To develop conceptual and operational definitions to define characteristics and related factors (individualised nursing care plan) for the process of 50-year-old patient with Wernicke–Korsakoff-encephalopathy.
MethodIntegrative literature review about Wernicke–Korsakoff-encephalopathy, after nursing assessment, based on the General Theory of Self-Care Deficit of Dorothea Orem, on admission to the Neurology ward of a third level Spanish hospital.
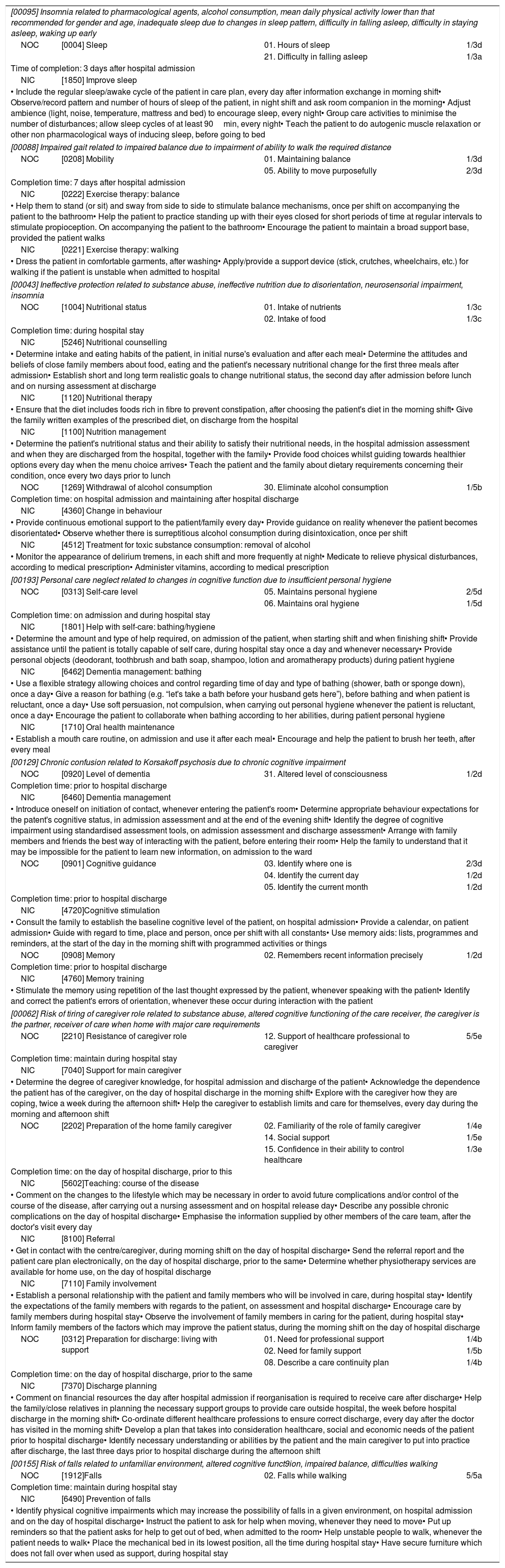
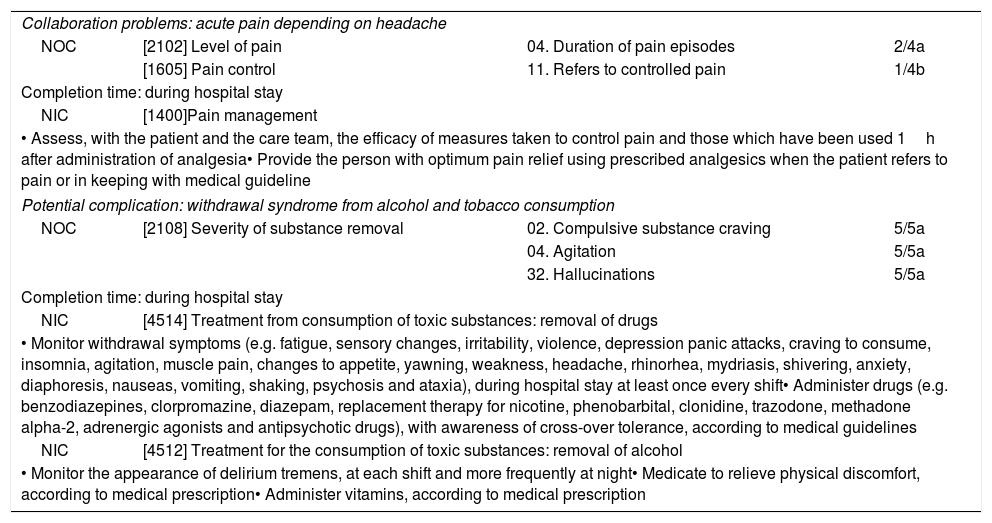
ResultsAn individualised care plan is proposed through the NANDA-NOC-NIC taxonomies following the nursing process. The attention to the main caregiver is highlighted in the plan, due to his great responsibility in the continuity of care on discharge, including new activities for it.
ConclusionsIt is necessary to use standard taxonomies for the development of the scientific nursing discipline, along with a holistic approach for the individualisation of care.
Desarrollar definiciones conceptuales y operacionales para definir características y factores relacionados (plan de cuidados individualizado de enfermería) de una paciente de 50 años con encefalopatía de Wernicke-Korsakoff.
MétodoRevisión integradora de literatura acerca de la encefalopatía de Wernicke-Korsakoff, para la valoración de enfermería, basada en la Teoría General sobre el Déficit de Autocuidado de Dorothea Orem al ingreso en la unidad de Neurología de un hospital español de tercer nivel.
ResultadosSe propone un plan de cuidado individualizado a través de las taxonomías NANDA-NOC-NIC siguiendo el proceso enfermero. Destaca la importancia de la atención al cuidador principal, debido su responsabilidad en la continuidad de los cuidados al alta, incluyendo para ello una propuesta de actividades específicas.
ConclusionesEs necesario el uso de taxonomías estandarizadas para el desarrollo de la disciplina científica de enfermería, junto a un abordaje holístico para la individualización de los cuidados.