigated.
Statistical analysisThe continuous variables were reported as mean and standard deviation (SD) or median and interquartile range (IQR), according to the sample size and distribution. The categorical variables were reported in percentages. For the bivariate analysis, we used for the continuous variables the Student's test or the Mann–Whitney test, according to the sample size and distribution. The categorical variables were analyzed by Chi-square or Fisher's exact test, according to the expected frequency distribution table. A multivariate logistic regression analysis was performed, taking the cutaneous manifestations as dependent variable. A comparative subanalysis was performed with the controls, considering the purpura as the dependent variable.
Ethical objectionsThe GESSAR multicenter database is approved by an independent Ethics Committee and subject to the Helsinki International Standards of the World Medical Association. The patients must give and sign an informed consent prior to the inclusion of their data in the database.
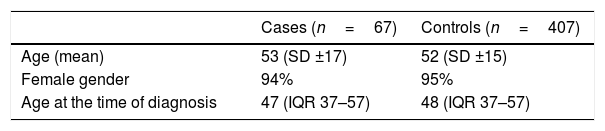
ResultsThe study included 474 patients, 67 of whom had extra-glandular cutaneous manifestations. The mean age of the cases was 53 years (SD ±17) and 94% of them were women. The demographic characteristics are described in Table 1. No statistically significant differences between cases and controls were found in terms of age, gender and time of evolution of the disease.
Of the 67 patients with extra-glandular cutaneous manifestations, 58% (n=39) had purpura, 19% (n=12) urticaria, 19% (n=12) petechiae, 16% (n=11) ulcers, 10% (n=7) subcutaneous nodules, 4% (n=3) erythema multiforme, 4% (n=3) erythema nodosum and 3% (n=2) erythema annulare. It should be highlighted that in our cohort of patients with pSS, 15 of the 67 patients with cutaneous manifestations presented 2 or more manifestations during the course of their disease.
The anatomopathological result of the biopsies of 18 patients with cutaneous manifestations was obtained; of these, 16 corresponded to leukocytoclastic vasculitis, one to lymphocytic vasculitis and one to granuloma annulare.
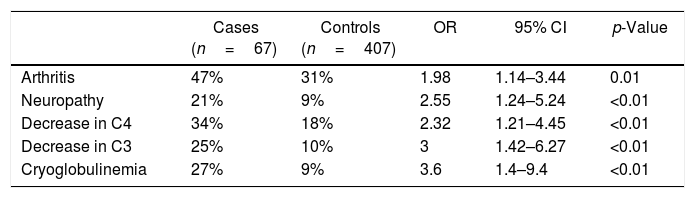
Association between cutaneous manifestations and clinical-immune commitmentWhen comparing the clinical manifestations collected from the database, both by systems and in each of them in particular, in the univariate analysis was found a significantly higher frequency of arthritis and neuropathy in the cases versus the controls (Table 2).
Bivariate analysis between patients with and without cutaneous manifestations.
| Cases (n=67) | Controls (n=407) | OR | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Arthritis | 47% | 31% | 1.98 | 1.14–3.44 | 0.01 |
| Neuropathy | 21% | 9% | 2.55 | 1.24–5.24 | <0.01 |
| Decrease in C4 | 34% | 18% | 2.32 | 1.21–4.45 | <0.01 |
| Decrease in C3 | 25% | 10% | 3 | 1.42–6.27 | <0.01 |
| Cryoglobulinemia | 27% | 9% | 3.6 | 1.4–9.4 | <0.01 |
When analyzing the laboratory alterations, a significantly higher frequency in the decrease of the C4 and C3 levels and positivity of cryoglobulins was observed in the cases compared to the controls (Table 2).
In the multivariate analysis, no independent association was found between the cutaneous manifestations and the mentioned variables, whether clinical or of laboratory.
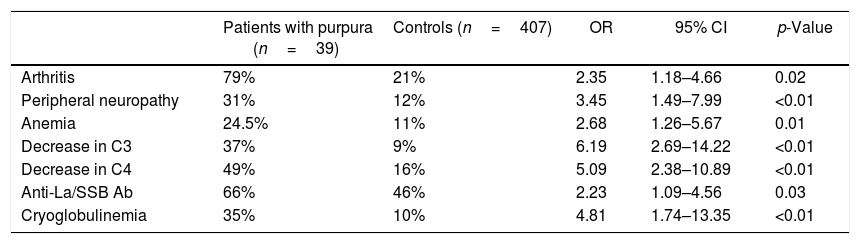
Association between purpura and clinical-immune commitmentRegarding the clinical manifestations, in the univariate analysis the patients with purpura showed a significantly higher frequency of arthritis, peripheral neuropathy and anemia of chronic disorders than the controls (Table 3).
Bivariate analysis between patients with purpura and without cutaneous manifestations.
| Patients with purpura (n=39) | Controls (n=407) | OR | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Arthritis | 79% | 21% | 2.35 | 1.18–4.66 | 0.02 |
| Peripheral neuropathy | 31% | 12% | 3.45 | 1.49–7.99 | <0.01 |
| Anemia | 24.5% | 11% | 2.68 | 1.26–5.67 | 0.01 |
| Decrease in C3 | 37% | 9% | 6.19 | 2.69–14.22 | <0.01 |
| Decrease in C4 | 49% | 16% | 5.09 | 2.38–10.89 | <0.01 |
| Anti-La/SSB Ab | 66% | 46% | 2.23 | 1.09–4.56 | 0.03 |
| Cryoglobulinemia | 35% | 10% | 4.81 | 1.74–13.35 | <0.01 |
When evaluating the results of the immunological laboratory, in the univariate analysis, in the patients with purpura was observed a significantly higher frequency in the decrease of C3 and C4 levels, anti-La/SSB antibodies and cryoglobulinemia (Table 3).
In the multivariate analysis, the decrease in C4 (OR: 4.8; 95% CI: 1.6–13.9, p<0.05) and the positivity of cryoglobulins (OR: 4.8; 95% CI: 1.4–16.3, p<0.05) were associated in an independent and statistically significant way with the presence of purpura.
DiscussionCutaneous lesions are frequently a sign of underlying disease and can be very helpful to get the diagnosis of a systemic disease, such as, for example, the connective tissue diseases. Systemic lupus erythematosus is the collagen disease that most characteristically presents skin manifestations. The pSS is another disease that may show cutaneous involvement. The lesions can be distinguished as non-vasculitic and vasculitis. Among the non-vasculitic lesions it was observed that photosensitivity and dryness of the skin (xerosis) are very common in patients with pSS, while palpable purpura is the most frequent among the lesions due to vasculitis.11,12
This study aimed to describe the frequency of extra-glandular cutaneous manifestations in patients with pSS and to determine the profile of clinical and laboratory manifestations presented by these patients compared with those who do not have such manifestations. A frequency of this commitment of 14% was observed, being purpura the most frequent form, followed by urticaria and petechiae.
Similarly as in our study, Ramos-Casals et al. reported in 2004 a frequency of cutaneous manifestations of 16% in a cohort of 558 patients. Of them, 58% had cutaneous vasculitis, being palpable purpura the form of expression most commonly found. They observed that the patients with cutaneous vasculitis had a higher frequency of articular affectation, peripheral neuropathy, Raynaud's phenomenon, renal involvement, antinuclear antibodies, rheumatoid factor, anti-Ro/SSA antibodies and need for hospitalization, compared with the patients with pSS without vasculitis. This shows the presence of a more severe disease and with greater systemic commitment in these cases.13,14
In 2004, Bernacchi et al. published a study which included 93 patients from 9 centers in Italy. In contrast to our work, the patients included had a diagnosis of pSS (n=62) and secondary SS (n=31). They observed a higher frequency of cutaneous vasculitis and erythema annulare compared with that observed in our cohort of patients.15
In 2015, Quartuccio et al. published a study in which they evaluated the clinical and laboratory differences between the patients with cryoglobulinemic purpura and those with purpura associated with hypergammaglobulinemia in a multicenter cohort of patients with pSS. A total of 652 patients were included in this study. The results revealed that peripheral neuropathy, decrease in C4, leukopenia, monoclonal hypergammaglobulinemia and the presence of anti-La antibodies were observed more frequently in patients with cryoglobulinemic vasculitis, whereas rheumatoid factor, leukopenia, monoclonal hypergammaglobulinemia and anti-Ro antibodies were significantly linked with vasculitis associated with hypergammaglobulinemia. Lymphoma was only associated with cryoglobulinemic vasculitis.16 Even though this work has an objective different than ours, it also suggests that the differences in the immunological mechanisms involved in such type of commitment would have prognostic implications.
On the other hand, we found two cases of erythema annulare. Erythema annulare is characterized by the presence of polycyclic, annular, erythematous and photosensitive lesions. It was initially described in Asian patients with pSS and it can be the initial manifestation of the disease.17,18 Brito-Zerón et al. published in 2014 a study in which they reported 35 (9%) cases of erythema annulare in a Spanish cohort of 377 patients with pSS. The lesions were observed most frequently in the face and the upper extremities; anti-Ro/La antibodies were positive in 89% of the patients with such involvement. The work included a bibliographic search in which they identified 8 additional cases in non-Asian patients and 52 in Asian patients.6 In our study, we found a very low frequency of this manifestation, without being able to rule out the possibility of a underdiagnosis, especially if we consider that it may be the first manifestation of the disease.
Even though there are currently international and local recommendations that aim to optimize the diagnosis and treatment, there is little information regarding this type of systemic involvement in the pSS.19,20 We consider that our study is a contribution to the knowledge of the disease and that it could contribute to a better clinical management therein.
Conclusion14% of the patients have extra-glandular cutaneous manifestations. Purpura was the most frequent manifestation. It was associated independently with the decrease in C4 and the presence of cryoglobulins. This could show a more unfavorable evolution of the disease.
Conflict of interestNone.
Please cite this article as: Durigan V, Secco A, Duarte V, Troitiño C, Pellet AC, Mamani M, et al. Manifestaciones cutáneas extraglandulares en pacientes con Síndrome de Sjögren primario. Rev Colomb Reumatol. 2018;25:79–84.