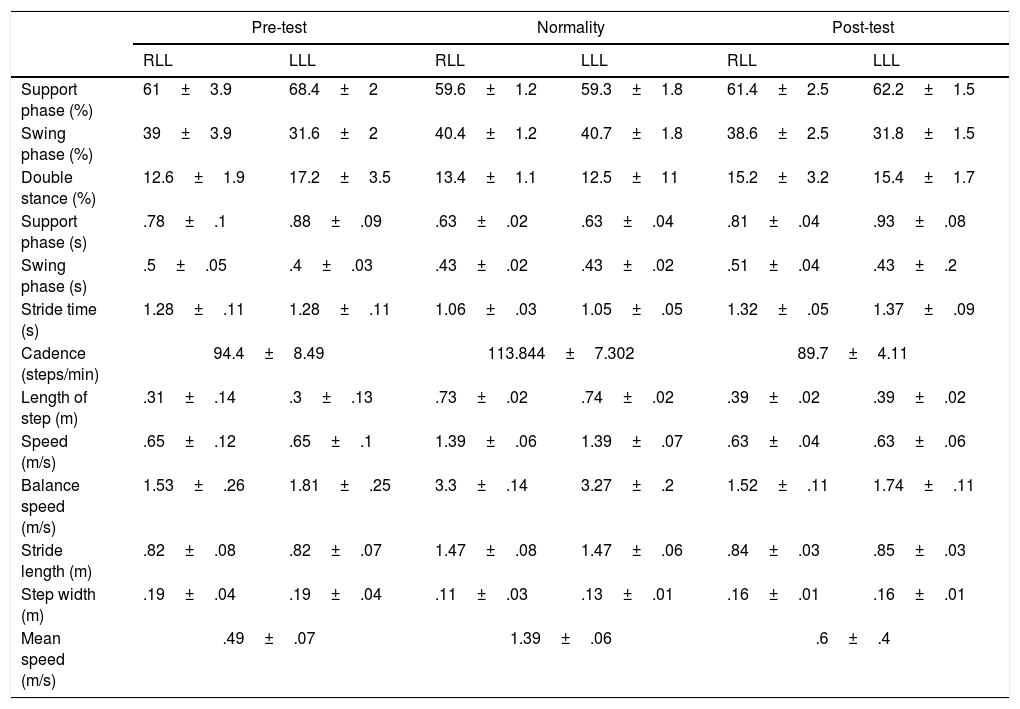
Multiple sclerosis is an autoimmune disease that causes progressive disability in young adults, in which they experience motor and sensory dysfunctions that contribute to alterations in balance and gait. The aim of this study is to determine these alterations in a 29-year-old patient with primary progressive multiple sclerosis, and to describe and implement a physiotherapeutic intervention (40min/day, 2 days/week for 5 months), and objectify the results through instrumental gait analysis. An increase was obtained in the muscular balance (Daniels Test) in the right lower limb, and in balance using the Berg Balance Scale (6 points), as well as a decrease in spasticity in the Modified Ashworth Scale in the right triceps surae. There was also an improvement in the spatiotemporal gait parameters, an increase in average speed by 0.11m, a decrease of 4.7 steps/min of the cadence, a decrease in step width by 0.03m, and an increase in stride lengths (0.08m right, 0.09m left). The data suggested a functional improvement, even in the case of a progressive disease. The joint action of an interdisciplinary team is essential to reinforce the physiotherapy treatment in these patients, as well as the use of innovative assessment tools that allow us to achieve the most optimal treatments.
La esclerosis múltiple es una enfermedad autoinmune que causa discapacidad progresiva en adultos jóvenes, quienes experimentan disfunciones motoras y sensitivas que contribuyen a las alteraciones del equilibrio y de la marcha. El objetivo del presente estudio es determinar estas alteraciones en una paciente de 29 años de edad con esclerosis múltiple progresiva primaria, describir e implementar una intervención fisioterapéutica (40min/día, 2 días/semana durante 5 meses) y objetivar los resultados mediante un sistema de análisis instrumentalizado de la marcha. Se obtuvo un aumento en el balance muscular (test de Daniels) en el miembro inferior derecho y el equilibrio (6 puntos) mediante la escala del equilibrio de Berg, y una disminución de la espasticidad en la escala modificada de Ashworth en el tríceps sural derecho. Los parámetros espacio-temporales de la marcha mejoraron: aumento de la velocidad media en un 0,11m/s, disminución de 4,7 pasos/minuto en la cadencia, disminución de la anchura del paso en 0,03m y aumento 0,08m en la longitud de paso derecho y de 0,09m en el izquierdo. Los datos implicaron una mejora funcional, aun tratándose de una enfermedad progresiva. Resulta fundamental una actuación conjunta del equipo interdisciplinar para reforzar el tratamiento de fisioterapia en estos pacientes, así como el uso de herramientas de evaluación innovadoras que nos permitan implementar los tratamientos más óptimos.
Article
Diríjase al área privada de socios de la web de la SEDENE, (https://sedene.com/revista-de-sedene/ ) y autentifíquese.