Although same-day discharge (SDD) after elective uncomplicated percutaneous coronary intervention (PCI) be adopted worldwide, it remains poorly studied in our country. We aim to evaluate our initial experience with SDD after elective PCI, regarding its safety and predictors of success.
MethodsA hundred and sixty-one single-center consecutive patients, selected in a specialized outpatient clinic, were included for SDD. To identify the factors associated with SDD, single and multiple logistic regression models were adjusted.
ResultsSDD was successfully performed in 114 patients (70.8%) and the remaining 47 patients remained hospitalized (45 with discharge in the following morning and 2 patients after 2 days). No patient with SDD presented major adverse cardiac events or major vascular complications at 30 days or at a median follow-up of 12 months. In the inpatient group, there was only one case of acute myocardial infarction due to a lateral branch occlusion and two patients with > 5cm hematoma related to the access site. The SDD predictors were radial access route (OR = 5.92; 95%CI 1.73-20.21; p = 0.005), presence of type A/B1 lesions (OR = 14.09; 95%CI 1.70-116.49%; p = 0.01) and contrast volume (OR = 0.76; 95%CI 0.65-0.88; p < 0.001).
ConclusionsSDD was safe and could be successfully performed in most patients selected for elective PCI, and its predictors were the radial access, less complex coronary lesions and a and lower contrast volume.
Apesar de a alta hospitalar no mesmo dia (AHMD) após intervenção coronária percutânea (ICP) eletiva não complicada ser adotada mundialmente, ela permanece pouco estudada em nosso meio. Objetivamos, assim, avaliar nossa experiência inicial com a AHMD após ICP eletiva, em relação à sua segurança e aos preditores de sucesso.
MétodosForam incluídos 161 pacientes consecutivos para AHMD, de único centro, selecionados em ambulatório especializado. Para a identificação dos fatores associados ao sucesso da AHMD, foram ajustados modelos de regressão logística simples e múltipla.
ResultadosA AHMD foi realizada com sucesso em 114 pacientes (70,8%), tendo os 47 pacientes restantes permanecido internados (45 com alta na manhã seguinte e 2 pacientes após 2 dias). Nenhum paciente com AHMD apresentou evento cardíaco adverso maior ou complicação vascular importante aos 30 dias e no seguimento mediano de 12 meses. No grupo internação, ocorreu apenas um caso de infarto agudo do miocárdio por oclusão de ramo lateral e dois hematomas > 5cm relacionados ao sítio de punção. Os preditores de sucesso da AHMD foram: via de acesso radial (OR = 5,92; IC95% 1,73-20,21; p = 0,005), presença de lesões tipo A/B1 (OR = 14,09; IC95% 1,70-116,49; p = 0,014) e volume de contraste (OR = 0,76; IC95% 0,65-0,88; p < 0,001).
ConclusõesA AHMD foi segura e pôde ser realizada com sucesso na maioria dos pacientes selecionados para ICP eletiva, sendo seus preditores de sucesso o acesso radial, as lesões menos complexas e um volume menor de contraste.
Since it was first performed more than three decades ago, percutaneous coronary intervention (PCI) has become the most widely used method for coronary revascularization worldwide. Technique improvement, together with the technological advancement of dedicated materials and effectiveness of adjunctive medication, greatly improved procedure safety and success, reducing complications and resulting in shorter hospital stay.1–5
These technological advances, however, allowed for the increasing number of PCIs and led to greater costs, resulting in hospital management policies directed at cost reduction logistics, while preserving clinical efficacy, safety, and patient satisfaction with the procedure.6–9 In this sense, previous studies have shown a significant reduction in PCI-related costs, including selected elective patients with low risk of complications in a same-day hospital discharge (SDD) program.10 The concept of SDD has been evaluated in several studies, which were grouped in a recent meta-analysis that confirmed the safety and efficacy of SDD in comparison with overnight in-hospital observation for uncomplicated elective PCIs.11,12
SDD in uncomplicated PCIs, although well established in the practice of global interventional cardiology,11 remains little studied and used in Brazil.13 Additionally, there are few data in the literature about predictors of success in the implementation of such practice. In this sense, the aims of this study were to evaluate an initial experience with SDD after elective PCI regarding its safety and predictors of success.
MethodsStudy populationConsecutive patients referred for elective angioplasty between March 2013 and November 2014 (n = 459), from a single center, were evaluated as outpatients by an interventional cardiologist from this service (F.C.) before PCI. The study was approved by the Research Ethics Committee of the institution and all patients signed an informed consent prior to the procedure.
Based on the appropriateness criteria for PCI performance14 and previous SDD studies,2,7,11,12,15,16 the following criteria were applied, with the intention of selecting patients eligible for the study: (1) presence of stable angina, crescendo angina or asymptomatic patients with positive functional test for ischemia; (2) elective angioplasty of one or two vessels; (3) absence of significant medical comorbidities that would justify the need for a longer hospital stay to prepare the patient for the procedure and post-angioplasty care, such as heart failure and ejection fraction < 35%, chronic renal failure (creatinine clearance < 60mL/min), hemorrhagic diathesis or known bleeding disorders, symptomatic chronic obstructive pulmonary disease, allergy to contrast, frailty and/or age > 80 years; (4) low- or intermediate-complexity coronary anatomy (SYNTAX score < 33) that did not involve the left main coronary artery or lesions in bifurcations scheduled to be treated with two stents; (5) possibility to perform the procedure through radial access, or via the femoral access, preferably with a 5F sheath.
After the procedure, the following criteria were considered for SDD: no complications during PCI; absence of prolonged chest pain during the procedure or chest pain in the recovery period post-PCI; no elevation in myocardial necrosis markers 6hours after the procedure or new electrocardiographic alteration suggesting ischemia; absence of vascular complications or hematoma > 5cm related to the puncture site; PCIs preferably performed in the morning, due to the recovery time considering the vascular access.
ProcedureFor patients eligible for SDD, the antiplatelet agent used was clopidogrel 300mg as loading dose, administered 24hours before the procedure (with an additional dose of 300mg immediately after the PCI), followed by 75mg/day for at least 30 days for bare-metal stents or one year for drug-eluting stents. For patients that were already using clopidogrel, an additional dose of 300mg was administered at the end of the procedure. For those receiving ticagrelor or prasugrel, 90 and 10mg were administered at the end of the procedure, respectively. Additionally, patients were prescribed acetylsalicylic acid (100mg per day) indefinitely. The transradial approach was the most commonly used, with the transfemoral approach used as an alternative when it was impossible to use the transradial approach or when it failed. After obtaining vascular access (5F or 6F sheath), unfractionated heparin was administered at a dose of 100 IU/kg. Glycoprotein IIb/IIIa inhibitors were not used. The procedure followed the currently established technique, using direct stenting whenever possible. After the PCI, the sheaths were immediately removed. For the transfemoral approach, a protamine dose was administered (1mL of Protamine 1000TM to neutralize 1,000 IU of heparin) and the sheath was removed with manual compression for 15 to 30minutes, followed by compressive dressing and limb rest for at least four hours. In the case of transradial approach, a hemostatic strap (TR BandTM; Terumo Medical Co., Elkton, USA) was used, followed by limb rest for 2hours. Post-procedure control included an electrocardiogram (compared to an electrocardiogram performed prior to PCI), vital signs, and physical examination of the access route. High-sensitivity troponin measurement was performed 6hours after the procedure in all patients eligible for SDD. Patients that remained asymptomatic without electrocardiographic alterations or significant increase in troponin levels and no complications at the puncture site were discharged, with recommendations on medication, additional rest periods, possible complications, and outpatient return visit for reassessment. In case of any signs or symptoms related to the procedure, they were advised to seek the emergency service of this hospital.
Data collection and analysisThe study data collection was performed by nurses and doctors trained during the index hospitalization, following the completion of previously standardized forms. Data collection included clinical characteristics, laboratory test results, data on the invasive procedure, and clinical outcome until hospital discharge. After discharge, clinical follow-up of patients was performed on an outpatient basis within 30 days of the procedure and, thereafter, by telephone contact and review of hospital records.
All angiograms were analyzed by the Hemodynamics and Interventional Cardiology Service of the hospital where the study was conducted to determine procedure success, vessel measurements and characteristics, as well as angiographic adverse events (F.C. and H.B.R.). Image acquisition was performed using two or more angiographic projections of the stenosis after nitrate administration. These projections were repeated at the time of the follow-up angiography in cases where necessary. Qualitative morphological characteristics were assessed using standardized criteria.17,18
Outcomes and definitionsThe primary safety outcome was the occurrence of major adverse cardiac events (death, acute myocardial infarction – AMI) and reintervention, as well as stent thrombosis rate, hospital readmission, and vascular complications at 30 days. These outcomes were also evaluated in the late follow-up period of 12 months, as well as predictors of SDD, based on clinical and angiographic characteristics and in-hospital outcomes.
The deaths included cardiac and non-cardiac causes. The diagnosis of AMI with ST-segment elevation, stable angina, and unstable angina followed previously described criteria.17,18 Increase in markers > 5 times the upper limit of normality (ULN of troponin of 0.01μg/L) was considered a significant troponin elevation.19 Angiog-raphic success was defined as achieving a target lesion < 30%, while maintaining or restoring the normal antegrade flow (Thrombolysis In Myocardial Infarction –TIMI 3). Target-lesion revascularization was defined as a new intervention, surgical or percutaneous, in lesions > 50% within the previously implanted stent or in the segment that included the 5mm proximal and/or 5mm distal to the stent. Stent thrombosis was defined according to the classification of the Academic Research Consortium.20
Intra-procedure complications included prolonged chest pain, hemodynamic instability, transient vessel occlusion, no-reflow and slow-flow phenomenon, side branch occlusion > 1.5mm, and suboptimal angiographic result. The lesions were classified into types A, B1, B2 and C, according to the American College of Cardiology/American Heart Association (ACC/AHA).21 Vascular complications included major bleeding according to TIMI classification (intracranial hemorrhage or decrease > 5mg/dL of hemoglobin or 15% of hematocrit), significant hematoma at the puncture site > 5cm, pseudoaneurysm, fistula, or thrombosis requiring surgical intervention.15
Statistical analysisCategorical variables were expressed as frequencies and percentages, and compared with the Chi-squared test. Continuous variables were described as mean and standard deviations, or median and interquartile range (25th and 75th percentiles), and were compared with Student's t-test or analysis of variance (ANOVA). Univariate and multivariate models using binary logistic regression were used to identify predictors of SDD success, with the variables showing a value of p < 0.05 included in the multivariate model. All tests were two-tailed and a p-value of < 0.05 was considered statistically significant. Analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago, USA).
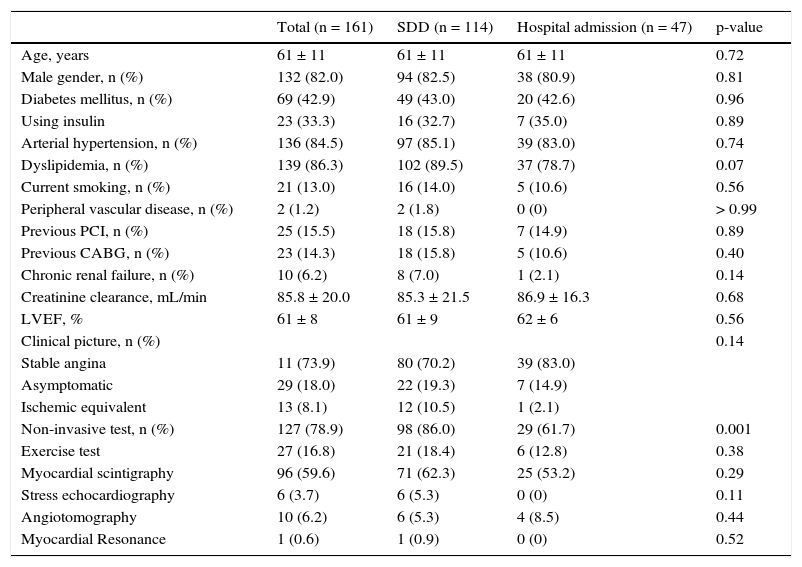
ResultsDuring the study period, 161 patients were selected for SDD, and this strategy was adopted successfully in 114 patients (70.8%); the remaining 47 patients (29.2%) remained hospitalized (45 discharged in the following morning and 2 patients after two days). Clinical characteristics of the overall study population, as well as in relation to SDD groups and hospitalization, are shown in Table 1. Both groups were very similar, with a majority of male patients, mean age of 61 ± 11 years, and high prevalence of diabetes (42.9%). Most patients had stable angina (73.9%) and preserved left ventricular ejection fraction (61% ± 9% vs. 62% ± 6%, p = 0.56).
Basal clinical characteristics.
| Total (n = 161) | SDD (n = 114) | Hospital admission (n = 47) | p-value | |
|---|---|---|---|---|
| Age, years | 61 ± 11 | 61 ± 11 | 61 ± 11 | 0.72 |
| Male gender, n (%) | 132 (82.0) | 94 (82.5) | 38 (80.9) | 0.81 |
| Diabetes mellitus, n (%) | 69 (42.9) | 49 (43.0) | 20 (42.6) | 0.96 |
| Using insulin | 23 (33.3) | 16 (32.7) | 7 (35.0) | 0.89 |
| Arterial hypertension, n (%) | 136 (84.5) | 97 (85.1) | 39 (83.0) | 0.74 |
| Dyslipidemia, n (%) | 139 (86.3) | 102 (89.5) | 37 (78.7) | 0.07 |
| Current smoking, n (%) | 21 (13.0) | 16 (14.0) | 5 (10.6) | 0.56 |
| Peripheral vascular disease, n (%) | 2 (1.2) | 2 (1.8) | 0 (0) | > 0.99 |
| Previous PCI, n (%) | 25 (15.5) | 18 (15.8) | 7 (14.9) | 0.89 |
| Previous CABG, n (%) | 23 (14.3) | 18 (15.8) | 5 (10.6) | 0.40 |
| Chronic renal failure, n (%) | 10 (6.2) | 8 (7.0) | 1 (2.1) | 0.14 |
| Creatinine clearance, mL/min | 85.8 ± 20.0 | 85.3 ± 21.5 | 86.9 ± 16.3 | 0.68 |
| LVEF, % | 61 ± 8 | 61 ± 9 | 62 ± 6 | 0.56 |
| Clinical picture, n (%) | 0.14 | |||
| Stable angina | 11 (73.9) | 80 (70.2) | 39 (83.0) | |
| Asymptomatic | 29 (18.0) | 22 (19.3) | 7 (14.9) | |
| Ischemic equivalent | 13 (8.1) | 12 (10.5) | 1 (2.1) | |
| Non-invasive test, n (%) | 127 (78.9) | 98 (86.0) | 29 (61.7) | 0.001 |
| Exercise test | 27 (16.8) | 21 (18.4) | 6 (12.8) | 0.38 |
| Myocardial scintigraphy | 96 (59.6) | 71 (62.3) | 25 (53.2) | 0.29 |
| Stress echocardiography | 6 (3.7) | 6 (5.3) | 0 (0) | 0.11 |
| Angiotomography | 10 (6.2) | 6 (5.3) | 4 (8.5) | 0.44 |
| Myocardial Resonance | 1 (0.6) | 1 (0.9) | 0 (0) | 0.52 |
SDD: same-day discharge; PCI: percutaneous coronary intervention; CABG: coronary artery bypass graft surgery; LVEF: left ventricular ejection fraction.
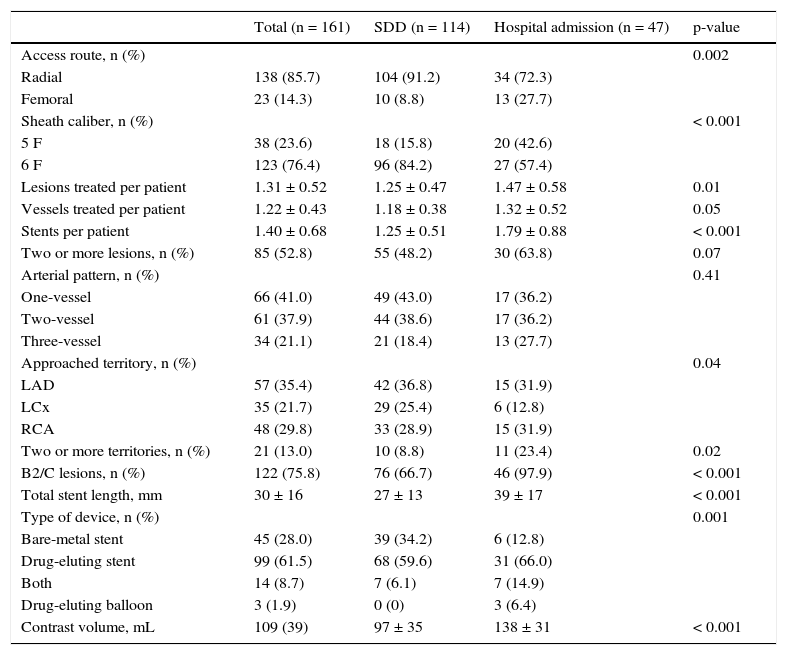
Angiographic characteristics are shown in Table 2. Transradial access and 6F sheath were more often used in the SDD group (91.2% vs. 72.3%; p = 0.002; and 84.2% vs. 57.4%; p < 0.001, respectively). Although both groups had similar arterial patterns, the complexity of the interventions was lower in the SDD group when compared to the hospital admission group. This was demonstrated by the lower number of lesions treated per patient (1.25 ± 0.47 vs. 1.47 ± 0.58; p=0.01), the lower complexity of lesions (B2/C type lesions 66.7% vs. 97.9%; p<0.01), and the lower number of stents/patient (1.25 ± 0.51 vs. 1.79 ± 0.88; p < 0.001).
Angiographic characteristics.
| Total (n = 161) | SDD (n = 114) | Hospital admission (n = 47) | p-value | |
|---|---|---|---|---|
| Access route, n (%) | 0.002 | |||
| Radial | 138 (85.7) | 104 (91.2) | 34 (72.3) | |
| Femoral | 23 (14.3) | 10 (8.8) | 13 (27.7) | |
| Sheath caliber, n (%) | < 0.001 | |||
| 5 F | 38 (23.6) | 18 (15.8) | 20 (42.6) | |
| 6 F | 123 (76.4) | 96 (84.2) | 27 (57.4) | |
| Lesions treated per patient | 1.31 ± 0.52 | 1.25 ± 0.47 | 1.47 ± 0.58 | 0.01 |
| Vessels treated per patient | 1.22 ± 0.43 | 1.18 ± 0.38 | 1.32 ± 0.52 | 0.05 |
| Stents per patient | 1.40 ± 0.68 | 1.25 ± 0.51 | 1.79 ± 0.88 | < 0.001 |
| Two or more lesions, n (%) | 85 (52.8) | 55 (48.2) | 30 (63.8) | 0.07 |
| Arterial pattern, n (%) | 0.41 | |||
| One-vessel | 66 (41.0) | 49 (43.0) | 17 (36.2) | |
| Two-vessel | 61 (37.9) | 44 (38.6) | 17 (36.2) | |
| Three-vessel | 34 (21.1) | 21 (18.4) | 13 (27.7) | |
| Approached territory, n (%) | 0.04 | |||
| LAD | 57 (35.4) | 42 (36.8) | 15 (31.9) | |
| LCx | 35 (21.7) | 29 (25.4) | 6 (12.8) | |
| RCA | 48 (29.8) | 33 (28.9) | 15 (31.9) | |
| Two or more territories, n (%) | 21 (13.0) | 10 (8.8) | 11 (23.4) | 0.02 |
| B2/C lesions, n (%) | 122 (75.8) | 76 (66.7) | 46 (97.9) | < 0.001 |
| Total stent length, mm | 30 ± 16 | 27 ± 13 | 39 ± 17 | < 0.001 |
| Type of device, n (%) | 0.001 | |||
| Bare-metal stent | 45 (28.0) | 39 (34.2) | 6 (12.8) | |
| Drug-eluting stent | 99 (61.5) | 68 (59.6) | 31 (66.0) | |
| Both | 14 (8.7) | 7 (6.1) | 7 (14.9) | |
| Drug-eluting balloon | 3 (1.9) | 0 (0) | 3 (6.4) | |
| Contrast volume, mL | 109 (39) | 97 ± 35 | 138 ± 31 | < 0.001 |
SDD: same-day discharge; LAD: left anterior descending artery; LCx: left circumflex artery; RCA: right coronary artery.
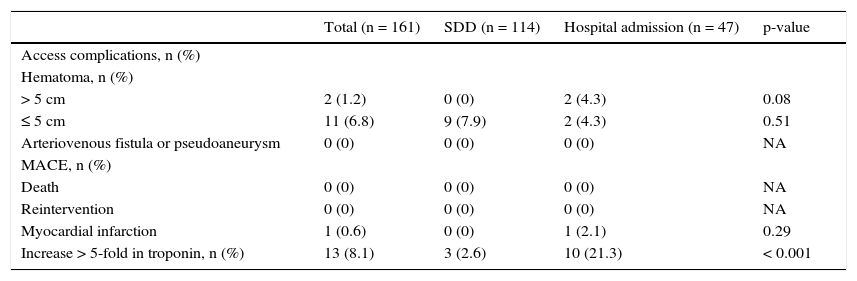
Hospital outcomes are shown in Table 3. Regarding access route complications, hematomas > 5cm were observed in 2 patients from the hospital group in the first 12hours after the intervention, and small hematomas (< 5cm) in 11 patients, 9 in the SDD group and 2 the hospital admission group (p = 0.51). There were no cases of pseudoaneurysm or arteriovenous fistula in either group. Increased troponin > 5 times the ULN, although an exclusion criterion for SDD, occurred in 2.6% of cases in this group. Regarding major adverse cardiac complications, there was only 1 case of AMI in the hospitalization group due to side branch occlusion, associated with chest pain, electrocardiographic alterations, and elevation of myocardial necrosis markers. There were no deaths or reinterventions in either group up to a median follow-up period of 12 months (6.2 to 28.7 months).
In-hospital outcomes.
| Total (n = 161) | SDD (n = 114) | Hospital admission (n = 47) | p-value | |
|---|---|---|---|---|
| Access complications, n (%) | ||||
| Hematoma, n (%) | ||||
| > 5 cm | 2 (1.2) | 0 (0) | 2 (4.3) | 0.08 |
| ≤ 5 cm | 11 (6.8) | 9 (7.9) | 2 (4.3) | 0.51 |
| Arteriovenous fistula or pseudoaneurysm | 0 (0) | 0 (0) | 0 (0) | NA |
| MACE, n (%) | ||||
| Death | 0 (0) | 0 (0) | 0 (0) | NA |
| Reintervention | 0 (0) | 0 (0) | 0 (0) | NA |
| Myocardial infarction | 1 (0.6) | 0 (0) | 1 (2.1) | 0.29 |
| Increase > 5-fold in troponin, n (%) | 13 (8.1) | 3 (2.6) | 10 (21.3) | < 0.001 |
SDD: same-day discharge; MACE: major adverse cardiac events; NA: not applicable.
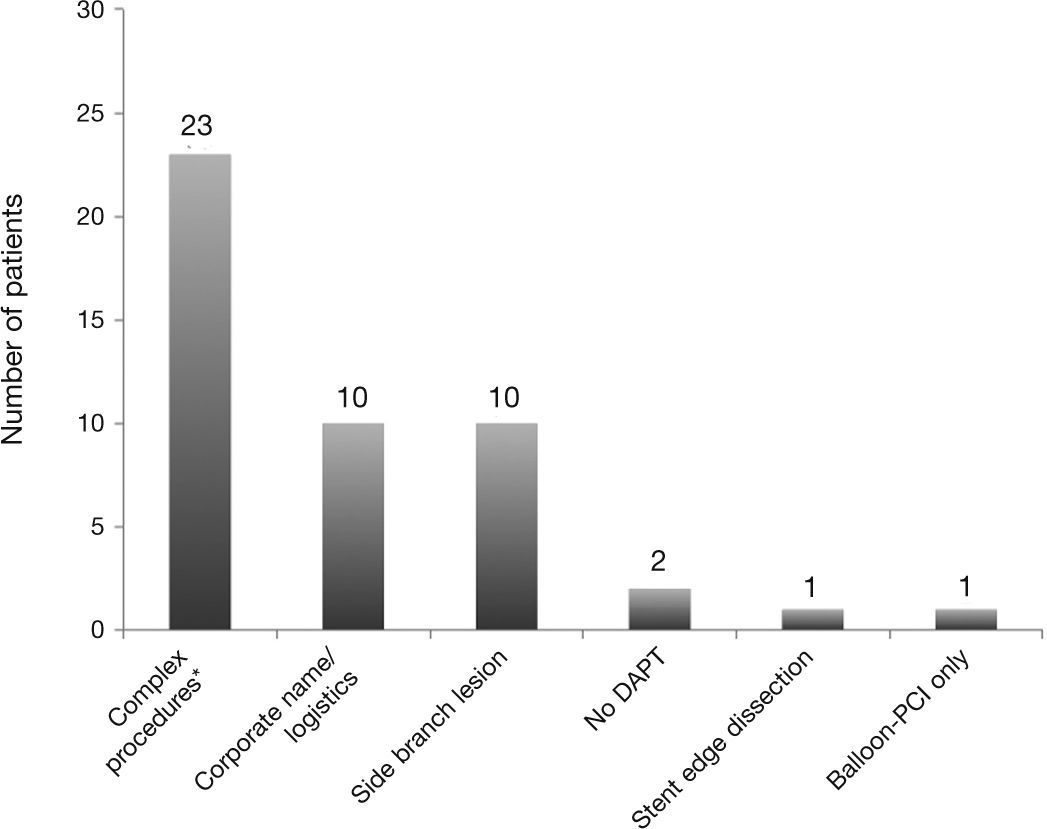
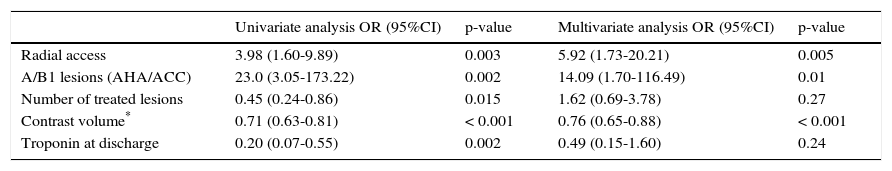
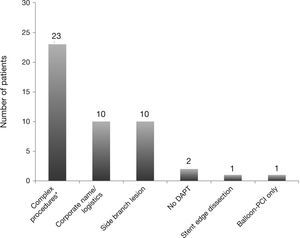
The main reasons for SDD failure in this population are shown in the Figure 1. Independent predictors of SDD success at the multivariate analysis are shown in Table 4. Transradial access (OR = 5.920; 95%CI 1.73-20.21; p = 0.005), the presence of A/B1 lesions (OR = 14.09; 95%CI 1.70-116.49; p = 0.01), and contrast volume (OR = 0.76; 95%CI 0.65-0.88; p < 0.001) were factors related to SDD.
Same-day hospital discharge success predictors.
| Univariate analysis OR (95%CI) | p-value | Multivariate analysis OR (95%CI) | p-value | |
|---|---|---|---|---|
| Radial access | 3.98 (1.60-9.89) | 0.003 | 5.92 (1.73-20.21) | 0.005 |
| A/B1 lesions (AHA/ACC) | 23.0 (3.05-173.22) | 0.002 | 14.09 (1.70-116.49) | 0.01 |
| Number of treated lesions | 0.45 (0.24-0.86) | 0.015 | 1.62 (0.69-3.78) | 0.27 |
| Contrast volume* | 0.71 (0.63-0.81) | < 0.001 | 0.76 (0.65-0.88) | < 0.001 |
| Troponin at discharge | 0.20 (0.07-0.55) | 0.002 | 0.49 (0.15-1.60) | 0.24 |
OR: odds ratio; 95%CI: 95% confidence interval; AHA/ACC: American Heart Association/American College of Cardiology.
* For each increment of 10mL of contrast volume.
The present study aimed to evaluate an initial experience with SDD after elective PCI regarding its safety, as well as predictors of success. In a consecutive population of 161 pre-PCI patients selected from the outpatient clinic, SDD was successfully applied to the majority of patients (71%), and the rate of major adverse cardiac event was low in both groups (SDD and hospital admission), while no events were observed in the patients from the SDD group. SDD success predictors were the use of transradial access, less complex angiographic lesions, and lower volume of contrast used.
Since the first reports of success almost two decades ago,22 SDD practice has faced a number of barriers for its implementation as a viable strategy in elective patients undergoing PCI. The concerns included forensic safety issues, patient preference and satisfaction, and cost analysis.23–27 Nevertheless, several studies over the last few years have evaluated the practice of SDD, with quite interesting results. These results were grouped into an important meta-analysis by Abdelaal et al.,11 involving five randomized and eight observational trials, with a total of 111,830 patients included. Although different methods of SDD practice have been observed among the assessed studies, its broad applicability was demonstrated, with low rates of cardiovascular adverse events, repeated hospitalizations, and overall complications, confirming it as a viable alternative in uncomplicated elective PCIs.
The experience with SDD is small in Brazil.13 In the present study, which evaluated consecutive patients selected for SDD, it was possible in 71%, whereas 29% were hospitalized and discharged on the following day. This is somewhat higher than the rate of 10%-20% observed in the literature.15 When analyzing the main reasons that led patients to not have SDD, vascular access (femoral) and procedure complexity were the most important. Most SDD studies assessed the safety and efficacy of this strategy using the transradial approach, in order to minimize possible vascular access complications. In the present study, 85.7% of the patients were treated with the transradial approach and 14.3%, the transfemoral, with the latter increasing the chance of hospitalization by six-fold, although a smaller-caliber sheath (5 F) was used in most cases. Because of the shorter recovery time and clear benefits regarding vascular complication reduction, the transradial approach should be preferred when using SDD.11,16,28 However, the femoral approach is still widely used globally, especially in European countries, the USA, and many states of Brazil. Thus, early discharge with the transfemoral approach has been described with good safety in some studies and can also be used.12,29
The present study showed high safety regarding hospital outcomes 30 days after the procedure and at late follow-up, as previously demonstrated in the literature.11,16,30,31 There were only two cases of major vascular complications (hematoma > 5cm at the vascular access site) observed within 6hours after PCI and only one case of symptomatic AMI due to side branch occlusion during the procedure. There were no cases of death or reintervention at a median follow-up of 12 months. Additionally, among patients with significant troponin increase (8.1%), no clinical implication was observed related to the isolated elevation of these markers, with three of these patients receiving SDD and ten hospitalized for overnight observation. Heyde et al.,12 in a previous randomized trial, also observed low rate of adverse clinical events, none of which occurred between 6 and 24hours after the procedure, validating the reliability of the SDD monitoring only in the first 6hours. In Brazil, Trindade et al.,13 retrospectively evaluating 69 patients included in a SDD protocol, also demonstrated its safety after a mean observation period of 6.8hours; no clinical events were identified during a 30-day follow-up.
Building a successful SDD program requires the choice and involvement of a multidisciplinary team, as well as all health care professionals involved in patient care. The selection of these patients involves institutional re-education, naturally focused on a well-established program of pre-procedure screening, strengthening the doctor-patient-family relationship, with contingency planning for likely emergencies and thorough monitoring in the short and long term after the procedure. Considering this strategy, the pre-angioplasty assessment clinic was implemented in this hospital so that an interventional cardiologist could select the ideal candidates for the implementation of the SDD project. This patient selection showed, in the literature, to be capable of reducing post-PCI complications such as ischemic events (abrupt occlusion of major vessels and secondary branches, and dissections of borders), periprocedural infarction, and acute stent thrombosis, as well as reducing bleeding and vascular complications.28,32
LimitationsThis was a single-center study with a small sample and selected patients and, thus, potential selection biases may have influenced the results and its generalization to other centers with different characteristics may not be possible. In the present study, the degree of satisfaction was not assessed; it should be the subject of future studies. Hospital costs, as well as their potential reduction with SDD, were not specifically assessed in this study, and this should also be considered in future studies.
ConclusionsIn patients selected from an outpatient clinic, with low risk for PCI, the SDD strategy was achieved in most cases and was safe in this Brazilian hospital, regarding rates of major adverse cardiac events and vascular complications. Predictors of success were use of transradial access and less complex angiographic lesions – noting that the transradial access should be preferred and that patient selection is crucial. The increasing number of elective PCI procedures and the costs involved with this increase over the years make SDD a worthwhile logistics strategy to reduce hospital costs. In this sense, the results of the present study, consistent with several studies in the literature, indicate that SDD should be encouraged for low-risk patients undergoing elective PCI in Brazil.
Funding sourcesNone declared.
Conflicts of interestThe authors declare no conflicts of interest.