To present current clinical experience and the clinical outcomes in the management of patients with adult Still disease.
Materials and methodsA retrospective study of a case series was conducted on of 17 cases diagnosed with adult Still disease during a period between 2009 and 2014 in 2 tertiary hospitals in Santiago de Cali.
ResultsOf the 17 cases diagnosed and treated, it was found that 50% of patients had an elevated ferritin five times its normal value, being useful in the diagnosis. Less than 50% of cases were under 40 years, and about 50% of the population required combined treatment, with two patients requiring biological therapy to control their symptoms. Yamaguchi criteria were used for diagnostic correlation.
ConclusionsAdult Still's disease is a rare disease that requires a high index of suspicion, but it must be a disease to rule out, and it always requires management generally combined with schemes to improve the quality of life of patients.
Dar a conocer la experiencia clínica en el mundo real y los resultados clínicos del manejo de los pacientes con enfermedad de Still del adulto.
Materiales y métodosSe realiza un estudio retrospectivo de serie de casos, de 17 casos con diagnóstico de enfermedad de Still del adulto, en 2 clínicas de nivel 3 de Santiago de Cali, Colombia, en el periodo comprendido entre 2009 y 2014.
ResultadosDe los 17 casos diagnosticados y tratados se encontró que en el 50% de los pacientes había una elevación de ferritina de 5 veces su valor normal, siendo útil en el diagnóstico, menos del 50% de los casos fueron en menores de 40 años, alrededor del 50% de la población requirió tratamiento combinado y 2 pacientes requirieron terapia biológica para el control de sus síntomas. Se usaron los criterios de Yamaguchi para la correlación diagnóstica.
ConclusionesLa enfermedad de Still del adulto es una enfermedad rara que requiere alto índice de sospecha pero debe ser una enfermedad de descarte y, generalmente, siempre requiere manejo con esquemas combinados para mejorar la calidad de vida del paciente.
Adult Still's disease (ASD) is an uncommon systemic disease of unknown etiology and inflammatory characteristics, with a broad spectrum of clinical presentations. There are no epidemiological data on its incidence or prevalence, and there is not a pathognomonic diagnostic test; given its behavior and the lack of diagnostic tests is considered a diagnosis by exclusion. Various criteria have been proposed for its diagnosis, including those of Yamaguchi that allow an accurate diagnostic approach.1
The pathophysiology of ASD is still not fully understood. Numerous causes such as infectious agents, genetic factors and alteration in the regulation of the immune response and the apoptosis have been postulated, but there are still not concrete data.2–6 The postulated infectious agents, based on temporal relationships between the onset of the disease and the serological evidence, are parvovirus B19, rubella, echovirus 7, Epstein–Barr, cytomegalovirus, Coxsackie B4, Chlamydia and Yersinia; however, it has not been possible to establish a definitive relationship.2
The immunological pathways of the disease have been considered the most significant in the pathophysiology. The studies have demonstrated that the proinflammatory interleukins (IL) play a vital role in the pathogenesis7,8 and elevated levels of IL-1 have been detected in the untreated disease, which has been correlated with the disease activity and severity.9 Likewise, this acute phase response is considered the responsible for the stimulation of the synthesis of ferritin and, particularly, the IL-18 favors such stimulation and plays an important role in the manifestations of the disease, by correlating with the levels of neutrophils in blood.10
The main manifestations of the disease are intermittent fever predominantly in the evenings, usually for less than 4h, associated with evanescent salmon colored maculopapular rash on the trunk and extremities. It can be accompanied by joint commitment that involves mainly the wrists, knees and ankles, although whichever joint may be affected, it also tends to be symmetrical and bilateral. In addition, it may occur odynophagia, hepatosplenomegaly and serious manifestations such as pleuropericarditis, pleural effusion and interstitial pneumonitis.11,12 Paraclinically, it may occur with leukocytosis and neutrophilia in more than 80% of cases, alterations of liver function tests, elevation of ferritin up to 5 times the normal upper value and elevation of glycosylated ferritin. The blood cultures and autoimmunity tests are negative.13 Several classification criteria had been used, being those of Yamaguchi the most commonly used given their sensitivity (93%). Other recognized criteria are those of Cush and Fautrel with a sensitivity of 80% for both.11
A series of 17 cases diagnosed in the city of Santiago de Cali, in 2 centers of level 3 of the city, is presented. The clinical description of the patients and the diagnostic method is made, and is also described how was the treatment of the patients and the results previously obtained. The lack of evidence, due to the low prevalence of the disease, motivates the realization of this type of case series for a better understanding of the behavior of the disease in our population.
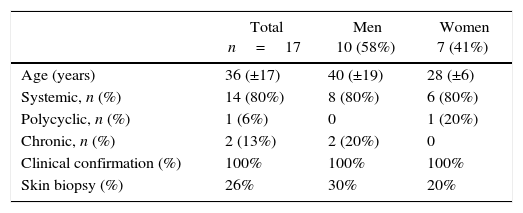
Materials and methodsRetrospective study of a case series. 17 cases with diagnosis of ASD based on Yamaguchi's criteria, in 2 clinics of level 3 of Santiago de Cali, in the period between 2009 and 2014 (15 from the Imbanaco Medical Center and 2 from the Comfenalco Valle Unilibre Corporation). The age, the gender, the clinical classification, the time elapsed between the onset of the symptoms and the diagnosis, the treatment used, and the clinical and laboratory characteristics are analyzed. Only the percentages were used for the analyses (Table 1).
Clinical characteristics of the patients who were studied in the article.
| Total n=17 | Men 10 (58%) | Women 7 (41%) | |
|---|---|---|---|
| Age (years) | 36 (±17) | 40 (±19) | 28 (±6) |
| Systemic, n (%) | 14 (80%) | 8 (80%) | 6 (80%) |
| Polycyclic, n (%) | 1 (6%) | 0 | 1 (20%) |
| Chronic, n (%) | 2 (13%) | 2 (20%) | 0 |
| Clinical confirmation (%) | 100% | 100% | 100% |
| Skin biopsy (%) | 26% | 30% | 20% |
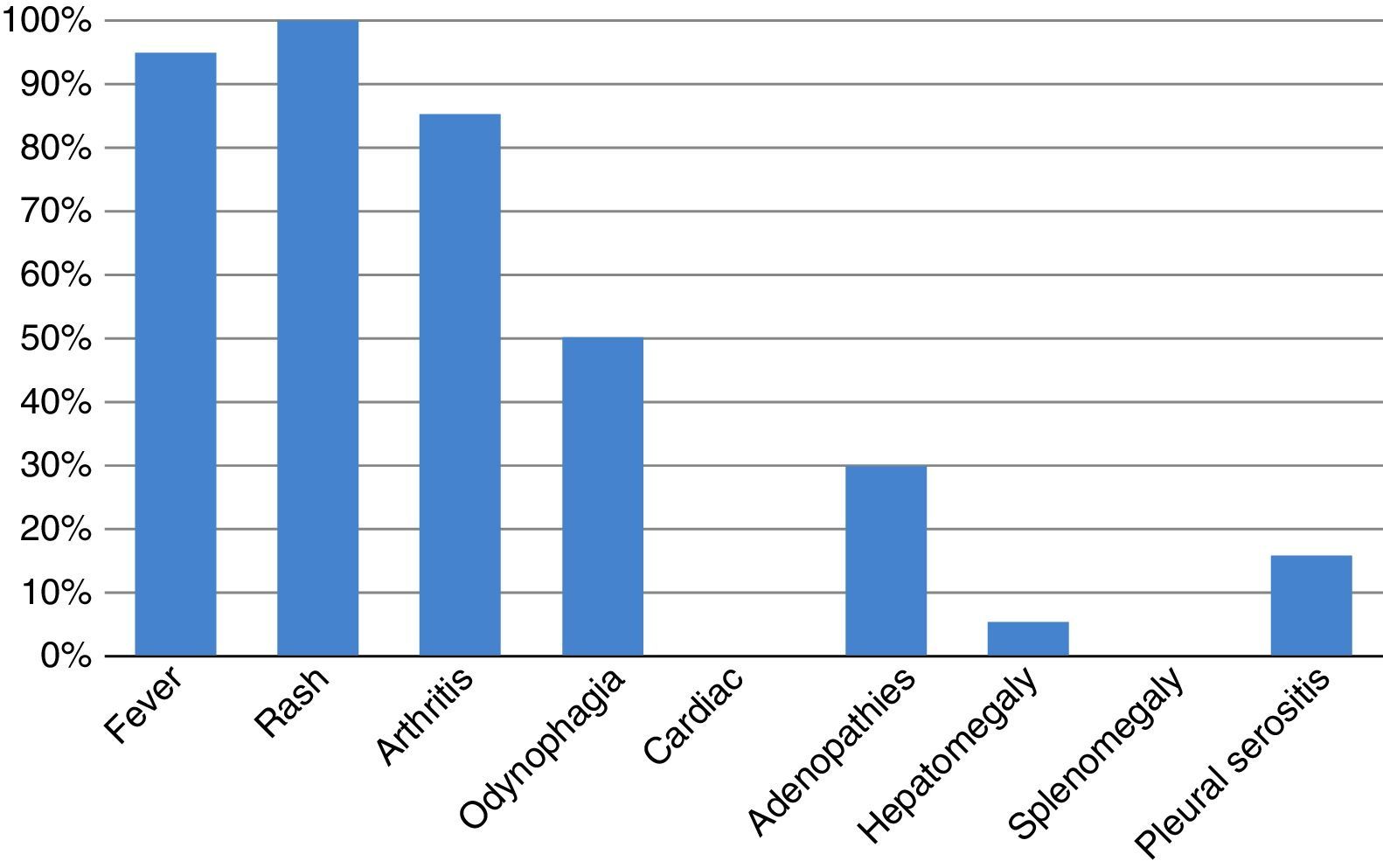
The curse of the disease had an approximated duration of 40 days between the onset of the symptoms and the diagnosis. The cases of rapid diagnosis were linked to a more timely consultation to a rheumatologist. 95% of patients had fever, all since the beginning of the disease. All patients had the characteristic skin rash. 86% of patients presented joint involvement at some point of the disease, generally associated with the febrile episodes. Half of the patients had odynophagia and 30% of the total had palpable adenopathies on the physical examination. Only one patient had hepatomegaly with transient alteration of the liver function tests (Fig. 1).
Laboratory characteristics of the patientsThe vast majority of patients (93%) exhibited leukocytosis with neutrophilia (≥10,000leukocytes/mm3, ≥80% neutrophils), without having a clear correlation with an alteration in the level of platelets. The acute-phase reactants (sedimentation rate, C-reactive protein) are characterized by being elevated in 86% of patients. All patients had negative autoantibodies. 80% of patients were cultivated without having isolated any germ. A skin biopsy was performed in 26% of patients, processed in the same laboratory, whose results shows an inflammatory reaction with no germ identified in the specimens.
TreatmentAll patients received steroids as the basis of the medical treatment with adequate response. Nonsteroidal anti-inflammatory drugs were used in half of the patients with a limited response. It should be mentioned that a standard scheme was not used. No patient received monotherapy. 50% of patients received treatment with steroids, methotrexate and hydroxychloroquine with adequate response. 33% of patients were managed with steroids and hydroxychloroquine, likewise, with good response. It cannot be stated that one therapeutic scheme is better than another, since it is not the priority of the present text, and there are no bioequivalence studies, but we can say that the combined scheme made the difference. Only one of the patients used biologic therapy as a first line treatment, without prior use of other therapeutic scheme, with which there was an improvement in the symptoms. The choice among the different therapeutic schemes by each rheumatologist was based in the degree of involvement of the disease at the time of diagnosis.
DiscussionWe describe a series of 17 cases of ASD of adult onset. The most prevalent symptoms were fever, maculopapular rash and polyarthralgia; regarding the paraclinical findings, the most prevalent were leukocytosis with neutrophilia, elevated acute-phase reactants and hyperferritinemia. Yamaguchi's criteria were met in the majority of our patients, suggesting that they are the most appropriate, as it has been mentioned in previous studies.14 It is worth highlighting the importance of ferritin in the diagnosis and follow-up along different studies,15,16 in our series was evidenced that in more than 50% of the patients, a value higher than the normal was present; since they have not been validated yet as a part of the diagnostic method, it has been suggested that they might be guiding tools.
Just as mentioned in the different series of cases that talk about the treatment in this pathology,17,18 management with steroids was started in 100% of patients, with which the remission of the symptoms was achieved; however, in order to maintain the remission of the condition, disease modulating drugs were used in combination in 50% of the patients, since the remission expected and commented in studies of 76% was not achieved when they were used as monotherapy. Another type of modulating drugs such as leflunomide, azathioprine, cyclosporine and mycophenolate was not administered. On the other hand, in those patients with more severe presentation it was decided to start treatment with biologic therapy with tocilizumab, in one as first line due to the severity of the symptoms and in other due to therapeutic failure with hydroxychloroquine, leflunomide and prednisolone, since it was not possible to reduce the dose of prednisolone below 15mg/day. When comparing the results with tocilizumab, which has been evaluated in other series of cases and in an open, multicenter, retrospective study,19,20 with ours, similar results were found after failures with first-line drugs; although we know that it is not the biological therapy of first choice, it was not possible to use anakinra because of the lack of availability in our country.21
In our country it was conducted a series of cases that shows that there are patients who have atypical forms of presentation and with greater systemic involvement,22 however, when comparing such results with our series we found that there is not much similarity in the frequency of appearance of severe presentations and we believe that the course of the disease tends to be more benign given the form of presentation in our series of cases. This could be explained because the sites from where the patients were taken are of high complexity and receive the most severe cases.
There are no controlled and randomized clinical trials evaluating the treatment of this disease and the information we have comes from observational studies; for this reason, we consider that the definitive therapeutic guideline should be done with 2 disease modulating drugs and, according to the presentation and severity of the symptoms, biologic therapy should be started in order to achieve a complete remission of the disease. In our environment, the medication to be started would be tocilizumab; however, we emphasize that anakinra would be the ideal drug.
ConclusionASD is an infrequent pathology that represents a major diagnostic challenge in the context of fever of unknown origin; it is important to have a high index of suspicion but it should be a diagnosis by exclusion. Since this disease is rare, there are not enough epidemiological studies to characterize its global prevalence and incidence. An adequate medical history, a good physical examination, a good differential diagnosis and the application of the clinical and paraclinical criteria are required to be able to reach the diagnosis and start the appropriate treatment with a combined scheme, usually, in order to improve the quality of life of the patient.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
FundingThe authors did not receive any funding for the elaboration of this manuscript.
Conflict of interestThe authors declare that they have no conflict of interest.
To the Imbanaco Medical Center and the Comfenalco Valle Unilibre Corporation, which are the places from where the information of the patients was obtained.
Please cite this article as: Muriel R. ÁJ, Rueda G. JM, Buriticá HG, Castaño C. O. Una patología poco frecuente: la enfermedad de Still del adulto. Experiencia clínica con 17 casos. Rev Colomb Reumatol. 2016;23:126–130.