The radial approach has demonstrated superior benefits to the femoral approach in reducing vascular complications and bleeding events associated to percutaneous coronary interventions. However, because this is a more complex procedure, it requires a learning curve to get all of the advantages of the technique. The aim of this study was to present the characteristics of the procedures of a center that prioritizes the use of radial approach.
MethodsProspective registry of patients undergoing percutaneous coronary intervention (PCI) using the radial or ulnar access where angiographic success, technical failure, ischemic adverse events and severe bleeding rates were assessed. A pre-specified analysis of the group undergoing PCI for the right coronary artery was performed, comparing patients using Judkins right catheter (JR) or Amplatz catheters.
ResultsBetween April 2010 and May 2012, 1,117 patients underwent PCI, 1,040 (93.1%) by the radial approach and 50 (4.5%) by the ulnar approach. Sedation was performed in 58.5% of the patients, the crossover rate was 1.2%, and angiographic success was 96.2%. Extra backup catheters were used in 99.1% of PCIs for the left coronary artery, JR in 69.4% and Amplatz in 27.1% of the PCIs for the right coronary artery. When the JR and Amplatz were compared, longer procedure duration, longer fluoroscopy time, larger number of catheters, more frequent lesion predilation and higher number of implanted stents were observed in the group using Amplatz catheters as well as lower angiographic success rates.
ConclusionsThe use of radial access in PCI showed a high success rate and a low rate of major cardiac events and bleeding complications. The liberal use of sedation and 6F introducer sheaths, associated to catheters with stronger backup force, are characteristics of our center, which prioritizes the use of the radial approach.
Características Operacionais das Intervenções Coronárias Percutâneas emCentro que Prioriza a Utilização do Acesso Radial
IntroduçãoO acesso radial tem demonstrado resultados superiores aos do acesso femoral na redução de complicações vasculares e ocorrência de sangramentos associados aos procedimentos coronários percutâneos. Entretanto, por ser procedimento mais elaborado, requer dos operadores curva de aprendizagem para se obter todas as vantagens da técnica. O objetivo deste estudo foi apresentar as características dos procedimentos de um serviço que prioriza a utilização da via radial.
MétodosRegistro prospectivo de pacientes submetidos a intervenção coronária percutânea (ICP) pelo acesso radial ou ulnar, em que foram avaliados sucesso angiográfico do procedimento, falência da técnica, taxa de eventos adversos isquêmicos e sangramento grave. Análise pré-especificada do subgrupo que realizou ICP para coronária direita foi realizada, comparando pacientes que utilizaram cateteres Judkins de direita (JR) ou Amplatz.
ResultadosEntre abril de 2010 e maio de 2012, 1.117 pacientes realizaram ICP, 1.040 (93,1%) pela via radial e 50 (4,5%), pela ulnar. Sedação foi realizada em 58,5% dos pacientes, a taxa de crossover foi de 1,2% e o sucesso angiográfico, de 96,2%. Cateteres extra backup foram utilizados em 99,1% das ICPs para coronária esquerda, JR em 69,4%, e Amplatz em 27,1% das ICPs para coronária direita. Na comparação entre JR e Amplatz, observou-se maior duração do procedimento, tempo de fluoroscopia, número de cateteres, pré-dilatação da lesão e número de stents implantados no grupo que utilizou cateteres Amplatz, bem como menor sucesso angiográfico.
ConclusõesA utilização do acesso radial na ICP mostrou alto índice de sucesso e baixo índice de eventos cardíacos maiores e de complicações hemorrágicas. O emprego liberal da sedação e de introdutores 6F associado à escolha de cateteres com maior suporte são características operacionais de nosso centro, que prioriza o uso da técnica radial.
Percutaneous coronary intervention (PCI) through the radial access route was introduced approximately 20 years ago. 1 Multiple randomized studies have demonstrated superior results compared to the traditional femoral approach, particularly regarding a decrease in vascular complications and in the occurrence of severe bleeding. 2,3
The impact of periprocedural bleeding on clinical outcome, particularly with respect to increased mortality, resulted in a great interest in the radial technique. 4−6 Even in countries such as the United States, which has preferably used femoral access, there has been a progressive increase in the use of the radial approach, although its use today still accounts for less than 10% of all procedures. 7,8
The radial access, in turn, is technically more elaborate, demanding a longer learning period by the surgeons. 9−11 The knowledge of strategies employed in services that prioritize the use of the radial access, particularly regarding the choice of materials, can facilitate the implementation of this technique in new services. The objective of this study was to demonstrate the characteristics of procedures performed through radial access in a centre that prioritizes this type of access. 12
METHODSConsecutive patients undergoing PCI by radial and ulnar access were included in a prospective study of efficacy and safety. The outcomes of efficacy consisted of procedural success, defined as achieving a stenosis diameter of the target lesion < 20% associated with final Thrombolysis In Myocardial Infarction (TIMI) III flow without the need to change the access route (technique failure); rates of hospital mortality; reinfarction; stroke; and emergency heart surgery. The total procedure duration and fluoroscopy time were obtained from the beginning of arterial puncture until sheath removal. Safety was assessed by the occurrence of severe bleeding and vascular complications related to the puncture site. A pre-specified analysis was performed in the subgroup that underwent PCI for the right coronary artery, comparing patients using Judkins right (JR) and Amplatz catheters.
In accordance with the classification of the Bleeding Academic Research Consortium, 13 severe bleeding was defined as type 3 (3a, bleeding with a decrease in haemoglobin > 3g/dL and < 5g/dL or transfusion of packed red blood cells; 3b, bleeding with a decrease in haemoglobin > 5g/dL, cardiac tamponade, bleeding requiring surgical intervention or bleeding requiring intravenous vasoactive drugs; 3c, intracranial hemorrhage or subcategories confirmed by autopsy, imaging examination, lumbar puncture or intraocular bleeding with vision impairment); or Type 5 (5a, likely fatal bleeding; 5b definitive fatal bleeding). The hematomas were graded according to the classification of the Early Discharge after Transradial Stenting of Coronary Arteries (EASY) study: 14 type I, < 5cm in diameter; type II, < 10cm diameter; type III, > 10cm without reaching the elbow; type IV, hematoma extending beyond the elbow; type V, any hematoma with ischemic injury to the hand. Complications related to the puncture site, in addition to hematomas, included arteriovenous fistula, pseudoaneurysm, asymptomatic arterial occlusion, need for surgical vascular repair and site infection.
Through the hyperextension of the wrist and infiltration of 1 to 2mL of 2% xylocaine, the radial artery was punctured at 1cm proximal to the styloid process, using a needle with a 20–22 gauge Jelco ® polyethylene catheter (Smiths Medical – Kent, England) and the Seldinger technique. After puncture, a 0.021-inch guidewire was introduced, followed by a small skin incision with a scalpel blade number 11 and the insertion of a short sheath (< 11cm) 5–7F. A solution containing 5,000IU heparin sulphate and 10mg of isosorbide mononitrate was administered through the sheath extender. At the end of the procedure, the sheath was immediately removed, and hemostasis was obtained with a pressure dressing using a porous elastic adhesive bandage (Tensoplast ®, BSN Medical – Hamburg, Germany) or selective compressor band (TR Band™, Terumo Medical – Tokyo, Japan). Clinical examination of the puncture site and evaluation of the radial pulse were performed at the time of hospital discharge.
Sedation was achieved with midazolam (3ml-15mg), fentanyl (3ml-150μg), and saline (4ml). The initial dose used was 1mL of the solution, which was repeated as needed.
Statistical AnalysisCategorical variables were expressed as frequencies and percentages and compared using the chi-squared test. Continuous variables were expressed as the mean and standard deviation and compared using Student’s t-test or Fisher’s exact test. Values were considered statistically significant at P < 0.05.
RESULTSBetween April 2010 and May 2012, PCIs were performed in 1,117 patients, of which 1,090 (97.6%) were performed through radial and ulnar access; radial access was used in 1,040 (93.1%) cases and ulnar in 50 (4.5%) cases.
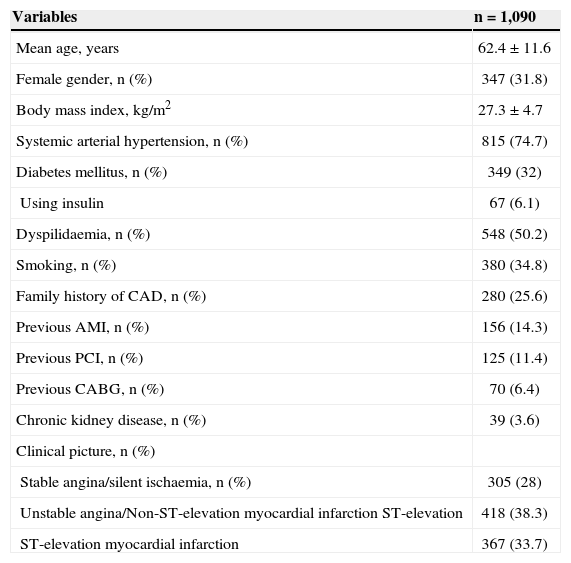
The demographic characteristics of the patients are indicated in Table 1. The mean age was 62.4±11.6years, 31.8% were females and 32% were diabetic. The predominant indication was acute coronary syndrome (72%), in which 38.3% were classified as unstable angina or acute myocardial infarction (AMI) without ST-segment elevation and 33.7% as AMI with ST-segment elevation.
Basal clinical characteristics
| Variables | n=1,090 |
|---|---|
| Mean age, years | 62.4±11.6 |
| Female gender, n (%) | 347 (31.8) |
| Body mass index, kg/m2 | 27.3±4.7 |
| Systemic arterial hypertension, n (%) | 815 (74.7) |
| Diabetes mellitus, n (%) | 349 (32) |
| Using insulin | 67 (6.1) |
| Dyspilidaemia, n (%) | 548 (50.2) |
| Smoking, n (%) | 380 (34.8) |
| Family history of CAD, n (%) | 280 (25.6) |
| Previous AMI, n (%) | 156 (14.3) |
| Previous PCI, n (%) | 125 (11.4) |
| Previous CABG, n (%) | 70 (6.4) |
| Chronic kidney disease, n (%) | 39 (3.6) |
| Clinical picture, n (%) | |
| Stable angina/silent ischaemia, n (%) | 305 (28) |
| Unstable angina/Non-ST-elevation myocardial infarction ST-elevation | 418 (38.3) |
| ST-elevation myocardial infarction | 367 (33.7) |
CAD=coronary artery disease; AMI=acute myocardial infarction; PCI=percutaneous coronary intervention; CABG=coronary artery bypass grafting.
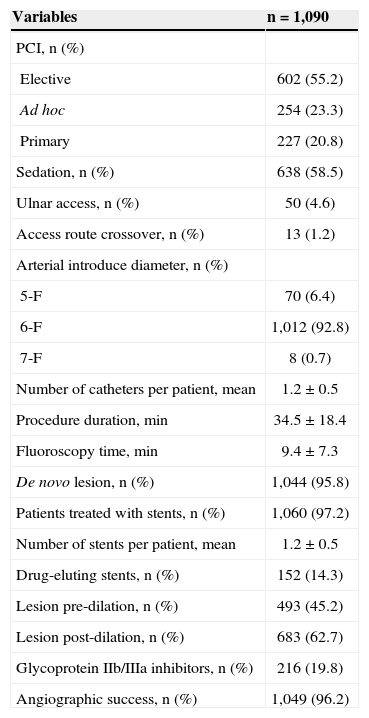
The characteristics of the procedures are indicated in Table 2. Elective PCI was performed in 55.2% of cases, ad hoc PCI in 23.3% and primary PCI in 20.8%. The rate of failure in obtaining radial and/or ulnar access or the need to change the access route for procedure completion was 1.2% (12 failures by the radial access and one by the ulnar). The most frequent causes of technique failure were right brachial artery occlusion after previous coronary angiography by Sones technique (five cases); inadequate support for the PCI (three cases); excessive tortuosity of the radial artery after its emergence from the brachial artery, preventing the progression of the guidewire and/or catheter (two cases); hypoplastic radial artery and/or spasm when attempting to perform puncture and cannulation (two cases); and failure to advance the sheath, most likely due to ulnar artery dissection by the guidewire (one case). The femoral artery was chosen as the alternative route in seven patients, the contralateral radial artery was chosen in five patients and the ipsilateral ulnar artery in one patient.
Characteristics of the procedures
| Variables | n=1,090 |
|---|---|
| PCI, n (%) | |
| Elective | 602 (55.2) |
| Ad hoc | 254 (23.3) |
| Primary | 227 (20.8) |
| Sedation, n (%) | 638 (58.5) |
| Ulnar access, n (%) | 50 (4.6) |
| Access route crossover, n (%) | 13 (1.2) |
| Arterial introduce diameter, n (%) | |
| 5-F | 70 (6.4) |
| 6-F | 1,012 (92.8) |
| 7-F | 8 (0.7) |
| Number of catheters per patient, mean | 1.2±0.5 |
| Procedure duration, min | 34.5±18.4 |
| Fluoroscopy time, min | 9.4±7.3 |
| De novo lesion, n (%) | 1,044 (95.8) |
| Patients treated with stents, n (%) | 1,060 (97.2) |
| Number of stents per patient, mean | 1.2±0.5 |
| Drug-eluting stents, n (%) | 152 (14.3) |
| Lesion pre-dilation, n (%) | 493 (45.2) |
| Lesion post-dilation, n (%) | 683 (62.7) |
| Glycoprotein IIb/IIIa inhibitors, n (%) | 216 (19.8) |
| Angiographic success, n (%) | 1,049 (96.2) |
PCI=percutaneous coronary intervention.
6-F sheaths were used in 92.8% of cases, with an average of 1.2±0.5 catheters per patient. The de novo lesions were treated in 95.8% of cases, and the number of stents used was 1.2±0.5 stents per patient. Drug-eluting stents were implanted in 14.3% of patients, and lesions were pre-and post-dilated in 45.2% and 62.7% of cases, respectively. Glycoprotein IIb/IIIa inhibitors were used in 19.8% of the procedures, representing two thirds of the cases with primary PCI. Sedation was used in more than half (58.5%) of the patients. Angiographic success was obtained in 96.2% of the PCIs.
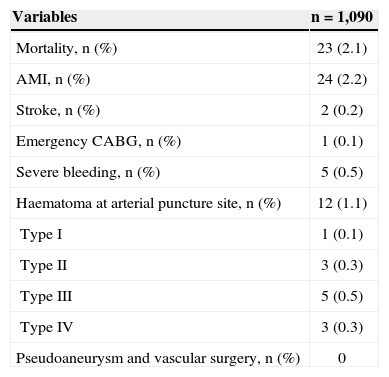
Table 3 illustrates the in-hospital outcomes of efficacy and safety. A severe bleeding episode was recorded in 5 (0.5%) patients, all classified as type 3 (3a in three patients and 3c in two patients). Hematomas were discovered in 1.1% of cases.
Efficacy and safety in-hospital outcomes
| Variables | n=1,090 |
|---|---|
| Mortality, n (%) | 23 (2.1) |
| AMI, n (%) | 24 (2.2) |
| Stroke, n (%) | 2 (0.2) |
| Emergency CABG, n (%) | 1 (0.1) |
| Severe bleeding, n (%) | 5 (0.5) |
| Haematoma at arterial puncture site, n (%) | 12 (1.1) |
| Type I | 1 (0.1) |
| Type II | 3 (0.3) |
| Type III | 5 (0.5) |
| Type IV | 3 (0.3) |
| Pseudoaneurysm and vascular surgery, n (%) | 0 |
AMI=acute myocardial infarction; CABG=coronary artery bypass grafting.
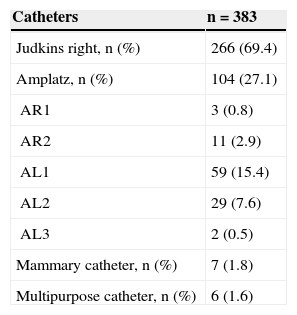
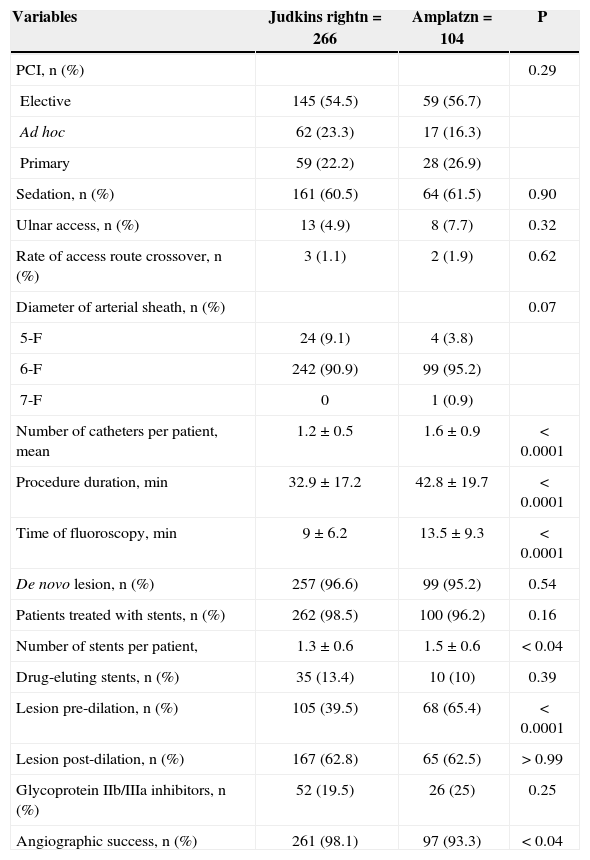
In PCIs to the left coronary artery, backup catheters were used in virtually all procedures (99.1%). JR catheters were used in 69.4% of cases in the treatment of the right coronary artery and Amplatz catheters in 27.1% (Table 4). The comparison between the groups treated with JR and Amplatz catheters indicated similar demographic characteristics, except for a higher prevalence of smoking (47.4% vs. 35.6%, P=0.04) in the group treated with the JR catheter and older age (60.6±10.7years vs. 64.1±10.7, P < 0.005), arterial hypertension (70.3% vs. 82.7%; P=0.01) and previous CABG (4.1% vs. 9.6%, P < 0.04) in the group treated with Amplatz catheters. The total duration of the procedure (32.9±17.2minutes vs. 42.8±19.7minutes, P < 0.0001), fluoroscopy time (9±6.2minutes vs. 13.5±9.3, P < 0.0001), number of catheters used (1.2±0.5 vs. 1.6±0.9; P < 0.0001), lesion pre-dilation (39.5% vs. 65.4%; P < 0.0001), and the number of stents per patient (1.3±0.6 vs. 1.5±0.6; P < 0.04) were higher in the group treated with Amplatz catheters. Angiographic success was greater (98.1% vs. 93.3%; P < 0.04) in the group treated with the JR catheter (Table 5). The rates of adverse cardiac events (4.6% vs. 2.7%; P=0.76) and severe bleeding (0.5% vs. 0.0%; P > 0.99) did not differ between the groups.
Characteristics of procedures according to the catheter used in right coronary artery treatment
| Variables | Judkins rightn=266 | Amplatzn=104 | P |
|---|---|---|---|
| PCI, n (%) | 0.29 | ||
| Elective | 145 (54.5) | 59 (56.7) | |
| Ad hoc | 62 (23.3) | 17 (16.3) | |
| Primary | 59 (22.2) | 28 (26.9) | |
| Sedation, n (%) | 161 (60.5) | 64 (61.5) | 0.90 |
| Ulnar access, n (%) | 13 (4.9) | 8 (7.7) | 0.32 |
| Rate of access route crossover, n (%) | 3 (1.1) | 2 (1.9) | 0.62 |
| Diameter of arterial sheath, n (%) | 0.07 | ||
| 5-F | 24 (9.1) | 4 (3.8) | |
| 6-F | 242 (90.9) | 99 (95.2) | |
| 7-F | 0 | 1 (0.9) | |
| Number of catheters per patient, mean | 1.2±0.5 | 1.6±0.9 | < 0.0001 |
| Procedure duration, min | 32.9±17.2 | 42.8±19.7 | < 0.0001 |
| Time of fluoroscopy, min | 9±6.2 | 13.5±9.3 | < 0.0001 |
| De novo lesion, n (%) | 257 (96.6) | 99 (95.2) | 0.54 |
| Patients treated with stents, n (%) | 262 (98.5) | 100 (96.2) | 0.16 |
| Number of stents per patient, | 1.3±0.6 | 1.5±0.6 | < 0.04 |
| Drug-eluting stents, n (%) | 35 (13.4) | 10 (10) | 0.39 |
| Lesion pre-dilation, n (%) | 105 (39.5) | 68 (65.4) | < 0.0001 |
| Lesion post-dilation, n (%) | 167 (62.8) | 65 (62.5) | > 0.99 |
| Glycoprotein IIb/IIIa inhibitors, n (%) | 52 (19.5) | 26 (25) | 0.25 |
| Angiographic success, n (%) | 261 (98.1) | 97 (93.3) | < 0.04 |
The current practice in a center that prioritizes the use of the radial (and ulnar) access when performing invasive coronary procedures is reported. The presence of acute coronary syndrome in the majority of the patients (72%), with some returning to their home hospitals after the procedure, was one of the major factors for the rapid adoption of this technique as the preferred treatment in the majority of cases. In this clinical group, there is a potential benefit by reducing ischemic outcomes due to the decreased occurrence of known determinants of poor prognosis: vascular complications at the arterial puncture site, episodes of severe bleeding, and need for transfusion. 3,15
The low rate of crossover and high success rate of the procedure demonstrated in the present study have a direct correlation with the frequency of the access use. Pristipino et al. 16 demonstrated in their Prospective REgistry of Vascular Access in Interventions in Lazio region (PREVAIL) an inverse correlation between the frequency of the use of radial access by the surgeon and the need for crossover of the access route. The correlation was as high as 33% among those who use radial access in at least 25% of the cases, decreasing to 3% among those whose percentage is higher than 85%.
The ulnar access is viable, safe, and effective in patients who cannot undergo the examination through the radial access, with success and complication rates related to the puncture site similar to those reported for the radial access. 17 This access has had increasing popularity, especially among the users of the transradial technique 18 (the so-called ‘radialists’ and ‘evangelists’). 19
Bertrand et al. 20 evaluated the contemporary use of the transradial practice by 1,107 interventional cardiologists from several centers around the world through an electronic questionnaire. The right radial access was used during 90% of procedures, and 25% of physicians reported not previously evaluating dual circulation of the hand. In cases where radial access failure occurred in centers that use this route during more than 50% of PCIs, 41% of physicians used the contralateral radial, and 47.1%, the femoral access. Sedation before the examination was used in 41.7%, and vasodilators were administered to more than 80% of cases. The use of the 6-F sheath was the standard, with a backup catheter used in more than 65% of the PCIs to the left coronary artery and the JR catheter in approximately 70% of PCIs to the right coronary artery. These results are consistent with those obtained in the present study, where backup catheters were used in almost all procedures to left coronary artery and JR catheters in approximately 70% of cases of PCI to right coronary artery. Over 90% of these cases, especially in primary PCIs, used 6-F sheaths, approximately 50% with direct stenting, a more liberal use of sedation (58.5%), and the use of glycoprotein IIb / IIIa inhibitors.
The sedative pharmacological solution used in this study combines the sleep-inducing and relaxing effects of midazolam with fentanyl analgesia, important factors in the prevention of radial spasm. The low use of 7-F catheters (< 1%) is noteworthy, even in the presence of bifurcation lesions, in which the provisional stenting technique is most commonly used in this hospital. This technique is easily performed with 6-F sheaths and lowprofile materials available in Brazil. Even when it is necessary to implant two stents, it is not necessary to change the catheter in most cases, when techniques such as T, TAP, or step crush are used.
The choice of guide catheters is one of the determinants of the successful implementation of training and learning programs for the transradial approach. Dedicated catheters are recommended, 21 although the utilization of catheters used during femoral route PCIs may facilitate the implementation and dissemination of the transradial approach without adding cost and time during the initial learning phase. Dedicated catheters can be used after the learning curve has been overcome.
Ikari et al. 22 evaluated the strength of support of guide catheters in simulations of femoral and radial PCIs to the left coronary artery in an arterial tree model. Three factors were associated with a greater support: the diameter of the catheter guide (the greatest diameter provided the greatest support); the angle (theta) of the catheter located on the opposite side of the aorta (one position lower than the catheter was preferable as the point of contact in the aorta, as the angle approached values close to 90 degrees, producing greater support); and the contact area with the aorta (the largest contact generated greater support to a limited extent). The study also demonstrated that, when using a left Judkins catheter, the support through the femoral access was 1.6 times greater when compared with the radial access. When the backup catheter was used, there was slightly greater support with the femoral approach (8%) with similar angles, but with a larger contact area compared with the radial access. There were no comparisons between the left Judkins catheters for femoral access and backup catheters through radial access; however, the maximum resistance values were very similar. In a later study conducted by the same group, 23 there was a comparison between the JR catheters and left Amplatz with PCIs to the right coronary catheter, indicating the superiority of the Amplatz in both radial and femoral approaches. This finding can be explained by a different mechanism from that regarding the use of catheters in the left coronary artery. The main factor that increased support to the guide catheter of the right coronary artery was the site of primary support of the catheter. For the right radial approach and the JR catheter, this site was the brachiocephalic trunk; for the left Amplatz catheter, this site was the reverse side of the aorta.
In the present study, the analysis of the subgroup submitted to PCI of the right coronary artery indicated patients with a higher-risk clinical profile, longer procedure and fluoroscopy times, higher number of catheters used, greater need for pre-dilation, increased number of stents per patient, and a lower angiographic success in patients who used the Amplatz catheter. This suggests that the choice of these catheters should be reserved for more complex cases, such as lesions that are more distal; the presence of tortuosity, calcification, and bifurcation lesions; and the presence of posterior and superior origins of the right coronary ostium.
LimitationsGiven that this study was observational, it has limitations, such as the nonrandomized nature of the subgroup analysis, its performance at only one centre, and the absence of late clinical follow up.
CONCLUSIONSThe use of radial access during PCIs produced a high success rate and a low incidence of major cardiac events and bleeding complications. The liberal use of sedation and 6F sheaths associated with the choice of catheters with higher support are operational characteristics of this centre, which prioritizes the use of the transradial approach.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.