Cluster headache was described by B.T. Horton as a strong unilateral pain in the orbital region of cyclical predominance, which affects mainly men. The structural and functional abnormalities of its aetiology are not exactly known, although it is related to an autosomal gene. The diagnosis is based on the patient's symptoms and the treatment on pain management and suppression of the precipitating factors of the episode.
ObjectiveTo develop a nursing care plan for patients with cluster headaches and establish health-promoting behaviour.
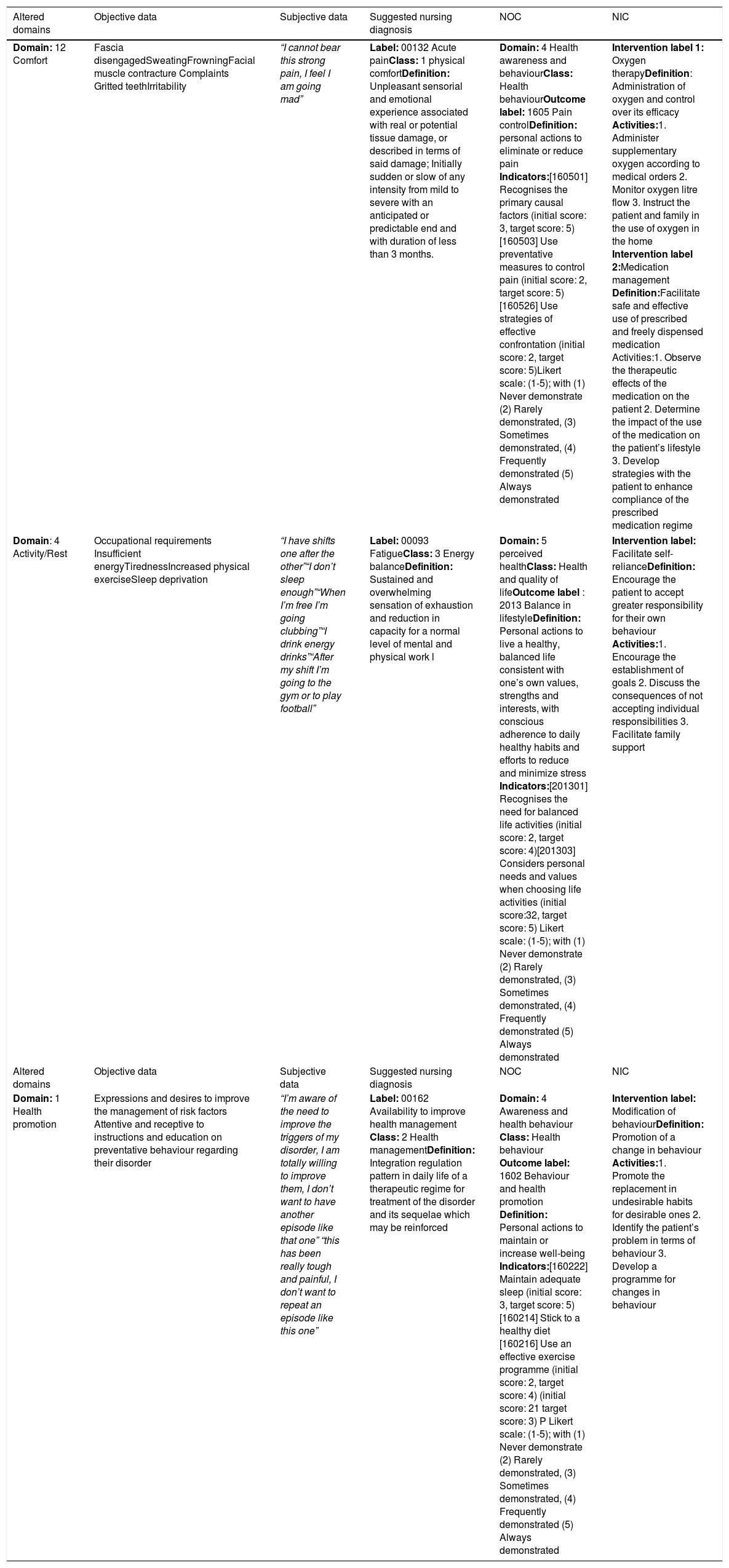
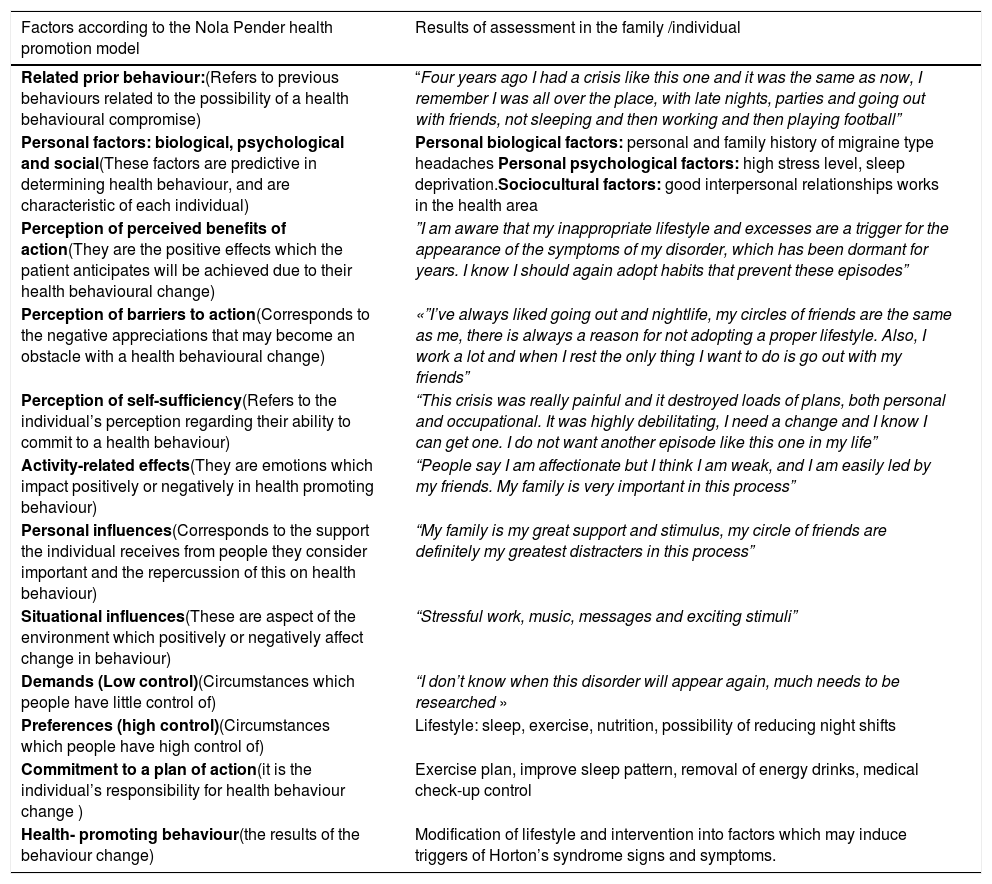
MethodologyA review of the literature on cluster headache was conducted. Based on the Nanda International domain assessment taxonomy, Nursing Outcomes Classification (NOC) and Nursing Interventions Classification (NIC), an individualized care plan was developed. Next, the Nola Pender Health Promotion Model was applied to the patient to promote health-promoting behaviours.
ResultsThe nursing process is described starting from the diagnoses of pain, fatigue, knowledge, and health behaviour with their respective objectives, interventions, and nursing actions. Improvement was evidenced when the patient was administered 50% venturi oxygen at 15 L per min, for 30 min; topiramate every 12 h and generation of healthy behaviours based on the Health Promotion Model proposed by Pender.
ConclusionsThe importance of not only addressing the severity of the clinical picture is highlighted, but also the promotion of appropriate lifestyles on risk factors that trigger the disease.
La cefalea en racimos fue descrita por B.T. Horton como un fuerte dolor unilateral en la región orbitaria de predominio cíclico, que afecta principalmente a hombres. No se conoce exactamente las anormalidades estructurales y funcionales de su etiología, aunque se relaciona con un gen autosómico. El diagnóstico se basa en la clínica del paciente y el tratamiento en el manejo del dolor y supresión de los factores precipitantes del episodio.
ObjetivoDesarrollar plan de cuidados de enfermería paciente con cefalea en racimos y establecer una conducta promotora de salud.
MetodologíaSe realizó revisión de la literatura sobre la cefalea en racimos. Basados en la taxonomía de valoración por dominios de Nanda Internacional, clasificación de Resultados de Enfermería (NOC) y clasificación de Intervenciones de Enfermería (NIC), se desarrolló un plan de cuidados individualizado. Seguidamente se aplicó en el paciente el Modelo de Promoción de la salud de Nola Pender con el fin de promover conductas promotoras de salud.
ResultadosSe describe proceso de enfermería partiendo de los diagnósticos dolor, fatiga y conocimiento y conducta de salud con sus respectivos objetivos, intervenciones y acciones de enfermería. Se evidenció mejoría al administrar al paciente oxígeno venturi al 50% a 15 litros por minuto, por 30 minutos; topiramato cada 12 horas y generación de conductas saludades orientadas desde el Modelo de Promoción de la Salud propuesto por Pender.
ConclusionesSe resalta la importancia no solo del abordaje en la severidad del cuadro clínico, sino de la promoción de los estilos de vida adecuados sobre factores de riesgos desencadenantes de la enfermedad.