Little is known regarding the relevance of racial/ethnic background to the risk for COVID-19 infection, particularly in Europe. We evaluated the risk of COVID-19 among migrants from different areas of the world within the context of universal free access to medical care.
Materials and methodsWe conducted a population-based cohort analysis of the cumulative incidence of PCR-confirmed COVID-19 among adult residents of Alcorcon (Spain) in the first wave of the disease up to April 25, 2020.
ResultsThe crude cumulative incidence among migrants (n = 20419) was higher than among Spaniards (n = 131599): 8.81 and 6.51 and per 1000 inhabitants, respectively (p < .001), but differed by region of origin. As per a negative binomial regression adjusted for age and sex, relative risk (RR) for COVID-19 for individuals from Europe, Asia, or North Africa was not significantly different from Spaniards. In contrast, a markedly increased risk was found in people from Sub-Saharan Africa (RR 3.66, 95% confidence interval (CI) 1.42−9.41, p = .007), the Caribbean (RR 6.35, 95% CI 3.83−10.55, p < .001), and Latin America (RR 6.92, 95% CI 4.49−10.67, p < .001).
ConclusionsMigrants from Sub-Saharan Africa, the Caribbean, and Latin America exhibited increased risk for COVID-19 as compared to Spaniards or migrants from Europe, North Africa, or Asia. Our data suggest ethnic background may play a role in risk for COVID-19. Migrants from some areas of the world may merit closer attention for both clinical and epidemiological reasons.
Existen pocos estudios sobre el potencial papel de los orígenes raciales / étnicos en el riesgo de infección de COVID-19, particularmente en Europa. Evaluamos el riesgo de COVID-19 entre los migrantes de diferentes zonas del mundo en un contexto de acceso universal gratuito a la atención médica.
Material y métodosRealizamos un análisis de cohortes poblacional de la incidencia acumulada de COVID-19 confirmado mediante PCR entre los residentes adultos en Alcorcón (España) en la primera oleada de la enfermedad hasta el 25 de abril de 2020.
ResultadosLa incidencia acumulada bruta entre los migrantes (n = 20419) fue mayor que entre los españoles (n = 131599): 8,81 y 6,51 y por cada 1000 habitantes respectivamente (p < 0,001), pero difería según la región de origen mundial. Mediante regresión binomial negativa, ajustada por edad y sexo, los riesgos relativos (RR) para COVID-19 no fueron significativamente diferentes de los españoles para los individuos provenientes de Europa, Asia o el norte de África. Por el contrario, hubo un marcado aumento del riesgo para los del África subsahariana (RR 3,66, intervalo de confianza del 95% [IC] 1,42-9,41, p = 0,007), el Caribe (RR 6,35, 95% IC 3,83-10,55, p < 0,001) y América Latina (RR 6,92, 95% IC 4,49-10,67, p < 0,001).
ConclusionesLos migrantes procedentes del África subsahariana, el Caribe y América Latina, a diferencia de los españoles o migrantes procedentes de Europa, el norte de África o Asia, presentaron un mayor riesgo de COVID-19. Nuestros datos sugieren un papel para el origen étnico en el riesgo de COVID-19. Los migrantes de algunas zonas del mundo pueden merecer una atención más cercana tanto por razones clínicas como epidemiológicas.
The COVID-19 pandemic represents a tremendous challenge to mankind, with dramatic health and economic consequences.1–3 Recent reports have highlighted increased COVID-19-related mortality among migrants and ethnic minorities in Western countries.4–10 However, the clinical outcomes—mortality in particular—associated with ethnic minorities are inextricably connected to different socioeconomic backgrounds, pre-existing medical conditions, and unequal access to medical services.11–14
There have been a number of media reports and calls to action in this regard, but very few sound scientific publications addressing this issue. In addition, most of the studies that do exist come from the United States of America or the United Kingdom and virtually none from European countries.15–18
In this work, we sought to describe the incidence of COVID-19 in the first wave of the disease among Spaniards and migrants from different areas of the world living in Alcorcón, a city in the suburbs of Madrid (Spain) with a substantial proportion of foreign residents. The different proportions of migrants from many areas of the world to Spain may provide an opportunity for evaluating COVID-19 risk in these populations.
MethodsThis population-based cohort study was conducted in Alcorcón (Madrid), which has a total population of about 170,000 inhabitants. The at-risk population was defined as all adults registered in the official municipal population registry of the City Council of Alcorcón (last updated March 14, 2020).19 The distribution of the population by nationality and country of origin and stratified by age and sex was obtained from this registry.
A case was defined as a patient with a COVID-19 diagnosis made at the Hospital Universitario Fundación Alcorcón confirmed by reverse transcription polymerase chain reaction (RT-PCR) for SARS-CoV-2 for adults residing in Alcorcón. Incident cases of COVID-19 were obtained from the electronic medical record (Selene ©). A clinical diagnosis of COVID-19 was established by the attending clinicians in the emergency department according to the European Centre for Disease Control and Prevention (ECDCP)-World Health Organization (WHO) criteria.20
For molecular diagnosis of SARS-CoV-2 infection, nasopharyngeal swabs from symptomatic patients were processed by automatized extraction using the MagNa Pure LC instrument (Roche Applied Science, Mannheim, Germany) and real-time RT-PCR (rRT-PCR) using the VAISURE SARS-CoV-2 nucleic acid detection kit (CerTest Biotec S.L.), following the manufacturer’s instructions. For this rRT-PCR, we used Bio-Rad CFX96™ Real-Time PCR Detection System. We amplified two different viral regions: the ORF1ab gene (FAM channel), N gene (ROX channel), and the internal control (HEX channel). Cycle threshold values ≤ 40 were considered positive. Positive and negative controls were included in each run for every assay.
An anonymized set of data was extracted from patients’ electronic medical records (from February 1 st to April 25th) and included the following parameters: age, sex, nationality, country of birth, city of residence, date of COVID-19 diagnosis (clinical), date and results of SARS-CoV-2 PCR, and clinical progress/outcomes (hospital admission, critical care admission, hospital discharge, length of hospital stay, and in-hospital death). For this study, patients whose residence was outside the city of Alcorcón were excluded.
Patients were classified according to their country of origin into one of the following groups: (a) Spain, (b) the European Union (including Switzerland and Norway), (c) Eastern Europe (including Russia), (d) Asia, (e) Australia and New Zealand, (f) North Africa, (g) Sub-Saharan Africa, (h) Latin America (Mexico and continental Latin American countries), (i) the Caribbean, and (j) the United States of America and Canada.
StatisticsResults are shown as means (± standard deviation), medians (interquartile range), or percentages, as appropriate. Quantitative variables were compared using the Student’s t-test, ANOVA, or Mann-Whitney U test, as appropriate. Qualitative variables were compared using the chi-square test or Fisher’s exact test, as appropriate.
Aggregated data were analyzed according to world area (or country) of origin, sex, and age group (< 30, 30–39, 40–49, 50–59, 60–69, 70–79, 80–89, and ≥ 90 years). Incidence rates and 95% exact Poisson confidence intervals were calculated by the world area of origin. A multivariate negative binomial regression model with robust variance was used to estimate the incidence rate by world area adjusted for sex and age. These models are appropriated to analyze overdispersed count data.21,22 Statistical significance was assumed for p values < .05. All statistical analyses were conducted with Stata 14 (StataCorp LLC, Texas, USA). The protocol was approved by the local independent review board/drug research ethics committee.
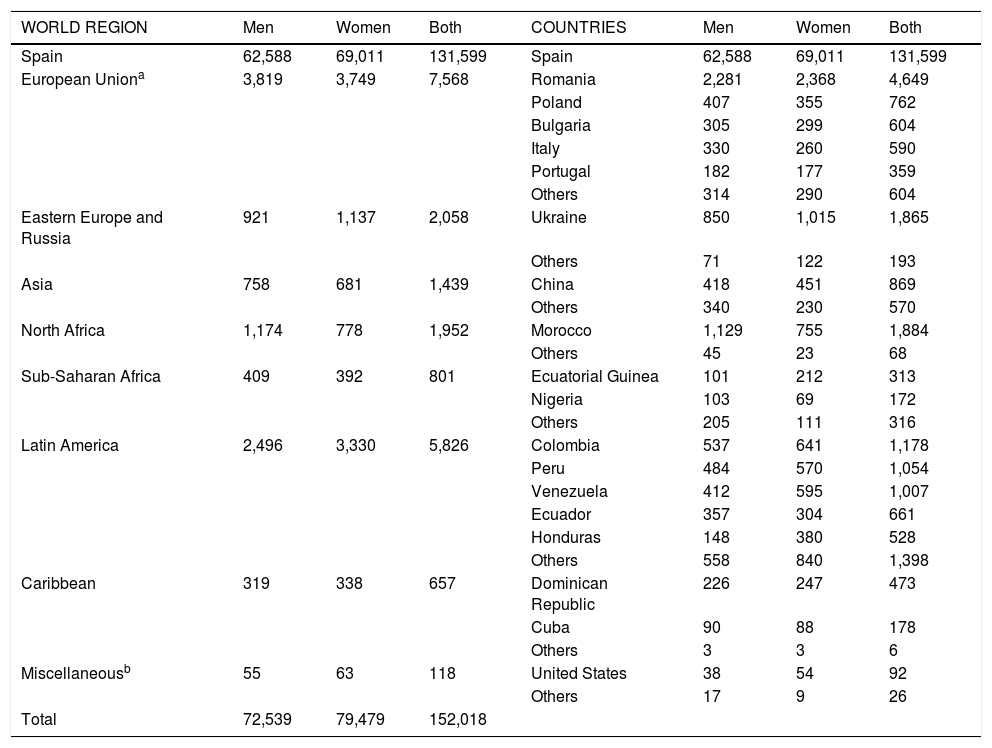
ResultsThe Alcorcón municipal registry included 152,018 individuals 17 years of age or older as of March 14, 2020.19 Of them, 20,419 (13.4%) residents had a nationality other than Spanish. The countries of origin (and associated areas of the world) are summarized in Table 1.
Distribution of migrants residing in Alcorcón (Spain) as of March 14, 2020 by world region, country, and sex.
| WORLD REGION | Men | Women | Both | COUNTRIES | Men | Women | Both |
|---|---|---|---|---|---|---|---|
| Spain | 62,588 | 69,011 | 131,599 | Spain | 62,588 | 69,011 | 131,599 |
| European Uniona | 3,819 | 3,749 | 7,568 | Romania | 2,281 | 2,368 | 4,649 |
| Poland | 407 | 355 | 762 | ||||
| Bulgaria | 305 | 299 | 604 | ||||
| Italy | 330 | 260 | 590 | ||||
| Portugal | 182 | 177 | 359 | ||||
| Others | 314 | 290 | 604 | ||||
| Eastern Europe and Russia | 921 | 1,137 | 2,058 | Ukraine | 850 | 1,015 | 1,865 |
| Others | 71 | 122 | 193 | ||||
| Asia | 758 | 681 | 1,439 | China | 418 | 451 | 869 |
| Others | 340 | 230 | 570 | ||||
| North Africa | 1,174 | 778 | 1,952 | Morocco | 1,129 | 755 | 1,884 |
| Others | 45 | 23 | 68 | ||||
| Sub-Saharan Africa | 409 | 392 | 801 | Ecuatorial Guinea | 101 | 212 | 313 |
| Nigeria | 103 | 69 | 172 | ||||
| Others | 205 | 111 | 316 | ||||
| Latin America | 2,496 | 3,330 | 5,826 | Colombia | 537 | 641 | 1,178 |
| Peru | 484 | 570 | 1,054 | ||||
| Venezuela | 412 | 595 | 1,007 | ||||
| Ecuador | 357 | 304 | 661 | ||||
| Honduras | 148 | 380 | 528 | ||||
| Others | 558 | 840 | 1,398 | ||||
| Caribbean | 319 | 338 | 657 | Dominican Republic | 226 | 247 | 473 |
| Cuba | 90 | 88 | 178 | ||||
| Others | 3 | 3 | 6 | ||||
| Miscellaneousb | 55 | 63 | 118 | United States | 38 | 54 | 92 |
| Others | 17 | 9 | 26 | ||||
| Total | 72,539 | 79,479 | 152,018 |
Different areas of the world were chosen according to geographical, socioeconomic, and ethnic background reasons, provided there was a minimum of 500 individuals per area. There were less than 200 migrants from the USA, Canada, Australia, and New Zealand and therefore they were removed further analysis.
Migrant residents were substantially younger than Spaniards (median age 40 years (IQR 30–50) vs. 49.5 years (IQR 38–67), respectively (Appendix B; Supplementary Fig. 1), and there was a slightly higher proportion of males (48.7 vs. 47.6% p = .002). Indeed, the age distribution pyramids in the reference population for Spaniards and migrants were remarkably different (Appendix B; Supplementary Fig. 2).
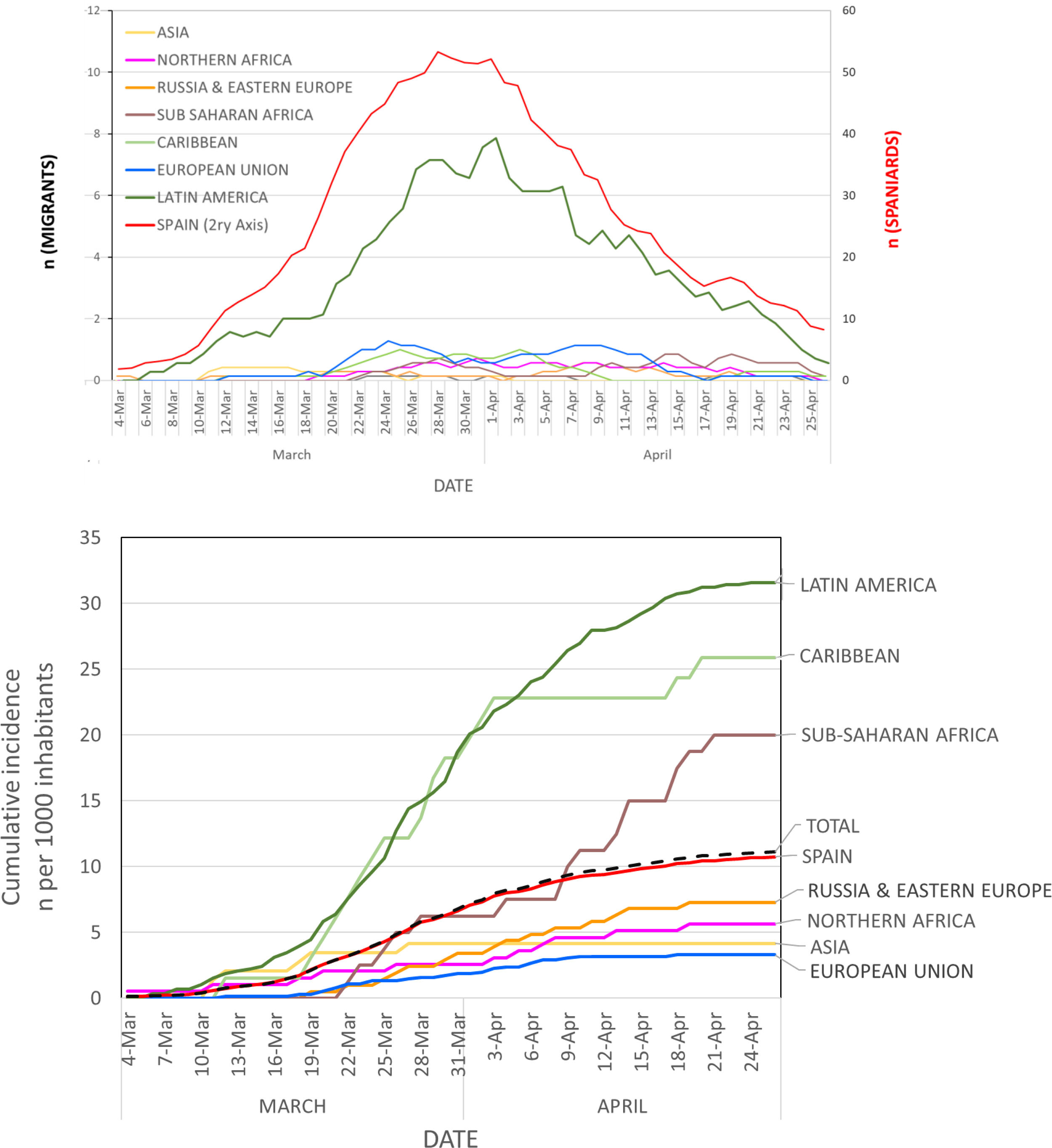
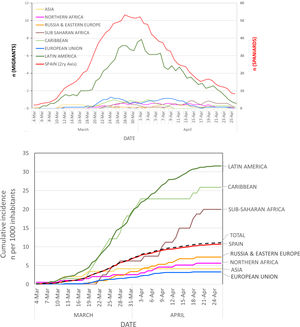
A total of 1691 residents in Alcorcón were diagnosed with COVID-19 according to ECDCP-WHO clinical criteria20 at our hospital from February 1 to April 25, 2020 (Fig. 1A). The number of cases increased steadily until the end of March and declined thereafter (Fig. 1B), roughly two weeks after the lockout Decree of the Spanish Government.23 In order to avoid potential misdiagnoses, we restricted our analysis to the 1036 cases with a positive SARS-CoV-2 PCR (COVID-19-PCR + cases). The median age of COVID-19-PCR + patients was 71 years (IQ range 54−79) and 57.2% were male.
Evolution of clinical diagnosis of COVID-19.
Panel A: daily diagnoses (graph represents the 7-day moving average on each date = number of daily diagnoses in the preceding week) at the Hospital Universitario Fundación Alcorcón.
Panel B: Cumulative incidence rate of new COVID-19 clinical diagnoses according to region of the world at the Hospital Universitario Fundación Alcorcón.
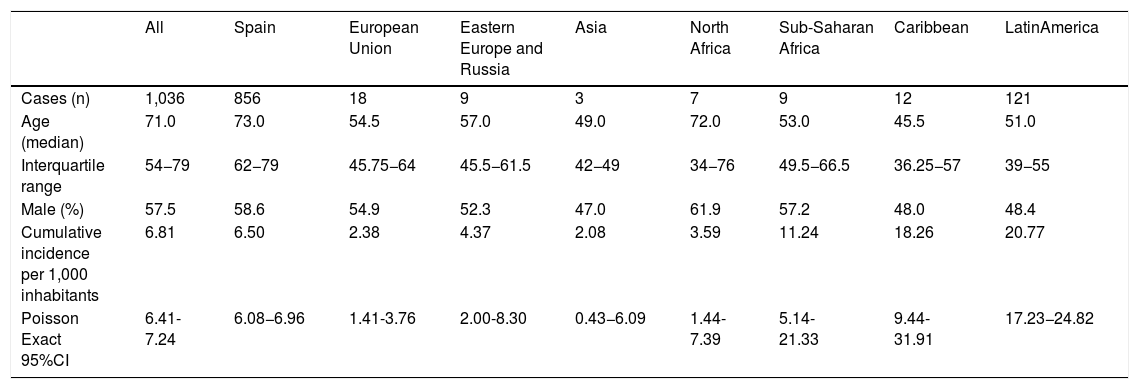
The overall cumulative COVID-19-PCR + incidence was 6.81 per 1000 inhabitants. The overall cumulative COVID-19-PCR + incidence in Spaniards was 6.50 cases per 1000 inhabitants as compared to 8.82 per 1000 for non-Spaniards (p < .001; Table 2, Fig. 1B).
COVID-19 PCR + patients in Alcorcón (Spain). Cumulative incidence by world region of origin (February-April 2020).
| All | Spain | European Union | Eastern Europe and Russia | Asia | North Africa | Sub-Saharan Africa | Caribbean | LatinAmerica | |
|---|---|---|---|---|---|---|---|---|---|
| Cases (n) | 1,036 | 856 | 18 | 9 | 3 | 7 | 9 | 12 | 121 |
| Age (median) | 71.0 | 73.0 | 54.5 | 57.0 | 49.0 | 72.0 | 53.0 | 45.5 | 51.0 |
| Interquartile range | 54−79 | 62−79 | 45.75−64 | 45.5−61.5 | 42−49 | 34−76 | 49.5−66.5 | 36.25−57 | 39−55 |
| Male (%) | 57.5 | 58.6 | 54.9 | 52.3 | 47.0 | 61.9 | 57.2 | 48.0 | 48.4 |
| Cumulative incidence per 1,000 inhabitants | 6.81 | 6.50 | 2.38 | 4.37 | 2.08 | 3.59 | 11.24 | 18.26 | 20.77 |
| Poisson Exact 95%CI | 6.41-7.24 | 6.08−6.96 | 1.41-3.76 | 2.00-8.30 | 0.43−6.09 | 1.44-7.39 | 5.14-21.33 | 9.44-31.91 | 17.23−24.82 |
COVID-19-PCR + cases who were Spaniards were substantially older than migrants (median age 73 years (IQR 62–80) vs 51.5 (IQR 41.7–58) p < .001) and there was a higher proportion of males, though this finding was not statistically significant (58.6% vs. 52.5%; p = .15) (Appendix B; Supplementary Fig. 3). The overall cumulative incidence increased dramatically with age in both Spaniards and migrants (Appendix B; Supplementary Fig. 3A).
Next, we evaluated the cumulative incidence of COVID-19-PCR + for natives from different regions of the world as compared to Spaniards (Table 2, Fig. 1B). Unadjusted incident rates for individuals from Europe, Asia, and North Africa were lower than average whereas rates for individuals from Sub-Saharan Africa, the Caribbean, and Latin America were higher than average. Cumulative incident rates for most representative countries are shown in Appendix B; Supplementary Fig. 1.
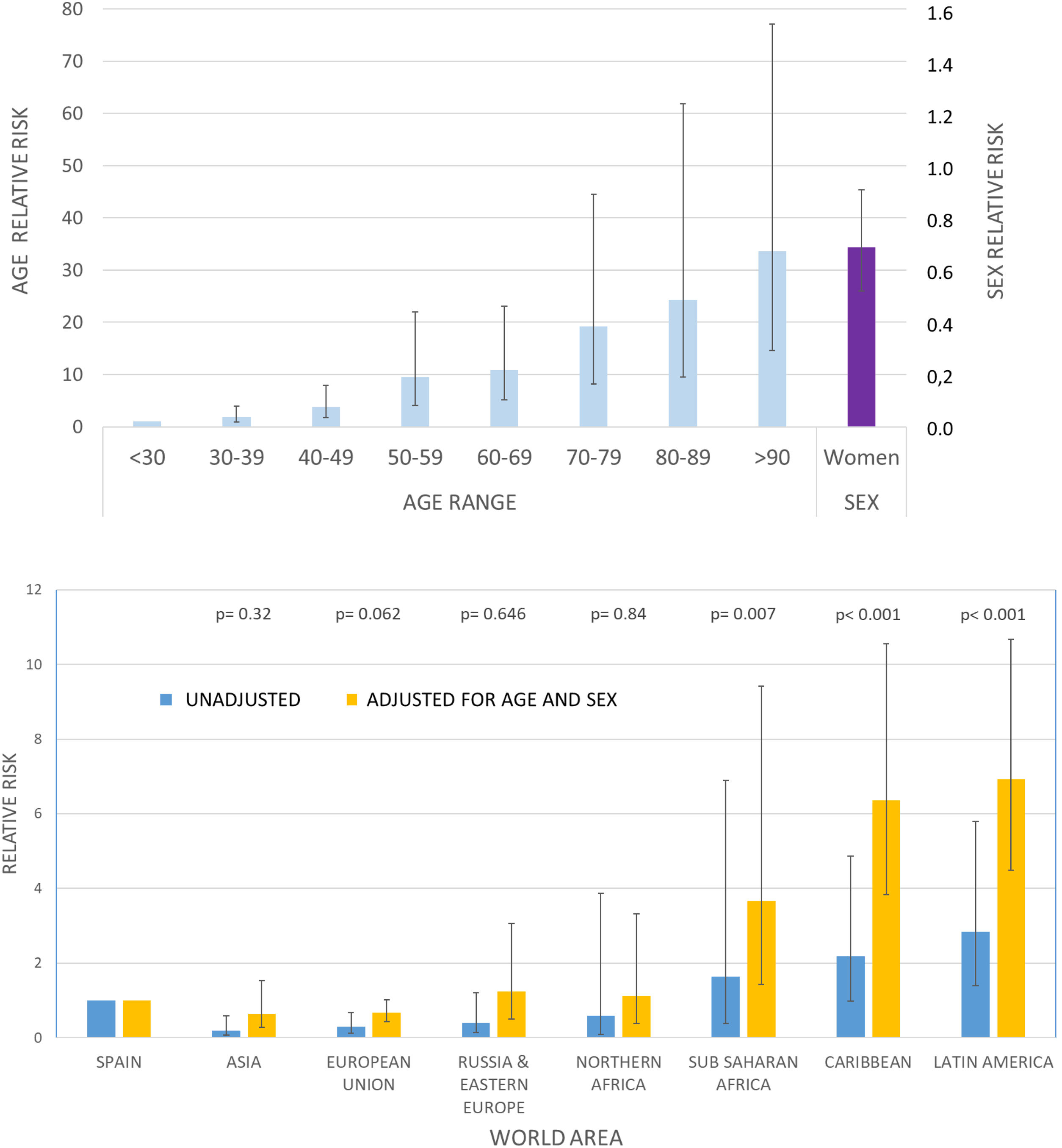
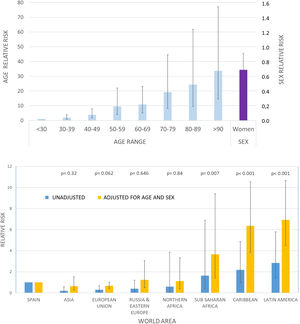
In order to better understand the risks for Spaniards and migrants from different regions of the world, we conducted a multivariate negative binomial regression analysis21,22 that was adjusted for age and sex, as these factors are proven determinants of COVID-19 risk (Fig. 2). The adjusted relative risks for COVID-19-PCR + among migrants from Asia, the European Union, and Eastern Europe did not significantly differ from Spaniards (Table 3, Fig. 2).
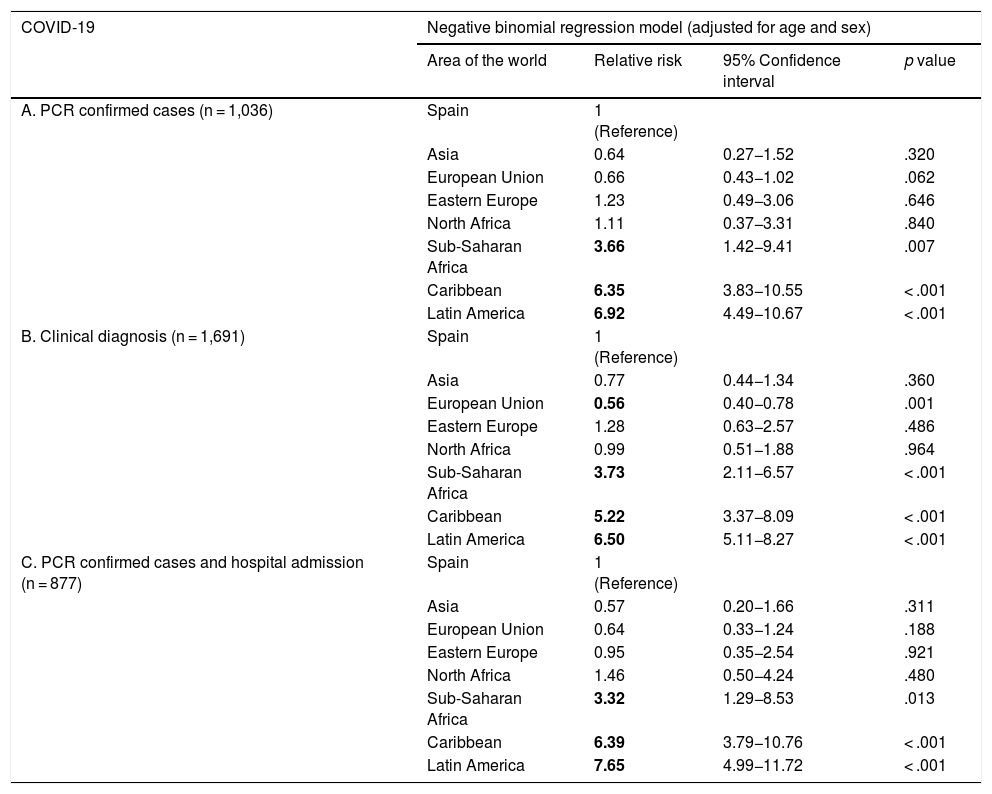
Negative binomial regression models for COVID-19 incidence by world region of origin (A) and sensitivity analysis (B and C). Alcorcón (Spain), February-April 2020.
| COVID-19 | Negative binomial regression model (adjusted for age and sex) | |||
|---|---|---|---|---|
| Area of the world | Relative risk | 95% Confidence interval | p value | |
| A. PCR confirmed cases (n = 1,036) | Spain | 1 (Reference) | ||
| Asia | 0.64 | 0.27−1.52 | .320 | |
| European Union | 0.66 | 0.43−1.02 | .062 | |
| Eastern Europe | 1.23 | 0.49−3.06 | .646 | |
| North Africa | 1.11 | 0.37−3.31 | .840 | |
| Sub-Saharan Africa | 3.66 | 1.42−9.41 | .007 | |
| Caribbean | 6.35 | 3.83−10.55 | < .001 | |
| Latin America | 6.92 | 4.49−10.67 | < .001 | |
| B. Clinical diagnosis (n = 1,691) | Spain | 1 (Reference) | ||
| Asia | 0.77 | 0.44−1.34 | .360 | |
| European Union | 0.56 | 0.40−0.78 | .001 | |
| Eastern Europe | 1.28 | 0.63−2.57 | .486 | |
| North Africa | 0.99 | 0.51−1.88 | .964 | |
| Sub-Saharan Africa | 3.73 | 2.11−6.57 | < .001 | |
| Caribbean | 5.22 | 3.37−8.09 | < .001 | |
| Latin America | 6.50 | 5.11−8.27 | < .001 | |
| C. PCR confirmed cases and hospital admission (n = 877) | Spain | 1 (Reference) | ||
| Asia | 0.57 | 0.20−1.66 | .311 | |
| European Union | 0.64 | 0.33−1.24 | .188 | |
| Eastern Europe | 0.95 | 0.35−2.54 | .921 | |
| North Africa | 1.46 | 0.50−4.24 | .480 | |
| Sub-Saharan Africa | 3.32 | 1.29−8.53 | .013 | |
| Caribbean | 6.39 | 3.79−10.76 | < .001 | |
| Latin America | 7.65 | 4.99−11.72 | < .001 | |
Relative risks in bold indicate statistical significance (p < .05).
In contrast, the relative risk for migrants from Latin America was about 7 times higher than that for Spaniards (RR 6.92; 95% CI 4.49−10.67; p < .001). In addition, the adjusted risk was also higher in migrants from Sub-Saharan Africa (RR 3.66; 95% 1.42−9.41; p = .007) as well as the Caribbean (RR 6.35; 95% CI 3.83−10.55; p < .001) in a manner that was highly clinically and statistically significant.
As a sensitivity analysis (Table 3), we repeated our estimation with more broadly-defined criteria (clinical diagnosis regardless of PCR results; n = 1,691) and stricter criteria (patients requiring hospital admission because of moderate-to-severe COVID-19, n = 877). In both cases, the results remained essentially unchanged.
Adjusted risks for migrants from Sub-Saharan Africa, the Caribbean, and Latin America were about 3, 6, and 7 times higher in all clinical scenarios (Table 3). As an exploratory assessment, we performed a similar analysis for countries that had at least 800 inhabitants in Alcorcón (Table 1). Citizens from Romania, Ukraine, China, and Morocco did not exhibit increased rates of COVID-19 cumulative incidence (Appendix B; Supplementary Fig. 4). In accordance with regional data, migrants from all Latin American countries showed a consistent increased risk for COVID-19.
Severe COVID-19, which was defined as death, intensive care unit admission, or a hospital stay longer than 7 days, occurred in 63% of Spaniards as compared to 33% of migrants. Similarly, unadjusted mortality was higher for Spaniards (25% of admissions) than for migrants (6%). This finding most likely mirrors the advanced age of patients who had severe disease (median age 76 years (IQR 69–82)) or those who died (median 79 years (IQR 74–85)), given that this age range virtually absent in migrants (Appendix B; Supplementary Figs. 1 and 2).
Our data do not support the notion that migrants residing in Spain have more severe disease.
DiscussionWith a population-based approach, our data reveal that incidence of COVID-19 varies among migrants from different areas of the world as compared to the Spanish reference population. A major finding of our work is an apparent higher risk for COVID-19 among individuals from Sub-Saharan Africa, the Caribbean or Latin America as compared to migrants from Europe, Asia, or North Africa or to Spaniards. Preliminary data on other areas in Madrid are consistent with our findings.10 A higher risk is consistently detected when it is estimated globally for the regions of origin or for particular countries and the risk is clearly enhanced when adjustments for age and gender are made.
We also found a lower unadjusted relative risk for COVID-19 for other European Union citizens as compared to Spaniards. However, migrants represent a younger population when compared to Spaniards,24,25 as is the case in our setting. Indeed, when adjusted for age and gender, the relative risk for COVID-19 for migrants from Europe (both the European Union and Eastern Europe) did not differ from Spaniards. Similarly, the adjusted incidence rate of COVID-19 in migrants from Asia or North Africa did not differ from the reference population.
The reasons underlying this apparent increased risk for COVID-19 among migrants from different areas of the world are not clear. First, all migrants have equal access to the virtually universal health coverage available to Spaniards. Second, most migrants have low-wage jobs and are of a lower socioeconomic status,26,27 which is also true for ‘European’ migrants, since this population mainly includes individuals from Romania and Ukraine in our city. An increased prevalence of hypertension or obesity may underlie a higher risk for migrants from Sub-Saharan Africa or Latin America, similar to what has been described in Blacks or Hispanics in the USA.28 However, in our setting, migrants from these areas do not seem to have a higher prevalence of obesity, hypertension, diabetes, or cardiovascular diseases. This may be related to their younger age and the so-called ‘healthy migrant effect.’24,25,29,30
Our study has several strengths, the first of which is its population-based approach. We used the best available updated registry of people living in the reference area. It is also likely that most migrants are included in this registry, since a number of social services rely upon current place of residence.19
Second, our approach to estimating incidence of COVID-19 in the entire population is reasonable given that the population primarily attended to in our hospital is precisely the city of Alcorcón and there is no other public hospital in the city.31 In a public health emergency like COVID-19, it is likely that residents would rely even more on their local facilities.
In any event, it is almost certain that a small number of Alcorcón residents would have sought care due to COVID-19 in hospitals different from ours and thus our data are likely an underestimation of the real incidence. The 16% of COVID-19 cases attended to in our hospital which were individuals whose residence was not Alcorcón were excluded from our analysis.
Official data from the Community of Madrid indicate that our hospital usually receives a slightly higher number of patients from other areas than vice-versa.(31) Accordingly, our underestimation of COVID-19 incidence in Alcorcón may be somewhere between 10% – 15%. We do not believe that these data would substantially modify the relative incidence for migrants, given that the proportion of COVID-19 cases in migrants which were excluded from our study because their residence was outside Alcorcon was essentially identical to that of Spaniards (17% vs. 16%, respectively).
Another critical issue is in relation to migrants’ access to medical care. Since July 2018, all individuals who reside in Spain have had access to free medical care in conditions virtually identical to Spaniards.32 It can be argued that some migrants may rely less on primary care physicians, thus leading to a disproportionate use of hospital services.25,33 However, our sensitivity analysis, which was restricted to more severe COVID-19 cases that requiring hospital admission, does not support this theoretical overuse of hospital resources.
Some limitations of our study must be addressed. First, we did not have local data regarding migrants’ socioeconomic status, education, or other health conditions. However, on aggregate, migrants from Romania, Ukraine, and Morocco who reside in Spain belong to a relatively lower socioeconomic class throughout Spain,27 as do migrants from Sub-Saharan Africa or Latin America. However, the former have not been found to be at increased risk for COVID-19 whereas the latter have, suggesting that socioeconomic status may not be a major reason for differences in COVID-19 incidence.
Given that the above-mentioned factors do not seem to adequately explain this increased incidence, attention should be paid to the ethnic background of the populations. Interestingly, a recent report from a large database from the United States Department of Veterans Affairs suggests that Black and Hispanic individuals in the USA are experiencing an excess burden of COVID-19 that is not entirely explained by underlying medical conditions,28 which is in accordance with our results.
Recent reports from the USA suggest that the increased risk found in Blacks is not found in Asians, which is also in agreement with our data.34 These data point to possible differences arising as a result of ethnic background, in addition to other socioeconomic reasons, as a potential risk factor for COVID-19.
There are limited data regarding different susceptibility to respiratory viruses in people from different ethnic backgrounds. Some studies have suggested that racial minorities have greater susceptibility to influenza.35 However, many studies have failed to dissociate clinical outcomes from socioeconomic issues, particularly unequal access to health care. Indeed, different susceptibilities to COVID-19 based on genetic background that have an unequal distribution are just beginning to be explored.36–38
Finally, our data do not suggest an increased mortality risk for migrants. Of note is the finding that Black and Hispanic individuals did not exhibit increased mortality in United States Department of Veterans Affairs database,28 which in contrast to other reports from the USA.6 These data suggest that access to healthcare rather than ethnicity may be the major determinant of survival in COVID-19.
ConclusionsIn conclusion, we report a selective increased risk for COVID-19 among certain migrant populations in Spain including those from Sub-Saharan Africa, the Caribbean, and Latin America that is not related to unequal access to health care. These groups may merit particular attention, especially when our country and others are experiencing an increase in COVID-19 incidence following the de-escalation of previous extreme social distancing measures.
Furthermore, our data may suggest different genetic susceptibility to COVID-19 among individuals from different ethnic backgrounds, a finding that warrants further study. Regardless of the reasons underlying the differential risk for COVID-19 in different migrant populations, our data serve to help identify individuals or groups at particularly high risk who may warrant special attention for both clinical and epidemiological reasons.
FundingSupported in part by Instituto de Salud Carlos III, grant COV20/00644.
Conflict of interestsThe authors declare no conflicts of interest.
This research has been approved by the Independent Review Board/Ethics Committee of the Hospital Universitario Fundación Alcorcón (Spain).
Appendix A. Alcorcón COVID Investigators: (Collaborators)Alejandro Algora, Juan Carlos Alonso-Punter, Gregorio Bonilla Zafra, Mercedes Bueno-Campaña, Virgilio Castilla, Ana Isabel Díaz-Cuasante, Aurora Fabero, Rosa María Fariña, Isabel M. Galán, Isabel González-Anglada, M. Mercedes Izquierdo, Susana Lorenzo, Juan Emilio Losa, Margarita Mosquera, Carmen Noguera, Montserrat Pérez-Encinas, Gil Rodríguez-Caravaca, José Francisco Valverde.
The authors thank Dr Fernando Rodríguez Artalejo for critically reviewing the manuscript.
Please cite this article as: Guijarro C, Pérez-Fernández E, González-Piñeiro B, Meléndez V, Goyanes MJ, Renilla ME et al. Riesgo de COVID-19 en españoles y migrantes de distintas zonas del mundo residentes en España en la primera oleada de la enfermedad. Rev Clin Esp. 2021;221:264–273.