It is known that non-adherence to psychiatric medications has harmful consequences for both patients and society.
ObjectiveTo collect information on the incidence of non-adherence, and the factors and causes affecting adherence to psychopharmacological treatment in patients with severe and persistent mental disorders.
MethodsA systematic review of scientific articles on adult patients (>17 years) published in the last five years (2015–2020) on specialised databases such as PubMed, Scopus, Scielo and BioMed. Original articles from indexed journals with an impact factor >0.5, in English or Spanish, with an analytical, prospective, retrospective, cross-sectional and randomised design were included. Once the articles were identified, they were analysed, extracting the information necessary to answer the research questions.
ResultsFifteen articles were included. Of these, 40% (n = 6) were published in 2020, 20% (n = 3) were produced in China and 53.3% (n = 8) had an observational design. A total of 5,837 patients were included, of which 50.6% were men (n = 2,955), with moderate adherence (n = 10; 66.7%) reported in 10 investigations. Non-adherence varies from 7.7% to 60.6%. The factors that affect adherence are specific to the patient (age and sex), their family support network, and related to the disease or the treatment. The main cause of non-adherence is lack of insight.
ConclusionsAdherence to treatment with psychotropic drugs is multifactorial. Access to mental health services should be improved, with an emphasis placed on patient education and providing greater knowledge of mental illness. Interventions to promote education and interaction with the psychiatrist could be beneficial.
Se sabe que la falta de adherencia a los medicamentos psiquiátricos tiene consecuencias perjudiciales tanto para los pacientes como para la sociedad.
ObjetivoRecopilar información sobre la incidencia de falta de adherencia, los factores y las causas que afectan a la adherencia al tratamiento psicofarmacológico de los pacientes con trastornos mentales graves y persistentes.
MétodosRevisión sistemática de artículos científicos en pacientes adultos (edad > 17 años), publicados en los últimos 5 años (2015-2020) en bases de datos especializadas como PubMed, Scopus, Scielo y BioMed. Se incluyeron artículos de revistas indexadas con factor de impacto > 0,5 en inglés o español, originales, con diseño analítico, prospectivo, retrospectivo, transversal y aleatorizados. Una vez identificados los artículos, se procedió a su análisis, extrayendo la información necesaria para responder las preguntas de investigación.
ResultadosSe incluyeron 15 artículos, el 40% (n = 6) publicados en 2020, el 20% (n = 3) realizados en China y el 53,3% (n = 8) de diseño observacional. Se incluyó una población total de 5.837 pacientes, varones el 50,6% (n = 2.955). Reportaron adherencia moderada 10 investigaciones (66,7%). La falta de adherencia varía desde el 7,7 al 60,6%. Los factores que afectan a la adherencia son propios del paciente (edad y sexo) o su red de apoyo familiar, relacionados con la enfermedad o el tratamiento. La principal causa de la falta de adherencia es la ausencia de insight.
ConclusionesLa adherencia al tratamiento con psicofármacos es multifactorial. Se debería mejorar el acceso a los servicios de salud mental, poner énfasis en la formación del paciente y aportar mayor conocimiento de la enfermedad mental; la formación y la interacción con el psiquiatra podrían ser intervenciones beneficiosas.
Serious mental disorders include a group of illnesses with obvious psychotic symptoms and severe impairment of social life, such as schizophrenia and related conditions, bipolar disorder and depression.1 People with severe and persistent mental disorders have an average mortality rate 2–3 times higher than the general population, which translates into a reduction in life expectancy of 10 to 20 years.2
Most patients require long-term treatment and care, which seriously affects their quality of life and productivity and that of their families. The disease burden is high due to its high incidence, recurrence rate and disability rate.3
Adherence to antipsychotic medication is essential for the treatment of patients with severe and persistent mental disorders.4 A low degree of acceptance of the illness has been associated with non-adherence to medication, resulting in negative clinical outcomes.5
Medication non-adherence is a major public health problem. According to the World Health Organization (WHO), “medication adherence can be defined as the degree to which a patient’s use of medication corresponds to the prescribed regimen”.6 In this sense, it should be considered as a variety of behaviours that range from complete adherence to medication (that comply 100% with medical instructions), to partial adherence (that comply with only part of the medical instructions), to complete non-adherence.
Non-adherence to psychiatric medications is known to have detrimental consequences for both patients and society, including increased symptom severity, relapses, hospital readmissions, suicides and reduced quality of life. Its consequences for society are mainly due to patients’ loss of income and high healthcare costs.7
When examining non-adherence, to address it appropriately, it is vital to understand the underlying factors. Among the main related factors are lack of knowledge, shorter duration of the illness, negative attitudes toward medication, lack of social support, and side effects of the medication.8 Internalised stigma, a process by which individuals with mental illness apply negative stereotypes to themselves, is another well-studied factor that affects adherence, as it makes patients feel ashamed and prefer not to take their medication to avoid being called “mentally ill”.8
Taking this into account, our aim with this study was to collect information on the incidence of non-adherence and the factors and causes that affect adherence to psychopharmacological treatment in patients with severe and persistent mental disorders. As the negative effect of non-adherence on these patients is well-known, we believe it is important that all the best evidence is available to all healthcare workers in psychiatry, to help identify the factors involved in treatment adherence and implement suitable measures.
Furthermore, this research is necessary because the evidence on factors that positively or negatively impact adherence to pharmacological treatment in patients with severe mental disorders needs to be updated and systematised.8 What we already know is that these patients have poor adherence to pharmacological treatment and that non-adherence is associated with a worse clinical prognosis, worse socio-family functioning, greater dependency and worse quality of life.9
MethodsSystematic review of scientific articles that meet the inclusion and exclusion criteria. We used the PubMed, Scopus, Scielo, Latindex, DOAJ (Directory of Open Access Journals), BioMed Research International and Google Scholar medical information search engines. The following keywords were taken into account: "Schizophrenia "[Mesh]// "Bipolar disorder" [Mesh] // "Depressive disorder" [Mesh]// "Severe mental illness" [Mesh] // "Severe Mental Disorders" [Mesh] // "Psychiatric Diseases" [Mesh] // "Serious mental illness" [Mesh] // AND "Adherence, Medication" [Mesh] // "Non-adherence, Medication" [Mesh] // "Noncompliance, Medication" [Mesh] // "Treatment abandonment" [Mesh] // "Therapeutic Adherence and Compliance" [Mesh] "Therapeutic Adherence" [Mesh] // AND "Risk factors" [Mesh] "Associated factors" [Mesh] // "Causes" [Mesh] // Spanish (lang) OR English (lang).
The inclusion criteria were scientific articles from journals indexed with an impact factor of >0.5, in English and Spanish, published in the last five years (2015–2020), complete, with adult patients (age >17 years), original, with analytical, prospective, retrospective, cross-sectional and randomised design.
The exclusion criteria were: paid publications, case reports, conference proceedings, letters to the editor, degree thesis, articles without a declaration of conflicts of interest, without bioethical considerations, with SACKETT IV level of evidence, compliance rate with the STROBE, CONSORT and PRISMA-p checklist <75%.
To avoid the risk of bias, a systematic search for evidence was carried out, following the aforementioned inclusion and exclusion criteria. The presence of different types of bias was assessed: selection, performance, detection and attrition or notification, using the tool proposed by Cochrane.10 To analyse the quality of the evidence, GRADE11 methodology was followed, with which the quality of the evidence was summarised and evaluated, and displayed in an evidence summary table.
The association measures are mean ± standard deviation, frequencies and percentages, risk estimation and I2 test.
PICOT strategy: P (patients with severe and persistent mental disorders), I (causes of non-adherence to psychopharmacological treatment), C (causes of adherence to psychopharmacological treatment), O (factors that affect adherence to psychopharmacological treatment of patients with severe and persistent mental disorders) and T (not applicable).
Research questionsWhat is the prevalence of non-adherence to psychopharmacological treatment in patients with serious mental disorders?
What factors affect adherence to psychopharmacological treatment in patients with serious and persistent mental illnesses?
What are the causes of non-adherence to psychopharmacological treatment in patients with serious mental disorders?
A search was carried out in specialised databases using the keywords [MESH terms], and open-access articles were downloaded for further analysis. This search was carried out over a period of four weeks. A record of the traceability of the articles was kept in a table that includes the URL, keywords used, and search engine where it was found.
Later, the evidence was classified to determine whether the inclusion and exclusion criteria were met. After selecting the articles, the analysis began taking into account aspects such as: article title; authors/year/country; objective/design; population description (number of participants, by gender, diagnosis and age); intervention carried out; and results. We then carried out an analysis and discussion of the information collected from the reviewed articles and prepared the final report of the systematic review.
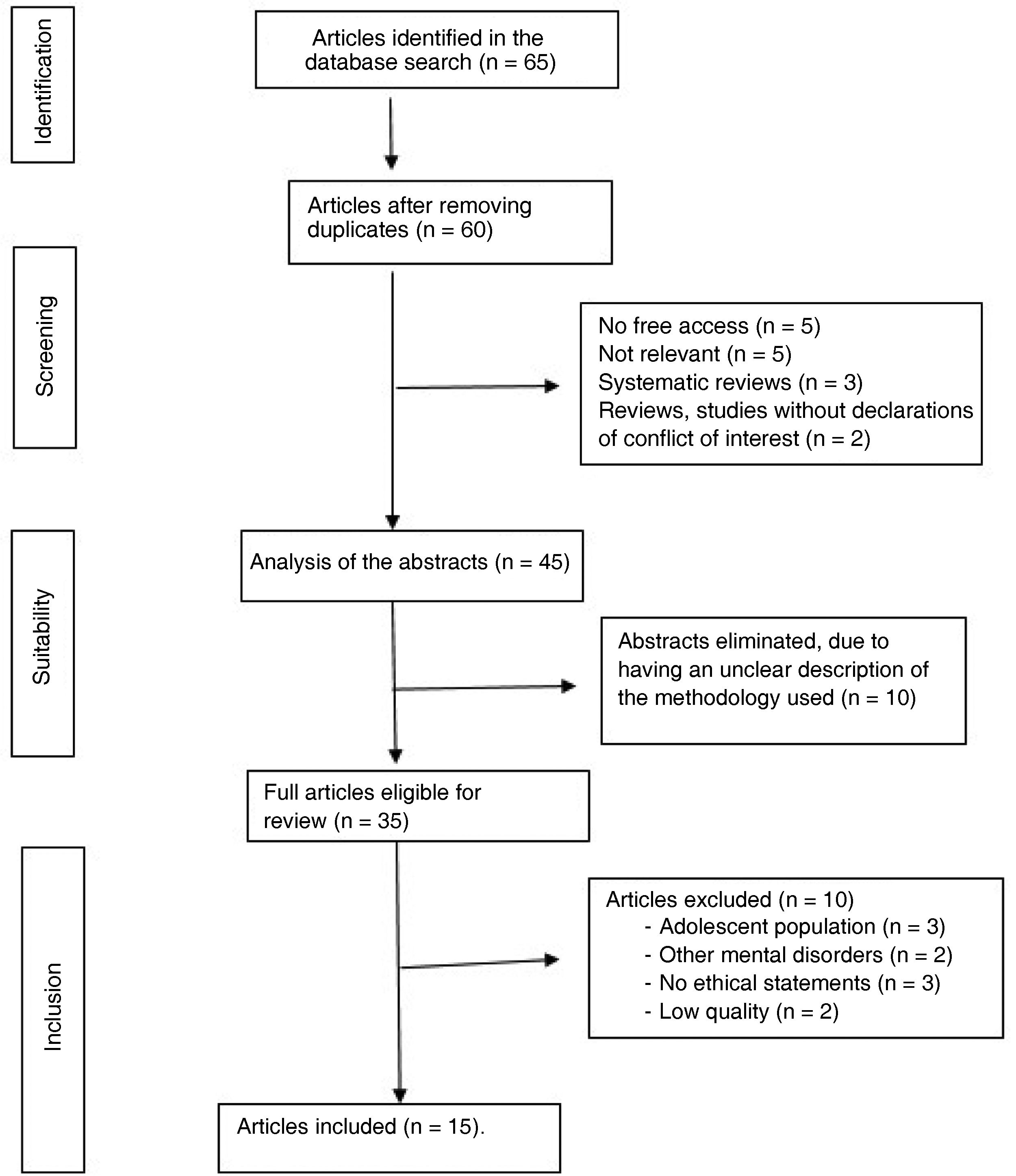
ResultsDescription of the articles selectedIn the search conducted by the lead author in the different specialised data sources, 65 articles were identified, from which we eliminated five duplicate, paid and non-relevant articles respectively, three systematic reviews and two that did not have conflict of interest declarations. Both authors performed the classification, in which the abstracts of 45 articles were analysed; 10 were eliminated for not having a clear description of the methodology followed, three for having included patients under 18 years of age, two for dealing with other mental disorders, three for not having ethical statements and two for being publications of low quality. At the end of this review process, 15 articles remained, which were included in this research by both authors.
The search, classification and review of the evidence was carried out at various times in a joint effort by the two authors. Fig. 1 shows the PRISMA12 flow chart, which depicts the article selection process. At the end of this selection process, 15 articles remained which were included in the review. Once selected, the articles were analysed (Table 1).
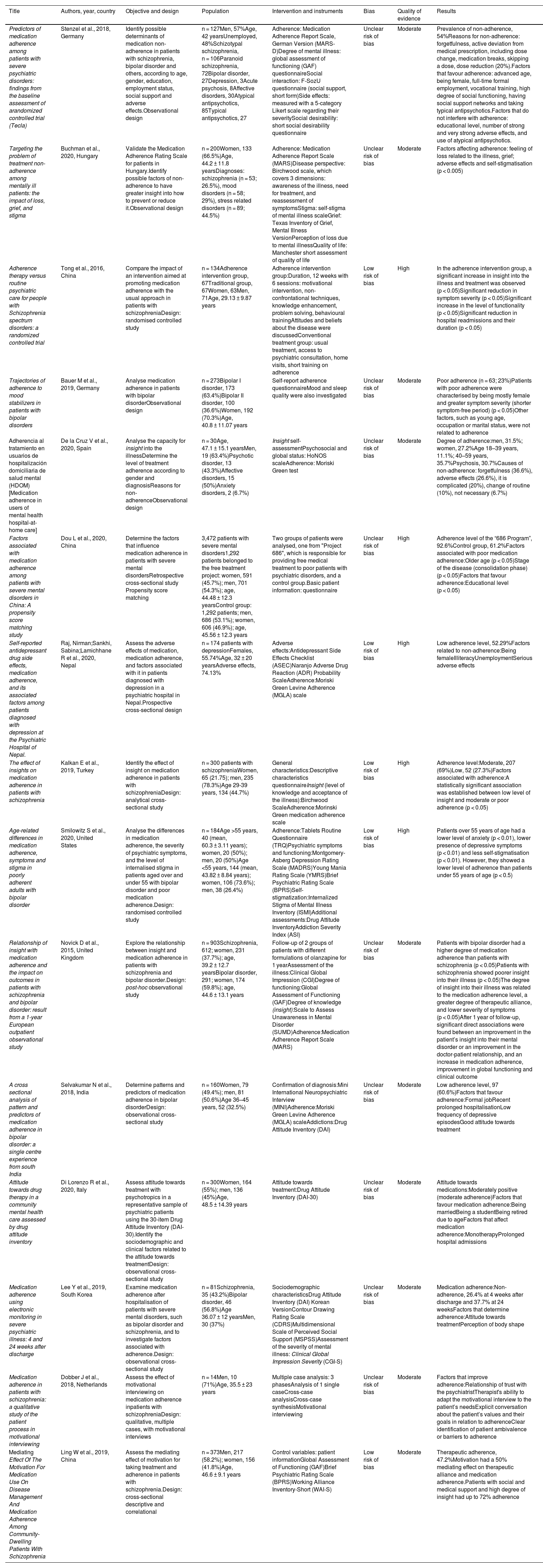
Analysis of the articles selected.
| Title | Authors, year, country | Objective and design | Population | Intervention and instruments | Bias | Quality of evidence | Results |
|---|---|---|---|---|---|---|---|
| Predictors of medication adherence among patients with severe psychiatric disorders: findings from the baseline assessment of arandomized controlled trial (Tecla) | Stenzel et al., 2018, Germany | Identify possible determinants of medication non-adherence in patients with schizophrenia, bipolar disorder and others, according to age, gender, education, employment status, social support and adverse effects.Observational design | n = 127Men, 57%Age, 42 yearsUnemployed, 48%Schizotypal schizophrenia, n = 106Paranoid schizophrenia, 72Bipolar disorder, 27Depression, 3Acute psychosis, 8Affective disorders, 30Atypical antipsychotics, 85Typical antipsychotics, 27 | Adherence: Medication Adherence Report Scale, German Version (MARS-D)Degree of mental illness: global assessment of functioning (GAF) questionnaireSocial interaction: F-SozU questionnaire (social support, short form)Side effects: measured with a 5-category Likert scale regarding their severitySocial desirability: short social desirability questionnaire | Unclear risk of bias | Moderate | Prevalence of non-adherence, 54%Reasons for non-adherence: forgetfulness, active deviation from medical prescription, including dose change, medication breaks, skipping a dose, dose reduction (20%).Factors that favour adherence: advanced age, being female, full-time formal employment, vocational training, high degree of social functioning, having social support networks and taking typical antipsychotics.Factors that do not interfere with adherence: educational level, number of strong and very strong adverse effects, and use of atypical antipsychotics. |
| Targeting the problem of treatment non-adherence among mentally ill patients: the impact of loss, grief, and stigma | Buchman et al., 2020, Hungary | Validate the Medication Adherence Rating Scale for patients in Hungary.Identify possible factors of non-adherence to have greater insight into how to prevent or reduce it.Observational design | n = 200Women, 133 (66.5%)Age, 44.2 ± 11.8 yearsDiagnoses: schizophrenia (n = 53; 26.5%), mood disorders (n = 58; 29%), stress related disorders (n = 89; 44.5%) | Adherence: Medication Adherence Report Scale (MARS)Disease perspective: Birchwood scale, which covers 3 dimensions: awareness of the illness, need for treatment, and reassessment of symptomsStigma: self-stigma of mental illness scaleGrief: Texas Inventory of Grief, Mental Illness VersionPerception of loss due to mental illnessQuality of life: Manchester short assessment of quality of life | Unclear risk of bias | Moderate | Factors affecting adherence: feeling of loss related to the illness, grief; adverse effects and self-stigmatisation (p < 0.005) |
| Adherence therapy versus routine psychiatric care for people with Schizophrenia spectrum disorders: a randomized controlled trial | Tong et al., 2016, China | Compare the impact of an intervention aimed at promoting medication adherence with the usual approach in patients with schizophreniaDesign: randomised controlled study | n = 134Adherence intervention group, 67Traditional group, 67Women, 63Men, 71Age, 29.13 ± 9.87 years | Adherence intervention group:Duration, 12 weeks with 6 sessions: motivational intervention, non-confrontational techniques, knowledge enhancement, problem solving, behavioural trainingAttitudes and beliefs about the disease were discussedConventional treatment group: usual treatment, access to psychiatric consultation, home visits, short training on adherence | Low risk of bias | High | In the adherence intervention group, a significant increase in insight into the illness and treatment was observed (p < 0.05)Significant reduction in symptom severity (p < 0.05)Significant increase in the level of functionality (p < 0.05)Significant reduction in hospital readmissions and their duration (p < 0.05) |
| Trajectories of adherence to mood stabilizers in patients with bipolar disorders | Bauer M et al., 2019, Germany | Analyse medication adherence in patients with bipolar disorderObservational design | n = 273Bipolar I disorder, 173 (63.4%)Bipolar II disorder, 100 (36.6%)Women, 192 (70.3%)Age, 40.8 ± 11.07 years | Self-report adherence questionnaireMood and sleep quality were also investigated | Unclear risk of bias | Moderate | Poor adherence (n = 63; 23%)Patients with poor adherence were characterised by being mostly female and greater symptom severity (shorter symptom-free period) (p < 0.05)Other factors, such as young age, occupation or marital status, were not related to adherence |
| Adherencia al tratamiento en usuarios de hospitalización domiciliaria de salud mental (HDOM) [Medication adherence in users of mental health hospital-at-home care] | De la Cruz V et al., 2020, Spain | Analyse the capacity for insight into the illnessDetermine the level of treatment adherence according to gender and diagnosisReasons for non-adherenceObservational design | n = 30Age, 47.1 ± 15.1 yearsMen, 19 (63.4%)Psychotic disorder, 13 (43.3%)Affective disorders, 15 (50%)Anxiety disorders, 2 (6.7%) | Insight self-assessmentPsychosocial and global status: HoNOS scaleAdherence: Moriski Green test | Unclear risk of bias | Moderate | Degree of adherence:men, 31.5%; women, 27.2%Age 18–39 years, 11.1%; 40–59 years, 35.7%Psychosis, 30.7%Causes of non-adherence: forgetfulness (36.6%), adverse effects (26.6%), it is complicated (20%), change of routine (10%), not necessary (6.7%) |
| Factors associated with medication adherence among patients with severe mental disorders in China: A propensity score matching study | Dou L et al., 2020, China | Determine the factors that influence medication adherence in patients with severe mental disordersRetrospective cross-sectional study Propensity score matching | 3,472 patients with severe mental disorders1,292 patients belonged to the free treatment project: women, 591 (45.7%); men, 701 (54.3%); age, 44.48 ± 12.3 yearsControl group: 1,292 patients; men, 686 (53.1%); women, 606 (46.9%); age, 45.56 ± 12.3 years | Two groups of patients were analysed, one from "Project 686", which is responsible for providing free medical treatment to poor patients with psychiatric disorders, and a control group.Basic patient information: questionnaire | Unclear risk of bias | High | Adherence level of the “686 Program”, 92.6%Control group, 61.2%Factors associated with poor medication adherence:Older age (p < 0.05)Stage of the disease (consolidation phase) (p < 0.05)Factors that favour adherence:Educational level (p < 0.05) |
| Self-reported antidepressant drug side effects, medication adherence, and its associated factors among patients diagnosed with depression at the Psychiatric Hospital of Nepal. | Raj, Nirman;Sankhi, Sabina;Lamichhane R et al., 2020, Nepal | Assess the adverse effects of medication, medication adherence, and factors associated with it in patients diagnosed with depression in a psychiatric hospital in Nepal.Prospective cross-sectional design | n = 174 patients with depressionFemales, 55.74%Age, 32 ± 20 yearsAdverse effects, 74.13% | Adverse effects:Antidepressant Side Effects Checklist (ASEC)Naranjo Adverse Drug Reaction (ADR) Probability ScaleAdherence:Moriski Green Levine Adherence (MGLA) scale | Low risk of bias | High | Low adherence level, 52.29%Factors related to non-adherence:Being femaleIlliteracyUnemploymentSerious adverse effects |
| The effect of insights on medication adherence in patients with schizophrenia | Kalkan E et al., 2019, Turkey | Identify the effect of insight on medication adherence in patients with schizophreniaDesign: analytical cross-sectional study | n = 300 patients with schizophreniaWomen, 65 (21.75); men, 235 (78.3%)Age 29-39 years, 134 (44.7%) | General characteristics:Descriptive characteristics questionnaireInsight (level of knowledge and acceptance of the illness):Birchwood ScaleAdherence:Morinski Green medication adherence scale | Low risk of bias | High | Adherence level:Moderate, 207 (69%)Low, 52 (27.3%)Factors associated with adherence:A statistically significant association was established between low level of insight and moderate or poor adherence (p < 0.05) |
| Age-related differences in medication adherence, symptoms and stigma in poorly adherent adults with bipolar disorder | Smilowitz S et al., 2020, United States | Analyse the differences in medication adherence, the severity of psychiatric symptoms, and the level of internalised stigma in patients aged over and under 55 with bipolar disorder and poor medication adherence.Design: randomised controlled study | n = 184Age >55 years, 40 (mean, 60.3 ± 3.11 years); women, 20 (50%); men, 20 (50%)Age <55 years, 144 (mean, 43.82 ± 8.84 years); women, 106 (73.6%); men, 38 (26.4%) | Adherence:Tablets Routine Questionnaire (TRQ)Psychiatric symptoms and functioning:Montgomery-Asberg Depression Rating Scale (MADRS)Young Mania Rating Scale (YMRS)Brief Psychiatric Rating Scale (BPRS)Self-stigmatization:Internalized Stigma of Mental Illness Inventory (ISMI)Additional assessments:Drug Attitude InventoryAddiction Severity Index (ASI) | Low risk of bias | High | Patients over 55 years of age had a lower level of anxiety (p < 0.01), lower presence of depressive symptoms (p < 0.01) and less self-stigmatisation (p < 0.01). However, they showed a lower level of adherence than patients under 55 years of age (p < 0.5) |
| Relationship of insight with medication adherence and the impact on outcomes in patients with schizophrenia and bipolar disorder: result from a 1-year European outpatient observational study | Novick D et al., 2015, United Kingdom | Explore the relationship between insight and medication adherence in patients with schizophrenia and bipolar disorder.Design: post-hoc observational study | n = 903Schizophrenia, 612; women, 231 (37.7%); age, 39.2 ± 12.7 yearsBipolar disorder, 291; women, 174 (59.8%); age, 44.6 ± 13.1 years | Follow-up of 2 groups of patients with different formulations of olanzapine for 1 yearAssessment of the illness:Clinical Global Impression (CGI)Degree of functioning:Global Assessment of Functioning (GAF)Degree of knowledge (insight):Scale to Assess Unawareness in Mental Disorder (SUMD)Adherence:Medication Adherence Report Scale (MARS) | Unclear risk of bias | Moderate | Patients with bipolar disorder had a higher degree of medication adherence than patients with schizophrenia (p < 0.05)Patients with schizophrenia showed poorer insight into their illness (p < 0.05)The degree of insight into their illness was related to the medication adherence level, a greater degree of therapeutic alliance, and lower severity of symptoms (p < 0.05)After 1 year of follow-up, significant direct associations were found between an improvement in the patient’s insight into their mental disorder or an improvement in the doctor-patient relationship, and an increase in medication adherence, improvement in global functioning and clinical outcome |
| A cross sectional analysis of pattern and predictors of medication adherence in bipolar disorder: a single centre experience from south India | Selvakumar N et al., 2018, India | Determine patterns and predictors of medication adherence in bipolar disorderDesign: observational cross-sectional study | n = 160Women, 79 (49.4%); men, 81 (50.6%)Age 36–45 years, 52 (32.5%) | Confirmation of diagnosis:Mini International Neuropsychiatric Interview (MINI)Adherence:Moriski Green Levine Adherence (MGLA) scaleAddictions:Drug Attitude Inventory (DAI) | Unclear risk of bias | Moderate | Low adherence level, 97 (60.6%)Factors that favour adherence:Formal jobRecent prolonged hospitalisationLow frequency of depressive episodesGood attitude towards treatment |
| Attitude towards drug therapy in a community mental health care assessed by drug attitude inventory | Di Lorenzo R et al., 2020, Italy | Assess attitude towards treatment with psychotropics in a representative sample of psychiatric patients using the 30-item Drug Attitude Inventory (DAI-30).Identify the sociodemographic and clinical factors related to the attitude towards treatmentDesign: observational cross-sectional study | n = 300Women, 164 (55%); men, 136 (45%)Age, 48.5 ± 14.39 years | Attitude towards treatment:Drug Attitude Inventory (DAI-30) | Unclear risk of bias | Moderate | Attitude towards medications:Moderately positive (moderate adherence)Factors that favour medication adherence:Being marriedBeing a studentBeing retired due to ageFactors that affect medication adherence:MonotherapyProlonged hospital admissions |
| Medication adherence using electronic monitoring in severe psychiatric illness: 4 and 24 weeks after discharge | Lee Y et al., 2019, South Korea | Examine medication adherence after hospitalisation of patients with severe mental disorders, such as bipolar disorder and schizophrenia, and to investigate factors associated with adherence.Design: observational cross-sectional study | n = 81Schizophrenia, 35 (43.2%)Bipolar disorder, 46 (56.8%)Age 36.07 ± 12 yearsMen, 30 (37%) | Sociodemographic characteristicsDrug Attitude Inventory (DAI) Korean VersionContour Drawing Rating Scale (CDRS)Multidimensional Scale of Perceived Social Support (MSPSS)Assessment of the severity of mental illness: Clinical Global Impression Severity (CGI-S) | Unclear risk of bias | Moderate | Medication adherence:Non-adherence, 26.4% at 4 weeks after discharge and 37.7% at 24 weeksFactors that determine adherence:Attitude towards treatmentPerception of body shape |
| Medication adherence in patients with schizophrenia: a qualitative study of the patient process in motivational interviewing | Dobber J et al., 2018, Netherlands | Assess the effect of motivational interviewing on medication adherence inpatients with schizophreniaDesign: qualitative, multiple cases, with motivational interviews | n = 14Men, 10 (71%)Age, 35.5 ± 23 years | Multiple case analysis: 3 phasesAnalysis of 1 single caseCross-case analysisCross-case synthesisMotivational interviewing | Unclear risk of bias | Moderate | Factors that improve adherence:Relationship of trust with the psychiatristTherapist's ability to adapt the motivational interview to the patient’s needsExplicit conversation about the patient’s values and their goals in relation to adherenceClear identification of patient ambivalence or barriers to adherence |
| Mediating Effect Of The Motivation For Medication Use On Disease Management And Medication Adherence Among Community-Dwelling Patients With Schizophrenia | Ling W et al., 2019, China | Assess the mediating effect of motivation for taking treatment and adherence in patients with schizophrenia.Design: cross-sectional descriptive and correlational | n = 373Men, 217 (58.2%); women, 156 (41.8%)Age, 46.6 ± 9.1 years | Control variables: patient informationGlobal Assessment of Functioning (GAF)Brief Psychiatric Rating Scale (BPRS)Working Alliance Inventory-Short (WAI-S) | Low risk of bias | Moderate | Therapeutic adherence, 47.2%Motivation had a 50% mediating effect on therapeutic alliance and medication adherence.Patients with social and medical support and high degree of insight had up to 72% adherence |
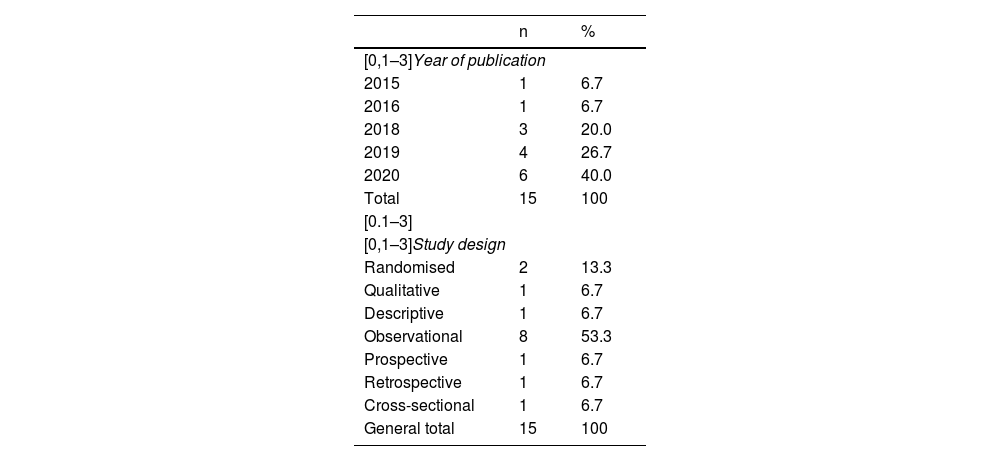
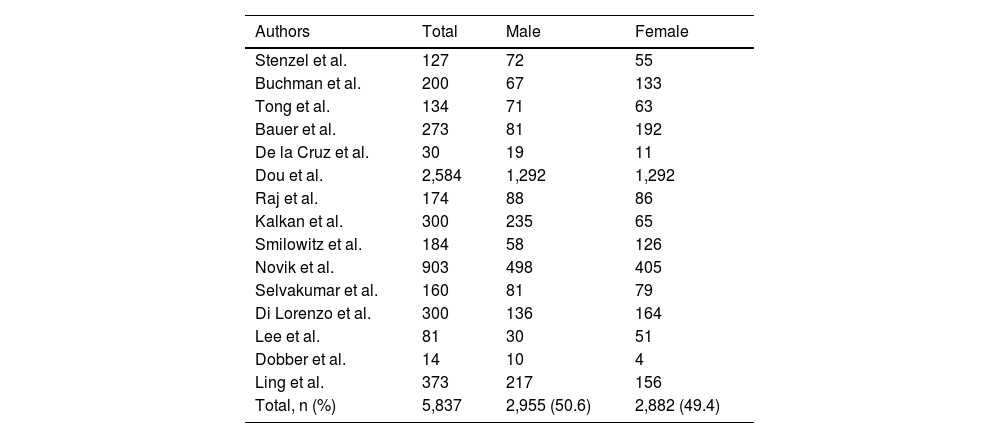
In terms of publication, 40% (n = 6) of the selected articles were from 2020; 20% (n = 3) were written in China and 53.3% (n = 8) were observational studies. A total population of 5,837 patients with serious psychiatric disorders was included, 49.4% women. (n = 2,882) and 50.6% men (n = 2,955) (Tables 2 and 3).
Year of publication and design of the assessed studies.
| n | % | |
|---|---|---|
| [0,1–3]Year of publication | ||
| 2015 | 1 | 6.7 |
| 2016 | 1 | 6.7 |
| 2018 | 3 | 20.0 |
| 2019 | 4 | 26.7 |
| 2020 | 6 | 40.0 |
| Total | 15 | 100 |
| [0.1–3] | ||
| [0,1–3]Study design | ||
| Randomised | 2 | 13.3 |
| Qualitative | 1 | 6.7 |
| Descriptive | 1 | 6.7 |
| Observational | 8 | 53.3 |
| Prospective | 1 | 6.7 |
| Retrospective | 1 | 6.7 |
| Cross-sectional | 1 | 6.7 |
| General total | 15 | 100 |
Study population.
| Authors | Total | Male | Female |
|---|---|---|---|
| Stenzel et al. | 127 | 72 | 55 |
| Buchman et al. | 200 | 67 | 133 |
| Tong et al. | 134 | 71 | 63 |
| Bauer et al. | 273 | 81 | 192 |
| De la Cruz et al. | 30 | 19 | 11 |
| Dou et al. | 2,584 | 1,292 | 1,292 |
| Raj et al. | 174 | 88 | 86 |
| Kalkan et al. | 300 | 235 | 65 |
| Smilowitz et al. | 184 | 58 | 126 |
| Novik et al. | 903 | 498 | 405 |
| Selvakumar et al. | 160 | 81 | 79 |
| Di Lorenzo et al. | 300 | 136 | 164 |
| Lee et al. | 81 | 30 | 51 |
| Dobber et al. | 14 | 10 | 4 |
| Ling et al. | 373 | 217 | 156 |
| Total, n (%) | 5,837 | 2,955 (50.6) | 2,882 (49.4) |
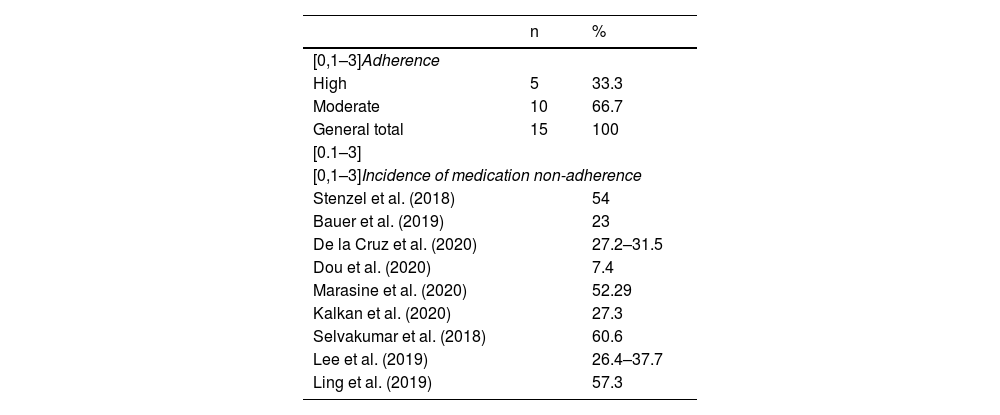
Reports on medication adherence were very heterogeneous. In most cases, the reports were qualitative: 10 investigations (66.7%)13–22 reported moderate adherence, and the rest (n = 5; 33.3%) had high adherence.3,23–26 The figures for non-adherence varied from 7.7% to 60.6% (Table 4).
Degree of adherence and incidence of medication non-adherence.
| n | % | |
|---|---|---|
| [0,1–3]Adherence | ||
| High | 5 | 33.3 |
| Moderate | 10 | 66.7 |
| General total | 15 | 100 |
| [0.1–3] | ||
| [0,1–3]Incidence of medication non-adherence | ||
| Stenzel et al. (2018) | 54 | |
| Bauer et al. (2019) | 23 | |
| De la Cruz et al. (2020) | 27.2–31.5 | |
| Dou et al. (2020) | 7.4 | |
| Marasine et al. (2020) | 52.29 | |
| Kalkan et al. (2020) | 27.3 | |
| Selvakumar et al. (2018) | 60.6 | |
| Lee et al. (2019) | 26.4–37.7 | |
| Ling et al. (2019) | 57.3 | |
Age was one of the factors most associated with low adherence to medication. Five studies reported that being an older adult was a factor related to worse adherence.3,13,15,19,26 Being female was also considered a factor that influences poor medication adherence.13,15,24
Other factors mentioned by the researchers consulted were the lack of full-time formal employment and vocational training, the low degree of social functioning, not having social support networks, and the taking of atypical antipsychotics.13
For Dou et al.27 the main factor associated with poor medication adherence is the stage of the illness (consolidation phase) (p < 0.05), while a high educational level favours adherence (p < 0.05). Marasine et al.24 establish that illiteracy, unemployment and the presence of serious adverse effects are the factors that most affect adherence to psychopharmacological treatment.
Buchman et al.28 mention that the feeling of loss related to the illness, grief, adverse effects and self-stigmatisation (p < 0.005) considerably reduce adherence.
According to Selvakumar et al.,18 the factors that favour adherence are formal employment and recent prolonged hospitalisation, a low rate of depressive episodes and a good attitude towards treatment.
Di Lorenzo et al.19 concluded that the factors that favour medication adherence are being married, being a student or being retired due to age, while monotherapy and prolonged hospitalisations reduce adherence. Lee et al.20 identified attitude toward treatment and perception of body shape as determining factors.
For Dobber et al.,21 the factors that improve adherence are the relationship of trust with the psychiatrist, the therapist's ability to adapt the motivational interview to the patient's needs, the explicit conversation about the patient’s values and goals, in relation to adherence, and clear identification of patient ambivalence or barriers to adherence.
Causes of non-adherenceThe most important cause of non-adherence identified in the research consulted is the lack of knowledge and acceptance of the illness (insight). The degree of insight into their illness was related to the level of medication adherence, with a greater degree of therapeutic alliance and less severity of symptoms (p < 0.05).17,22,25
Significant direct associations were found between an improvement in the patient’s insight into their mental disorder or an improvement in the doctor-patient relationship and an increase in medication adherence and improvement in global functioning and clinical outcome.17,22,25
Other causes of non-adherence described were the lack of social support and low empathy with the psychiatrist, which induces a low degree of motivation to adhere to treatment.22 Also, Chieng et al.23 mention that the significant increase in insight into the illness and treatment increases therapeutic adherence, reduces the severity of symptoms, increases functionality and reduces hospital readmissions.
Meanwhile, as the cause of non-adherence, De la Cruz et al.16 report forgetfulness (36.6%), adverse effects (26,6%), polymedication (20%), changes in routine (10%), and the perception that it is not necessary (6.7%).
DiscussionAccording to the literature consulted, medication adherence in patients with severe mental disorders is subject to several factors, including sociodemographic conditions (age and gender) related to the illness, medication and access to psychiatric services.3,13–26
Regarding the characteristics of the patients, there is consensus in the literature about a predominance of low adherence among women, who have been shown to be less adherent to treatment in several studies, although with no causal explanation established.14,29 However, there are authors who indicate that living as a couple and having a family and social support network increase adherence and positive attitudes towards treatment, and that women, in general, stay married longer than men. Therefore, it would be necessary to delve deeper into the role of gender in adherence to antipsychotic treatment.30,31
The role of the caregiver in adherence, as part of sociodemographic factors, was analysed by Guerrero32 in a series of 43 cases of schizophrenia in Ecuador. This study demonstrated that the main factor in poor adherence among these patients was the lack of knowledge of the family member or caregiver about the basic aspects of the illness and the importance of ensuring compliance with medical instructions. This author mentions that most people in charge of caring for patients with schizophrenia have not been trained to look after them, do not know the symptoms of the disease or how it evolves, nor do they have general notions about the effects of antipsychotic medications or the effect on the individual of not taking them regularly.
Differences in medication adherence are also described depending on the diagnosis. Patients with schizophrenia and depressive disorders are those with the lowest degree of adherence in the studies consulted. These results can be held up by those of Kalkan et al.,25 who established that adherence to pharmacological treatment by patients with schizophrenia is directly related to the degree to which patients can make their own decisions, accept their illness, and participate actively in their treatment (insight). For these authors, medication adherence in their patients with schizophrenia was moderate, and the main cause of non-adherence was intolerance to the side effects of the medications and the perception that the medications were useless. They also mention that patients’ low educational level and lack of employment are directly related to the non-adherence and abandonment of treatment by these patients.
In the case of patients with bipolar disorder, although they show more adherence than patients with depression and schizophrenia, this depends on crisis-free time or the degree of social support. Authors like Levin et al.,33 who included 160 patients with bipolar disorder, report non-adherence in 75% of patients. In that study, the factors related to adherence were: favourable or positive attitudes towards the treatment (which increase adherence), negative attitudes towards it (which reduce adherence); and involuntary non-adherence related to the family support network and economic factors. The authors therefore propose that, among the interventions to improve treatment adherence by these patients, efforts should be made to reinforce positive attitudes to the treatment.
Chapman et al.34 established that physical and perceptual barriers determine medication non-adherence in patients with severe depression, with a significant predominance of the perceptual barriers, in which beliefs about treatment and its importance play a primary role. This is why the non-adherence of patients with depression is usually unintentional and due to forgetfulness. They point out that motivational factors can have a significant impact on the practical and perceptual barriers to medication adherence for these patients. These authors therefore propose focusing actions for ensuring adherence on strengthening motivation.
Ifteni et al.35 also addressed the importance of access to psychiatric services in medication adherence, mentioning that in the current epidemiological context, adherence of patients with serious mental disorders is affected by restrictions on access to medication and follow-up consultations. Therefore, they propose prescribing long-acting antipsychotics by injection as an effective way of ensuring continuity of treatment, especially in young patients with schizophrenia (under 35 years of age), in whom they are most effective. For these authors, long-acting antipsychotics by injection more frequently determined remission and recovery than oral antipsychotics, by avoiding treatment dropout. Their efficacy in preventing relapses, even in catatonic forms, has been demonstrated, and their great utility in reducing hospital visits; an important factor in the midst of this current health emergency.
Study limitationsAs the studies we consulted used heterogeneous instruments, methods and populations to measure medication adherence, this could be considered a limitation of our research which merits further investigation into the topic.
ConclusionsAdherence of patients with serious mental illness to treatment with psychotropic drugs is multifactorial. It depends on patient-specific factors, such as their age, gender, marital status, and social and family support network, and factors related to the illness or treatment. The most important cause of non-adherence identified in the research consulted is the lack of insight into their illness. Non-adherence figures vary from 7.7% to 60.6%.
Medication adherence in patients with schizophrenia was moderate, and the main cause of non-adherence is intolerance to the side effects of the drugs. Patients with bipolar disorder show greater adherence than patients with depression and schizophrenia. Non-adherence in patients with depression is usually unintentional and due to forgetfulness. It has therefore been suggested that motivational factors may have a significant impact.
In any event, it has been shown that interventions aimed at improving access to psychiatric services, levels of knowledge about the illness, education of the family and the patients themselves, and the interaction with the mental health worker can promote positive attitudes towards treatment and adherence.
FundingThis research was self-funded and did not receive contributions from any institution.
Conflicts of interestThe authors have no conflicts of interest to declare.