Although the advanced age is not an exclusion criterion for the stroke treatments, is characterized by a frailty state that affected the evolution and prognosis in such patients.
ObjectivesTo describe the possibility of a relation between frailty in elderly people (≥ 80 years old) after mechanical thrombectomy, and clinical severity, and to describe stroke clinical features.
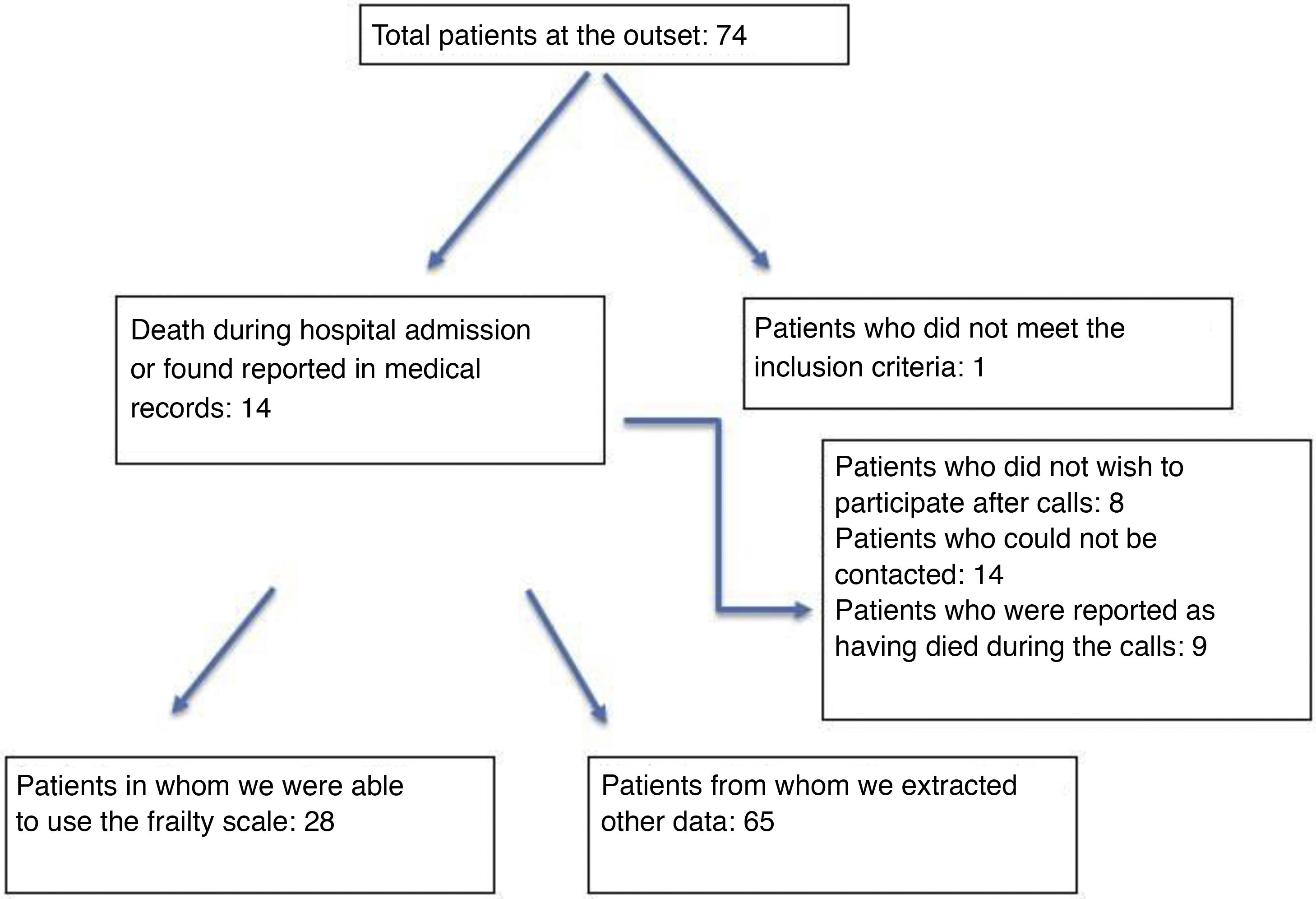
MethodsObservational study in people over 80 year-old who suffered an ischemic stroke and underwent to mechanical thrombectomy, between February and October 2018. Data about cardiovascular risk factors, medical treatment, stroke episode and frailty were collected.
ResultsThe sample was constituted by 65 people. A 72% suffered hypertension and 43% atrial fibrillation. A 75% did not take anticoagulants. A 82% did not suffer complications with the procedure, and a complete arterial reperfusion was achieved in 83%. A 27.69% (n = 28) was not fragile. There was statistical association between age and frailty (P = .003).
DiscussionIn our sample, the neurological and functional state caused by the stroke were more severe (described by the NIHS and Rankin modified scales score), but the recovery after hospital discharge was more positive. Elderly survivor patients were characterized as no fragile. The recovery after a stroke should be measured in functionality and quality of life terms, and not only using the age data.
Aunque la edad en el ictus no condiciona los tratamientos de reperfusión, lleva implícitamente una fragilidad que condiciona el estado funcional y probablemente el pronóstico y la evolución.
ObjetivosEstudiar la fragilidad en pacientes con ictus isquémico tratados con trombectomía mecánica y de ≥ 80 años de edad.
MétodoEstudio observacional en población ≥ 80 años tras sufrir un ictus isquémico y tratarse con trombectomía mecánica, entre febrero y octubre de 2018. Se recogieron variables sobre factores de riesgo cardiovascular, tratamiento concomitante, datos correspondientes al episodio del ictus (gravedad neurológica y funcional con las escalas NIHS y Rankin modificada) y fragilidad (entrevista telefónica, enero-febrero 2019).
ResultadosLa muestra fue de 65 personas. El 72% padecían hipertensión arterial y el 43%, fibrilación auricular. El 75% no estaban a tratamiento anticoagulante. El 78% fueron tratados antes de 6 h. El 82% no sufrieron complicaciones neurológicas. Se consiguió una reperfusión arterial completa en el 83%. El 27,69% puntuaron como no frágil (n = 28). Se observó relación estadística entre la fragilidad y la edad (p = 0,003).
DiscusiónA nivel neurológico y funcional los ictus presentaban puntuaciones mayores (más graves) en las escalas NIHS y Rankin modificada respecto a otros estudios de investigación. Los pacientes más mayores que sobrevivieron al ictus son en su mayoría no frágiles, por lo que la recuperación debería medirse en términos de funcionalidad y calidad de vida y no tanto en base a la edad cronológica.
Article
Diríjase al área privada de socios de la web de la SEDENE, (https://sedene.com/revista-de-sedene/ ) y autentifíquese.