Systemic lupus erythematosus (SLE) is a chronic disease that affects multiple systems and may include neurological and psychiatric events that could compromise treatment adherence and long-term outcomes in SLE.
ObjectiveTo evaluate treatment adherence in patients with diffuse neuropsychiatric disorders associated with SLE.
MethodsA cross-sectional descriptive study was conducted. Treatment adherence was evaluated with the Morisky Medication Adherence Scale (MMAS-8) in patients with diffuse neuropsychiatric disorders associated with SLE (cognitive impairment, psychosis, mood disorders, and anxiety).
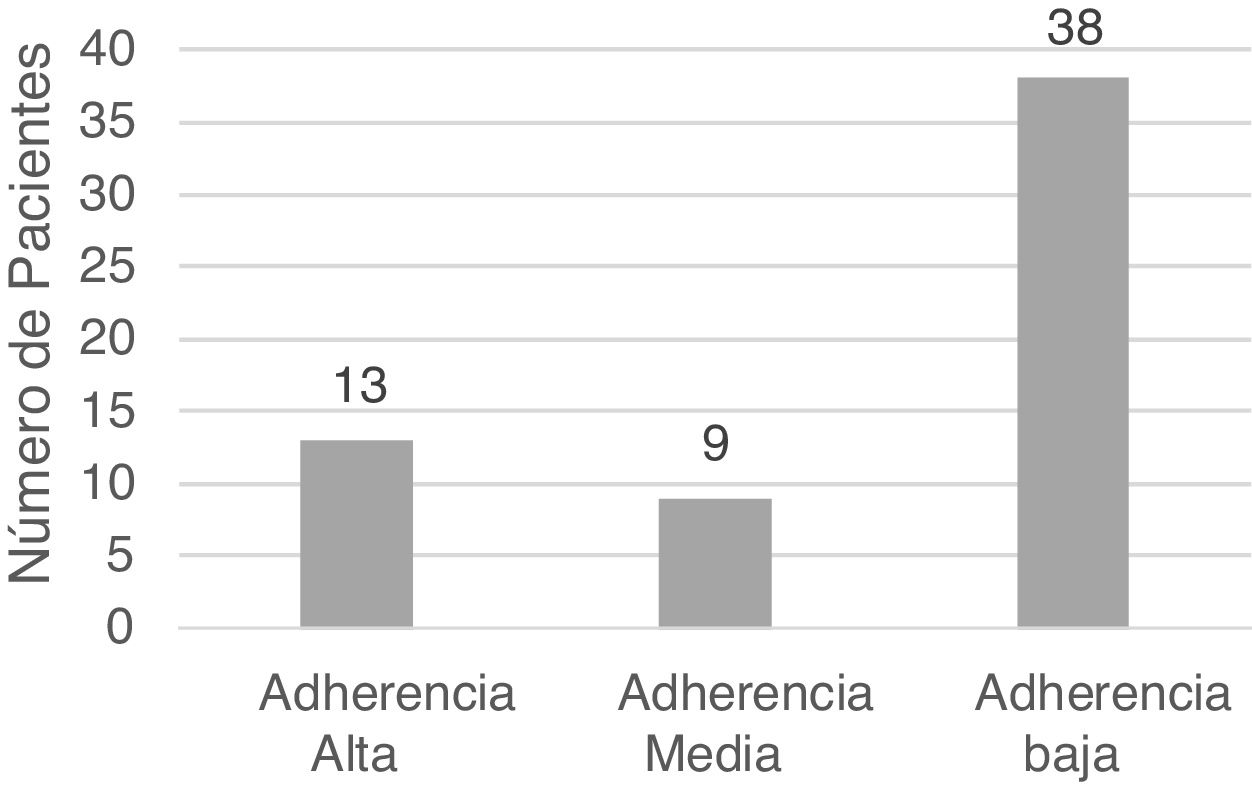
ResultsA total of 60 patients with neuropsychiatric disorders associated with SLE were included. Thirteen patients (21.6%) had high adherence, 9 (15%) had medium adherence, and 38 patients (63.3%) had low treatment adherence.
ConclusionThis study has identified that almost two-thirds of the participants (63.3%) had low treatment adherence.
El lupus eritematoso sistémico (LES) es una enfermedad crónica que afecta a múltiples sistemas, entre ellos el sistema nervioso, con eventos neurológicos y psiquiátricos que podrían influir en la adherencia al tratamiento y los resultados a largo plazo de la enfermedad.
ObjetivoEvaluar la adherencia al tratamiento de los pacientes con trastornos neuropsiquiátricos difusos asociados con LES.
MetodologíaSe llevó a cabo un estudio descriptivo transversal que evaluó el grado de adherencia al tratamiento con el test de Morisky en pacientes con trastornos neuropsiquiátricos difusos asociados con LES (alteración cognitiva, psicosis, trastornos del ánimo y ansiedad).
ResultadosSe incluyó a 60 pacientes con trastornos neuropsiquiátricos difusos asociados con LES, de los cuales 13 (21,6%) tuvieron adherencia alta, 9 (15%) adherencia media y 38 (63,3%) presentaron baja adherencia al tratamiento.
ConclusiónEn este estudio se identificó que más de la mitad de los participantes (63,3%) presentaron baja adherencia al tratamiento.
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that affects approximately 20–50/100,000 inhabitants worldwide.1 Current therapeutic approaches have improved the prognosis and the quality of life of the patients with this disease,2 however, their quality of life is lower than that of the general population.3
According to the American College of Rheumatology (ACR), neuropsychiatric syndromes associated with this disease include 19 entities. There are 12 that affect the central nervous system (CNS), of them, 5 are considered diffuse (cognitive alteration, psychosis, acute confusional state, mood disorders and anxiety).4
Timely diagnosis and adequate treatment can influence adherence, prognosis and the quality of life of the patients5; however, some studies demonstrate that adherence in these cases is not appropriate.2,6,7 This could be explained by several factors, such as the difficulty to accept the disease and the belief of the patients that the treatment is not necessary, the fear of the adverse effects of the drugs, the practical difficulties in obtaining the medications and the scarce communication between the doctor and the patient due to time limitations.7–10
Adherence to treatment refers to compliance with medical recommendations on drug regimens and changes in lifestyle, including the diet and exercise agreed with the patient.11 Treatments are usually complex and prolonged, and can predispose the patients not to adhere adequately.1
Neuropsychiatric disorders in patients with SLE can reduce therapeutic compliance and thus cause reactivation of the disease, increased number of visits to health care centers and the consequent impact on prognosis and quality of life. Therefore, the main objective of this study was to evaluate the degree of adherence to treatment in patients with diffuse neuropsychiatric disorders of the CNS associated with SLE.
Material and methodsPatientsAll patients with a diagnosis of diffuse neuropsychiatric disorders associated with SLE, belonging to the Internal Medicine service of a third-level hospital in Ecuador were included. In total, there were 60 patients. The inclusion criteria were: meeting a diagnosis of SLE according to the Systemic Lupus International Collaborating Clinics 2012 criteria, having a diagnosis of diffuse neuropsychiatric disorders established through the MINI neuropsychiatric interview and the Montreal cognitive assessment, being over 15 years of age and agreeing to participate in the research through an informed consent/assent process. Patients under 15 years of age and a previous neuropsychiatric disease were considered as exclusion criteria.
InstrumentsThe Systemic Lupus International Collaborating Clinics 2012 criteria were used for the diagnosis of SLE, and the MINI neuropsychiatric interview and the Montreal cognitive assessment for the diagnosis of diffuse neuropsychiatric disorders, previously conducted by the services of Internal Medicine and Psychiatry. The lupus activity was evaluated according to the Systemic Lupus Erythematosus Disease Activity Index 2000. The 8-item Morisky Medication Adherence Scale (MMAS-8), a validated indirect method which was performed in Spanish was applied for this study. The score ranges from 0 to 8, considering a value of 8 as high adherence, 6–7 as medium adherence, and <6 as low adherence.12
ProcedureA descriptive cross-sectional study that evaluated the degree of adherence to treatment was conducted. This study was carried out from October 2017 to May 2018. Patients with a previous diagnosis of diffuse neuropsychiatric disorders of the CNS associated with SLE were evaluated in the outpatient clinic of the Internal Medicine service. An informed consent/assent process was carried out and sociodemographic and clinical characteristics were collected. Next, the assessment of the adherence to treatment was performed with the MMAS-8, which lasted approximately 10 min for each patient.
Statistical analysisTo perform the statistical analysis, the SPSS 23 software was used, the degree of adherence to treatment was calculated using the MMAS-8, and the main sociodemographic, clinical and neuropsychiatric characteristics were described.
Ethical considerationsThe study was approved by the Bioethics Committee of the hospital; the patients participated in the study through a written informed consent/assent process.
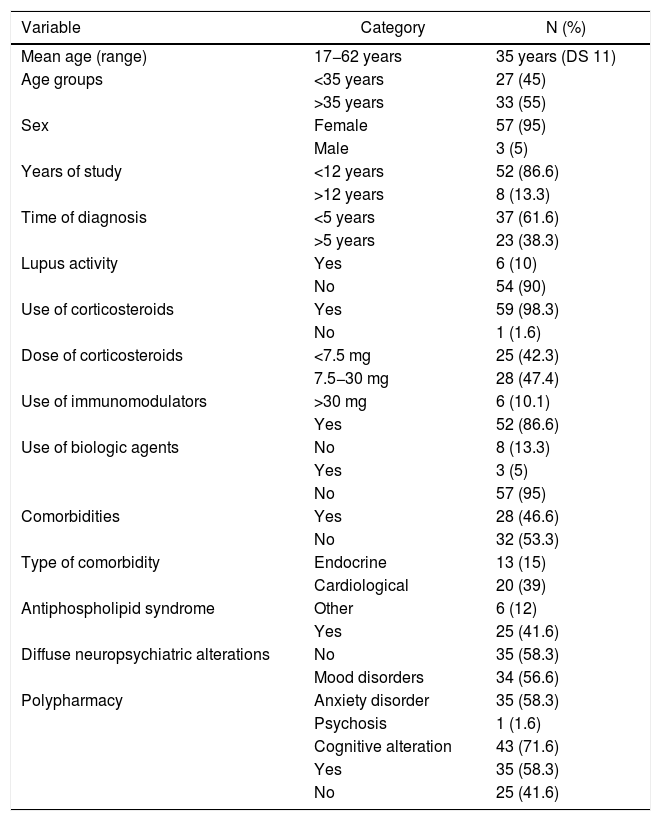
ResultsSixty patients with diffuse neuropsychiatric disorders associated with SLE were included, the mean age was 35 years and the majority of them were women, with at least 12 years of study. At the time of the research, 37 patients had a time of diagnosis of the disease <5 years and 90% did not present lupus activity according to the Systemic Lupus Erythematosus Disease Activity Index 2000. As for the medication, 98.3% took corticosteroids, and almost half of them used intermediate doses (between 7.5–30 mg/day), while 52 patients (86.6%) used immunomodulators and 3 (5%) received biological agents. In addition, 46.6% had comorbidities, mainly cardiological, and 25 patients (41.6%) had an association with antiphospholipid syndrome. In total, 58.3% of the participants received polypharmacy. The 4 most prevalent diffuse neuropsychiatric syndromes were: cognitive impairment (71.6%), mood disorders (56.6%), anxiety disorders (58.3%), and psychosis (1.6%). Table 1 describes the sociodemographic and clinical characteristics of the study population.
Demographic and clinical characteristics of the study population.
| Variable | Category | N (%) |
|---|---|---|
| Mean age (range) | 17−62 years | 35 years (DS 11) |
| Age groups | <35 years | 27 (45) |
| >35 years | 33 (55) | |
| Sex | Female | 57 (95) |
| Male | 3 (5) | |
| Years of study | <12 years | 52 (86.6) |
| >12 years | 8 (13.3) | |
| Time of diagnosis | <5 years | 37 (61.6) |
| >5 years | 23 (38.3) | |
| Lupus activity | Yes | 6 (10) |
| No | 54 (90) | |
| Use of corticosteroids | Yes | 59 (98.3) |
| No | 1 (1.6) | |
| Dose of corticosteroids | <7.5 mg | 25 (42.3) |
| 7.5−30 mg | 28 (47.4) | |
| Use of immunomodulators | >30 mg | 6 (10.1) |
| Yes | 52 (86.6) | |
| Use of biologic agents | No | 8 (13.3) |
| Yes | 3 (5) | |
| No | 57 (95) | |
| Comorbidities | Yes | 28 (46.6) |
| No | 32 (53.3) | |
| Type of comorbidity | Endocrine | 13 (15) |
| Cardiological | 20 (39) | |
| Antiphospholipid syndrome | Other | 6 (12) |
| Yes | 25 (41.6) | |
| Diffuse neuropsychiatric alterations | No | 35 (58.3) |
| Mood disorders | 34 (56.6) | |
| Polypharmacy | Anxiety disorder | 35 (58.3) |
| Psychosis | 1 (1.6) | |
| Cognitive alteration | 43 (71.6) | |
| Yes | 35 (58.3) | |
| No | 25 (41.6) |
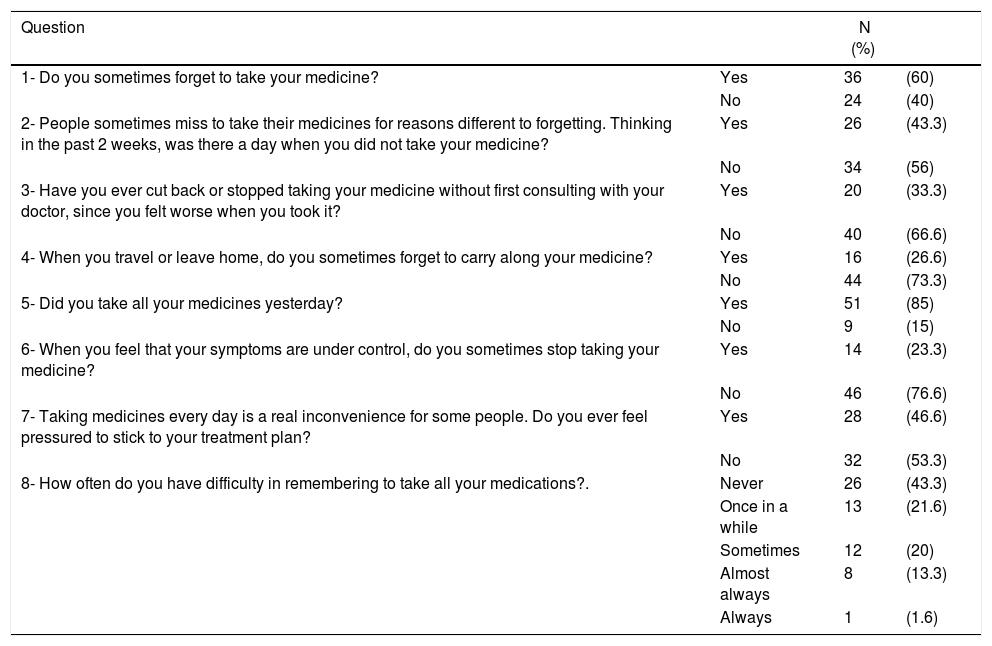
The MMAS-8 was used to assess adherence to treatment. Of the total population, 63.3% had low adherence (the global assessment is presented in Fig. 1). The breakdown of the answers obtained from the 8 questions that make up the MMAS-8 is found in Table 2.
Questions of the Morisky Medication Adherence Scale.
| Question | N (%) | ||
|---|---|---|---|
| 1- Do you sometimes forget to take your medicine? | Yes | 36 | (60) |
| No | 24 | (40) | |
| 2- People sometimes miss to take their medicines for reasons different to forgetting. Thinking in the past 2 weeks, was there a day when you did not take your medicine? | Yes | 26 | (43.3) |
| No | 34 | (56) | |
| 3- Have you ever cut back or stopped taking your medicine without first consulting with your doctor, since you felt worse when you took it? | Yes | 20 | (33.3) |
| No | 40 | (66.6) | |
| 4- When you travel or leave home, do you sometimes forget to carry along your medicine? | Yes | 16 | (26.6) |
| No | 44 | (73.3) | |
| 5- Did you take all your medicines yesterday? | Yes | 51 | (85) |
| No | 9 | (15) | |
| 6- When you feel that your symptoms are under control, do you sometimes stop taking your medicine? | Yes | 14 | (23.3) |
| No | 46 | (76.6) | |
| 7- Taking medicines every day is a real inconvenience for some people. Do you ever feel pressured to stick to your treatment plan? | Yes | 28 | (46.6) |
| No | 32 | (53.3) | |
| 8- How often do you have difficulty in remembering to take all your medications?. | Never | 26 | (43.3) |
| Once in a while | 13 | (21.6) | |
| Sometimes | 12 | (20) | |
| Almost always | 8 | (13.3) | |
| Always | 1 | (1.6) |
In our work, according to the Morisky test applied, only 21.6% of the patients had high adherence to their pharmacological treatment. Only patients with diffuse neuropsychiatric manifestations were analyzed; however, the result is consistent with published data on adherence in patients with SLE. For example, the first work on adherence measured with a direct method, in which the hour when the drug bottles were opened was monitored with an electronic system, reported that throughout the 2 years of study only 24% of the participants adhered to their treatment in more than 80% of the doses that were initially prescribed.13 In another more recent work, with 72 patients with SLE in an outpatient service of Internal Medicine in Spain, 63.9% did not have adequate adherence to treatment.14 On a regional scale, a work conducted in Peru determined an adherence of 25% in 48 patients with SLE.15
There are studies that describe adherence problems in patients with psychiatric disorders.
A study conducted in China found that the presence of anxiety in patients with SLE, had a negative influence on the adherence; in contrast, Alsowaida et al. associated it with depression.2,16
We described some variables of interest such as the years of study, time to diagnosis, lupus activity and polypharmacy; the latter was present in more than a half of the patients. In a study they found that the patients with high adherence had better punctuations in the sphere of mental health measured with questionnaires on quality of life, compared with those patients with lack of adherence to treatment. Furthermore, depression and polypharmacy were independent risk factors for poor adherence.13
In 2003 the World Health Organization (WHO) made a report on the problems of adherence to treatment in chronic diseases. Already on that date, the WHO considered it a global problem of alarming magnitude, which would have as a consequence an increase in direct and indirect healthcare costs and, logically, a negative impact on the health status of the individuals.17
We consider that evaluating adherence to treatment should be one of the priorities in the consultation of a patient with SLE, especially in patients with neuropsychiatric manifestations. According to the WHO, it is emphasized that “increasing the effectiveness of interventions on therapeutic adherence can have a much greater impact on the health of the population than any improvement in specific medical treatments-”17
Finally, the limitations of the study should be considered. This work was carried out with a relatively small sample; in addition, adherence to treatment and the presentation of neuropsychiatric disorders were measured with indirect methods subject to a margin of error, since they depended only on the veracity of the patient's report. On the other hand, the study was conducted in a public hospital, so there may be differences regarding the characteristics of the population in private centers or with greater and better access to health services. It was also not possible to differentiate the primary neuropsychiatric disorders caused directly by the SLE, from those secondary to factors such as treatment, comorbidities, other metabolic alterations or psychosocial factors.
ConclusionsIn our study population there is a significant number of patients (63.3%) with low adherence to treatment. The results highlight the importance of the diagnosis and treatment of neuropsychiatric disorders and their influence on adherence to treatment. The poor adherence to treatment in patients with SLE is a problem that must be taken into account in the management of this disease. New studies with larger samples and a more rigorous methodological design could identify risk factors for lack of adherence to management.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Cevallos Guerrero A, Fernández HÁ, Jimbo Sotomayor R, Guevara GC, Mera Orcés D, Naranjo-Saltos F. Adherencia al tratamiento en pacientes con trastornos neuropsiquiátricos difusos asociados a lupus eritematoso sistémico. Rev Colomb Reumatol. 2022;29:26–30.