Gardner-Diamond syndrome or psychogenic purpura is a vasculopathy characterized by a localized cutaneous reaction, associated with episodes of emotional stress or mental illness as trigger factors. A case of a female patient with multiple, intermittent, nodular, ecchymotic and painful lesions related to various stressing events that was treated as lupus is reported below.
El síndrome de Gardner-Diamond o púrpura psicógena es una vasculopatía de presunto origen autoinmune que se caracteriza por una reacción cutánea localizada, asociada a situaciones de estrés emocional. Se presenta el caso de una paciente con lesiones equimóticas, dolorosas y de aparición intermitente, relacionadas con diversos eventos estresores, que habían sido manejadas como manifestación de lupus.
Organic diseases associated with a psychological component generate a challenge to the clinician, both in the diagnosis and in the therapeutic approach; given that some manifestations can be erroneously attributed to self-inflicted lesions or be undervalued at the time of the evaluation. The Gardner-Diamond syndrome, also known as psychogenic purpura, autoerythrocyte sensitization syndrome or painful bruising syndrome,1–4 is one of these pathologies where the psychological component plays a primordial role as a triggering or exacerbating factor of the disease. This syndrome is a vasculopathy of presumed autoimmune etiology, which is characterized by a localized cutaneous reaction.1 It is mainly diagnosed in Caucasian women, under 30 years old, with emotional stress or one or more concomitant mental illnesses.2 Below we present the case of a 23-year-old patient, with a clinical picture of 10 years of evolution of multiple painful intermittent ecchymotic lesions in the upper and lower limbs, whose onset was related with various stressful events.
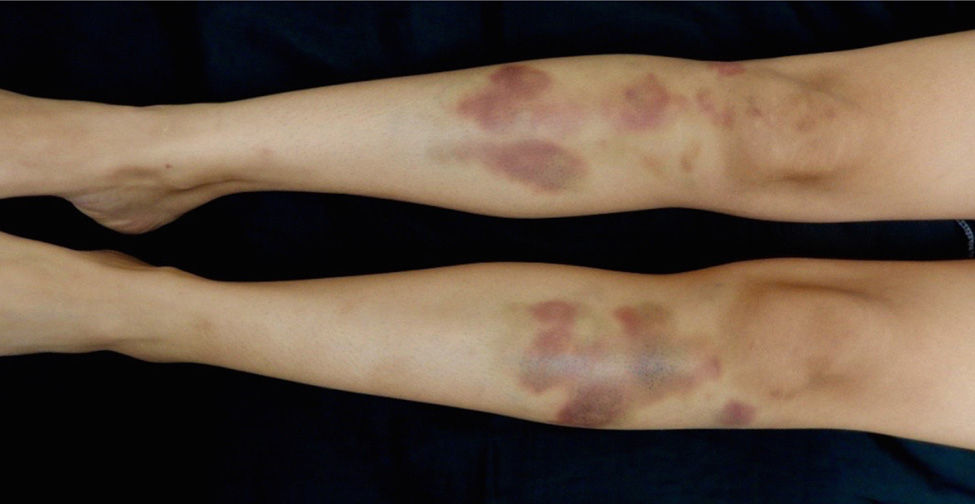
Case reportA 23-year-old woman, with unclear diagnosis of systemic lupus erythematosus (SLE) since she was 13 years old; according to the medical record of another institution, this diagnosis was made due to the presence of arthritis and macular lesions in the right knee, since then in management with prednisone 10mg daily. She consulted for a clinical picture of edema, erythema and local heat in the left forearm, of one month of evolution, which began after a soft tissue trauma in this area; in the outpatient clinic it was considered as a superficial soft tissue infection, and for this reason she received intrahospital management with intravenous clindamycin and ciprofloxacin for 16 days, without clinical improvement. Subsequently, appearance of violaceous indurated nodular lesions, very painful, associated with vasomotor changes (diaphoresis, coldness and hyperalgesia), in addition to polyarthralgias and objective fever of up to 38.5°C. The physical examination of the left forearm showed edema, as well as multiple violaceous nodules, indurated, not adhered to deep planes, and coldness on palpation of the extremity but with preserved pulses and capillary refill (Fig. 1). Initially, among the diagnostic options were considered: lupus panniculitis versus infectious process (atypical bacterial germs, tuberculosis or deep mycoses), and for this reason the patient was hospitalized in order to carry out an incisional biopsy and complementary studies to confirm or rule out the diagnosis of SLE.
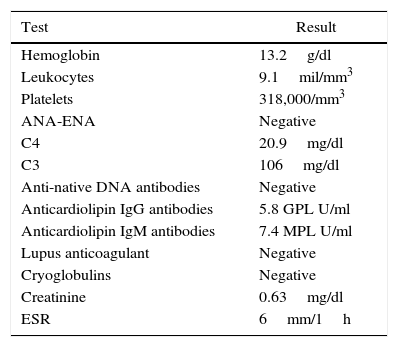
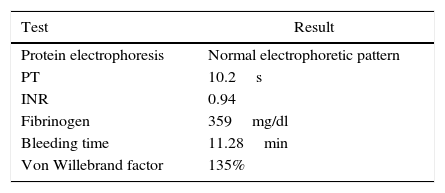
During the hospital stay, new nodules appeared in the contralateral forearm and the anterior tuberosity of both tibiae (Fig. 2), as well as postprandial abdominal pain of colic type of 8/10 intensity and sensation of paresthesia in the 4 limbs, which made us consider the diagnostic possibility of polyarteritis nodosa and, in view of the rapid evolution of the clinical picture it was decided, considering the risk/benefit, to administer pulses of methylprednisolone and to request computed angiotomography of the abdominal aorta, electromyography and nerve conduction study of the four extremities. These studies were performed on a priority basis, reporting computed angiotomography within normal limits, as well as electromyography and nerve conduction without evidence of peripheral neuropathy or multiple mononeuritis. The skin biopsy reported epidermis and mid dermis without changes; deep dermis and subcutaneous cellular tissue with abundant extravasated erythrocytes, mild fibrosis of the septa of the adipose panniculus and discreet lymphocytic inflammatory infiltrate in the lobule, without changes of small or medium vessel vasculitis, without thrombotic phenomena or changes that suggest infectious or lupus panniculitis, special stains (ZN, modified ZN and methenamine silver) negative. Given the foregoing and added to the paraclinical tests carried out during the hospitalization (Table 1), the possibility of SLE or systemic vasculitis was ruled out and the order of methylprednisolone pulses was canceled.
Paraclinical tests.
| Test | Result |
|---|---|
| Hemoglobin | 13.2g/dl |
| Leukocytes | 9.1mil/mm3 |
| Platelets | 318,000/mm3 |
| ANA-ENA | Negative |
| C4 | 20.9mg/dl |
| C3 | 106mg/dl |
| Anti-native DNA antibodies | Negative |
| Anticardiolipin IgG antibodies | 5.8 GPL U/ml |
| Anticardiolipin IgM antibodies | 7.4 MPL U/ml |
| Lupus anticoagulant | Negative |
| Cryoglobulins | Negative |
| Creatinine | 0.63mg/dl |
| ESR | 6mm/1h |
ANA: antinuclear antibodies; C3-C4: complement; ENA: extractable nuclear antibodies; ESR: erythrocyte sedimentation rate.
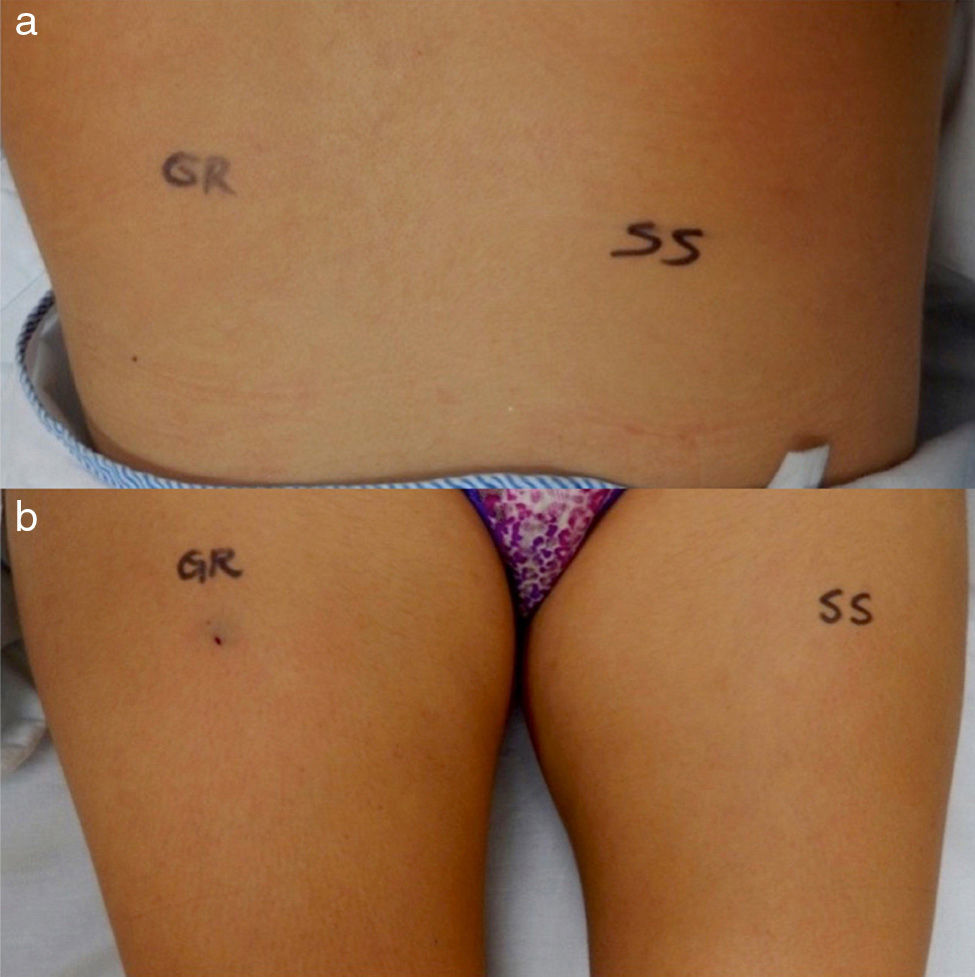
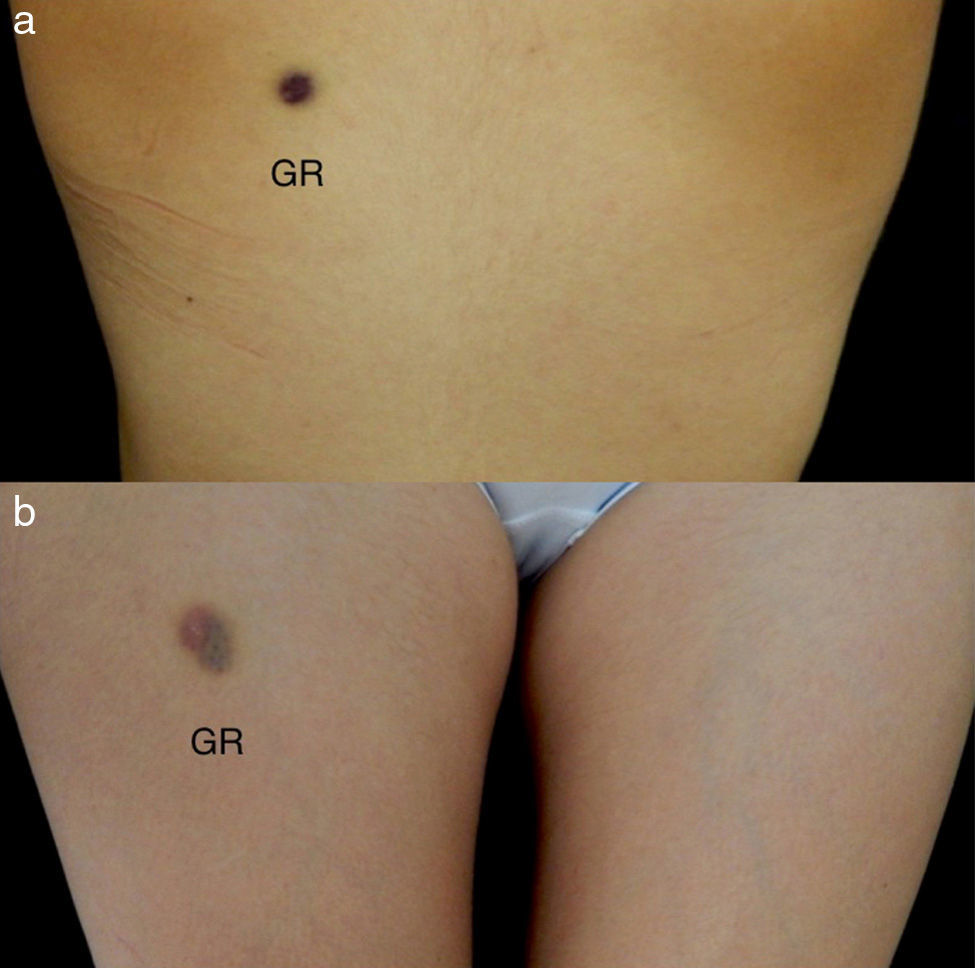
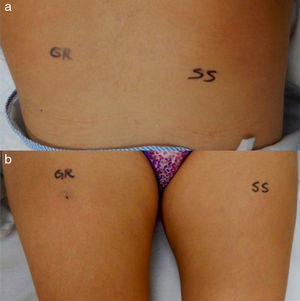
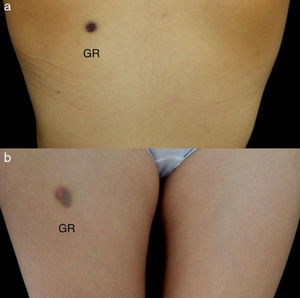
In view of the negativity of the studies and the presence of extravasated erythrocytes in the skin biopsy, without evidence of panniculitis, the Gardner-Diamond syndrome or psychogenic purpura was raised as a diagnostic possibility. An intradermal sensitization test with washed autologous erythrocytes was performed as follows: 0.1ml of washed autologous erythrocytes was injected in the left scapula and 0.1ml of 0.9% saline solution as a control in the right scapula; in addition is was injected 0.1ml of washed autologous erythrocytes in the right thigh and 0.1ml of 0.9% saline solution in the left thigh (Fig. 3a and b), with control at 3 and 24h to evaluate the response, being considered for the diagnosis of psychogenic purpura a positive subcutaneous test at 48h (Fig. 4a and b).
Since the diagnosis of psychogenic purpura is, in many occasions, of exclusion, additional studies were performed in order to rule out hematological alterations that would explain the cutaneous manifestations. All these studies were normal (Table 2). It was started topical management with 2% vitamin K and progressive clearing of the prednisone that she was receiving. The patient was reevaluated 12 days after the hospital discharge, observing residual palpable nodules and violaceous macules in the forearms, without lesions in the lower limbs or appearance of new lesions.
When the patient was reinterrogated, she reported that the lesions usually appeared after mild traumas or events that generated psychological stress; 2 years ago, after carpal tunnel release surgery she had presented the same lesions (ecchymosis), in areas distant from the surgical sites, which were self-limiting over time. On the other hand, previously to this hospitalization, she reported psychosocial events of family nature which generated marked emotional stress. She was evaluated by Psychiatry, which confirmed the previous findings and prescribed sertraline.
DiscussionThe first descriptions of the Gardner-Diamond syndrome were made at the beginning of the 20th century,3 being the first in 1955, when Gardner and Diamond described 4 adult women with painful ecchymotic lesions, reproducible after an intradermal injection of autologous red blood cells.3–5 Later, in 1968, Agle and Ratnoff observed the psychological factors that underlie the disease, changing the name to psychogenic purpura syndrome.1,5
It is an extremely rare disorder. Only about 162 cases have been described in the world literature until the year 2009.3 The majority of cases are diagnosed in women under 30 years of age and only 5% of them occur in the male gender; the symptoms tend to develop after severe stress, emotional trauma, mental illness, minor trauma or surgery.2,5,6 However, it has been not possible to identify the origin of the syndrome.2,5,7,8
Among the postulated etiological mechanisms, it has been raised the possibility of an autoimmune vasculopathy due to autosensitization to phosphatidylserine, a phosphoglyceride of the cell membrane, a component of the stroma of the erythrocytes2–4; however, this theory has not been proven.5,9 Other pathophysiological mechanisms proposed have taken into account the stress response in these patients, in whom it has been associated with an increase in glucocorticoids and catecholamines, which would eventually lead to alterations in the hemostatic mechanisms such as fibrinolysis. In addition, there is evidence that in this disease the local activity (at the cutaneous level) of the tissue plasminogen activator is increased, which would lead to an increased local plasmin activity, with rapid degradation of the fibrin clots, resulting in subcutaneous bleeding.10–12
The Gardner-Diamond syndrome consists in a localized cutaneous reaction characterized by painful, single or multiple, poorly defined erythematous plaques, found most frequently in the trunk and the upper and lower limbs (especially on the ventral surface), that progress into ecchymosis in the next 24h.1,3,13,14 There is often a prodrome in the form of local paresthesia and burning sensation a few hours before the onset of the symptoms, followed by cutaneous induration and finally, after 4–5h, appearance of erythematous plaques that evolve slowly into ecchymosis, disappearing completely in 7 to 10 days without leaving scars or residual pigmentation.1–3,5,15
The psychological evaluation of these patients may show hysterical, masochistic, depressive or anxiety traits; usually considered as a borderline personality disorder. It should be noted that some patients do not demonstrate any predominant psychopathological syndrome.1,3
Besides the psychogenic and cutaneous symptoms, systemic symptoms may occur, such as gastrointestinal symptoms (abdominal pain, diarrhea, nausea and emesis) in more than half of the patients; disorders in the menstrual cycle (up to 80% of the affected women experience profuse menstrual cycles); external hemorrhages (epistaxis, gastrointestinal bleeding and otorrhagia); and non-specific symptoms such as chest pain, headache, arthralgia and fever; which in many occasions oblige the clinician to consider an infinite number of diagnostic possibilities.1,2,6,7,9,10
Even though there is not a specific laboratory test and the diagnosis is made by exclusion, it has been considered that a positive test with intradermal injection of a 80% solution of washed autologous erythrocytes can corroborate the diagnosis; although the usefulness of this test remain controversial, given the lack of knowledge regarding its sensitivity and specificity.2,5
In this test, a positive result is considered if there is immediate pruritus and erythema around the injection site with further development (in the next 48h), of a typical lesion, however, it is clear that a negative result does not rule out the diagnosis.1–3 The hematologic studies, including the coagulation parameters, should be normal.1,2,4
Although the skin biopsy is not mandatory and usually shows non-specific changes; when is performed, it evidences an epidermis without changes with extravasated dermal erythrocytes in the absence of changes suggestive of vasculitis, with edema and a nonspecific perivascular lymphohistiocitary infiltrate and with less dermal infiltration. The macrophages may contain pigment that stains positive for iron.2,14 There is absence of leukocytoclastic vasculitis or fibrinoid degeneration of blood vessels.2,3,14
In definitive, the diagnosis is based on the anamnesis, taking into account the presence of an episode of physical or psychological trauma before the development of the symptoms, in combination with typical cutaneous lesions, being a diagnosis of exclusion, based on the history and the physical examination of the patient.7 In difficult cases, the diagnosis may require multidisciplinary management with other specialties such as Psychiatry or Hematology, mainly, to rule out other causes which are potentially fatal for the patient.3,7
The differential diagnosis includes a wide variety of disorders such as: disseminated intravascular coagulation, idiopathic thrombocytopenic purpura, anaphylactoid purpura, Von Willebrand disease, factor XIII deficiency, antiphospholipid syndrome, SLE, Ehlers–Danlos syndrome, dermatitis artefacta, cellulitis, Munchausen syndrome, compartment syndrome, and spontaneous panniculitis. The use of some drugs such as steroids and selective serotonin reuptake inhibitors is also part of the conditions to rule out in this group of patients.2,3,8,9 In the case of steroids, it can be present like purpura, which usually appears with photosensitivity in areas exposed to the sun, but without edema or pain; our patient, despite the chronic intake of steroids, did not have areas of photosensitivity and her lesions were very painful and with great soft tissue edema. The selective serotonin reuptake inhibitors may induce bleeding episodes related with the inhibition of platelet aggregation, due to the effect of these drugs on the decrease of intraplatelet serotonin concentrations.16
Unfortunately, in the majority of patients reported with Gardner-Diamond syndrome, the results of the tests for a primary hemostatic disorder are not available; therefore, its prevalence in this population of patients is completely unknown.17
The prognosis depends on the severity of the factitious symptoms.15 The disease follows an intermittent and irregular course with a variable response to treatment; in the majority of cases the remissions may be of long-term, being reported in the literature free-relapse periods of up to 38 years.1,3,9 Psychotherapy is more effective when is started early during the course of the disease.1,3 Likewise, some psychotropic drugs (amitriptyline and levomepromazine) have been prescribed with success.3,18 Other therapeutic options include the use of antidepressants, especially selective serotonin reuptake inhibitors, which besides their mechanism of action, exert and antihistamine and anticholinergic effect that could lead to an improvement of the symptoms in the patients5; the use of antihistamines could also be recommended, and topical management with corticosteroids or vitamin K has been used, but it has been seen that their effect is similar to placebo.3,8
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare they do not have any conflict of interest.
Please cite this article as: Santos Estrada J, Rivera Toquica FE, Muñoz-Grajales C, Velásquez Franco CJ, Márquez Hernández JD, Pinto Peñaranda LF. Síndrome de Gardner-Diamond como diagnóstico diferencial de lupus. Rev Colomb Reumatol. 2016;23:195–199.