Patients undergoing transradial procedures may experience pain associated with radial artery spasm. The pain can be assessed using the Visual Analogue Scale (VAS), an easy-to-apply, one-dimensional method. This study analyzed the perception of pain using the VAS and correlated it with the perception of spasm by the interventionist.
MethodsThis was an observational, prospective, single-center registry, which included patients undergoing diagnostic or therapeutic transradial procedures. The VAS consists of a 100-mm horizontal line, which has at its extremes the words “no pain” and “unbearable pain”. The patient was instructed to identify the point that represented the perceived pain during the procedure. The interventionist quantified the spasm as zero for no pain, 1 for pain with no resistance to catheter movement, 2 for mild resistance, 3 for moderate resistance, and 4 for intense resistance.
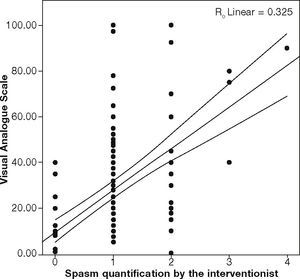
ResultsPain assessment by patients using the VAS was possible in all patients, and had a mean of 25.5 ± 25.7mm. For the interventionist, spasm was classified as grade zero in 53 cases (35.8%); grade 1 in 67 (45.3%); grade 2 in 24 (16.2%); grade 3 in 3 (2.0%); and grade 4 in 1 patient (0.7%). Kendall's tau-b and Spearman's (rho) rank correlation coefficients were, respectively, 0.527 and 0.647, showing a moderate positive correlation between the perception of pain by the patient and the perception of spasm by the operator.
ConclusionsVAS can be used to assess spasm during procedures that use the transradial access, showing a positive correlation with spasm assessment by the interventionist.
Pacientes submetidos a procedimentos por via transradial podem apresentar dor associada ao espasmo da artéria radial. A dor pode ser avaliada utilizando-se a Escala Visual Analógica (EVA), um método unidimensional de fácil aplicação. Analisamos a percepção de dor utilizando a EVA e a correlacionamos com a percepção de espasmo pelo operador.
MétodosRegistro observacional, prospectivo, unicêntrico, que incluiu pacientes submetidos a procedimentos diagnósticos ou terapêuticos por acesso transradial. A EVA é constituída por uma linha horizontal de 100mm, que traz nos extremos as inscrições “ausência de dor” e “dor insuportável”. O paciente foi instruído a marcar o ponto que representava a dor percebida no momento do procedimento. O operador quantificou o espasmo como zero se sem dor, 1 para dor sem resistência à movimentação dos cateteres, 2 para resistência leve, 3 para resistência moderada e 4 para resistência intensa.
ResultadosA avaliação de dor pelo paciente por meio da EVA foi possível em todos os pacientes, e teve média de 25,5 ± 25,7mm. Pelo operador, o espasmo foi classificado em grau zero em 53 casos (35,8%); grau 1 em 67 (45,3%); grau 2 em 24 (16,2%); grau 3 em 3 (2,0%); e grau 4 em 1 (0,7%). Os coeficientes de correlação tau b de Kendall e Ro de Spearman foram, respectivamente, de 0,527 e 0,647, mostrando correlação positiva moderada entre a percepção de dor pelo paciente e a percepção de espasmo pelo operador.
ConclusõesA EVA pode ser utilizada para a avaliação de espasmo durante os procedimentos que utilizem a via transradial, tendo demonstrado correlação positiva com a avaliação de espasmo pelo operador.
Transradial cardiac catheterization has attracted increasing interest and acceptance since its description by Campeau, in 1989,1 for diagnostic procedures, as well as by Kiemeneij and Laarman, in 1993,2 for therapeutic procedures.
Advances in the technique, with more experienced interventionists and improvement of materials and equipment, has contributed to the dissemination of the use of this vascular access, which has been increasingly employed in several centers.3,4
During the procedure, radial artery spasm, whose incidence varies between 3 and 22%, represents the main complication and a limitation to performing the transradial access catheterization. It can limit catheter manipulation, hindering the procedure, or even lead to changing access site. For the patient, it can result in severe pain, reducing comfort during the examination.5–7
When assessing radial artery spasm, the pain experienced by the patient is one of the criteria used.5 Pain is conceptually defined as an unpleasant sensory and emotional experience, associated with objective or potential damage. It has a subjective characteristic, and tools have been created to standardize the assessment and monitoring of the symptom. The tools can be classified as one-dimensional and multidimensional, according to the number of assessed characteristics. One-dimensional tools assess the intensity of pain and are useful for rapid assessment, ideal for acute cases.8,9
The Visual Analogue Scale (VAS) consists of a 100-mm horizontal line, which shows at its extremes the terms “no pain” and “unbearable pain”. The patient is instructed to mark on the line the point that represents the pain perceived during the procedure. The distance between the extreme “no pain” and the point marked by the patient determines pain intensity.8
The present analysis aimed to evaluate the perception of pain through a VAS, in patients undergoing diagnostic or therapeutic transradial cardiac catheterization, and to correlate it with the perception of spasm by the interventionist during the procedure.
MethodsStudy populationA prospective, observational, single-center registry was carried out, including 150 patients undergoing diagnostic and/or therapeutic transradial procedures. All interventionists had great experience with the transradial approach. Age older than 18 years; indication of cardiac percutaneous procedures, as determined by the attending physician; and the choice of transradial access by the interventional physician were considered inclusion criteria.
Patients undergoing primary angioplasty in acute myocardial infarction; requiring mechanical ventilation; with cardiorespiratory arrest, acute pulmonary edema, cardiogenic shock, or stroke during the procedure; and prior inclusion in this registry were considered exclusion criteria.
The study was approved by the Research Ethics Committee of the institution, through Plataforma Brasil, and all patients signed an informed consent form for the procedures.
ProceduresThe radial artery was punctured using a 20-22 G Jelco catheter or needle through the Seldinger or modified Seldinger technique, using a short hydrophilic sheath (10cm) (Radifocus™ Introducer II, Terumo, Tokyo, Japan). All patients received 5,000 IU of unfractionated heparin; the dose was complemented up to 100 IU/kg in cases of percutaneous coronary intervention. The use of medications to control the spasm was left to the discretion of the operator in charge of the procedure, as well as the choice of technique and catheters. At the end of the procedure, the sheath was immediately removed and hemostasis was carried out with a pressure dressing. Allen's test was not routinely performed.
At the end of the examination, the interventionist quantified the spasm according to the scale used in this service (zero for no pain or resistance to catheter movement; 1 for the presence of pain without resistance; 2 for mild resistance; 3 for moderate resistance, and 4 for intense resistance), and the patient was asked about the presence and quantification of pain in the upper limb through the VAS.
Statistical analysisContinuous variables were described as mean and standard deviation. Categorical variables were described as frequencies and percentages. Kendall's tau-b and Spearman's (rho) rank correlation coefficients were used to examine the relationship between the perception of pain by the patient and the perception of spasm by the operator. The alpha level of significance was 0.05, with a beta of 0.1. As there are no previous studies that evaluated the relationship between these variables, coefficient that was at least moderate (> 0.30) was considered to calculate the sample size, requiring a sample of at least 113 patients. Statistical calculations were performed and analyzed with the IBM software Statistical Package for Social Sciences (SPSS) 22.0.
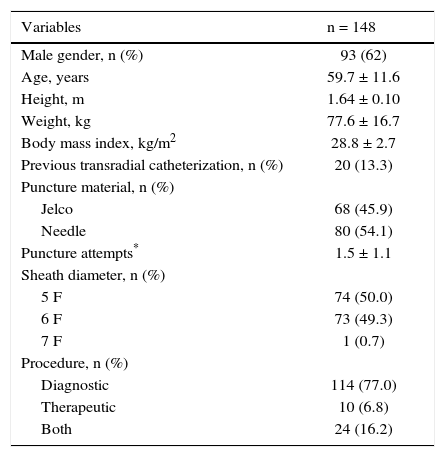
ResultsConsidering the 150 procedures included, radial puncture failure was observed in two (1.3%), and the access was changed to femoral. The radial artery puncture was successfully obtained in 148 patients (98.7%), with 107 (71.8%) at the first attempt. Clinical and procedural characteristics of the 148 patients included in the study are shown in Table 1. One (0.7%) procedure had the access changed due to the presence of spasm. Most procedures (74.4%) were performed without spasmolytic drugs, with isosorbide mononitrate being used, at a dose of 10mg, in 15.3% of the patients and nitroglycerin, at a dose of 200μg, in 10.3% of cases.
Baseline clinical and procedure characteristics.
| Variables | n = 148 |
|---|---|
| Male gender, n (%) | 93 (62) |
| Age, years | 59.7 ± 11.6 |
| Height, m | 1.64 ± 0.10 |
| Weight, kg | 77.6 ± 16.7 |
| Body mass index, kg/m2 | 28.8 ± 2.7 |
| Previous transradial catheterization, n (%) | 20 (13.3) |
| Puncture material, n (%) | |
| Jelco | 68 (45.9) |
| Needle | 80 (54.1) |
| Puncture attempts* | 1.5 ± 1.1 |
| Sheath diameter, n (%) | |
| 5 F | 74 (50.0) |
| 6 F | 73 (49.3) |
| 7 F | 1 (0.7) |
| Procedure, n (%) | |
| Diagnostic | 114 (77.0) |
| Therapeutic | 10 (6.8) |
| Both | 24 (16.2) |
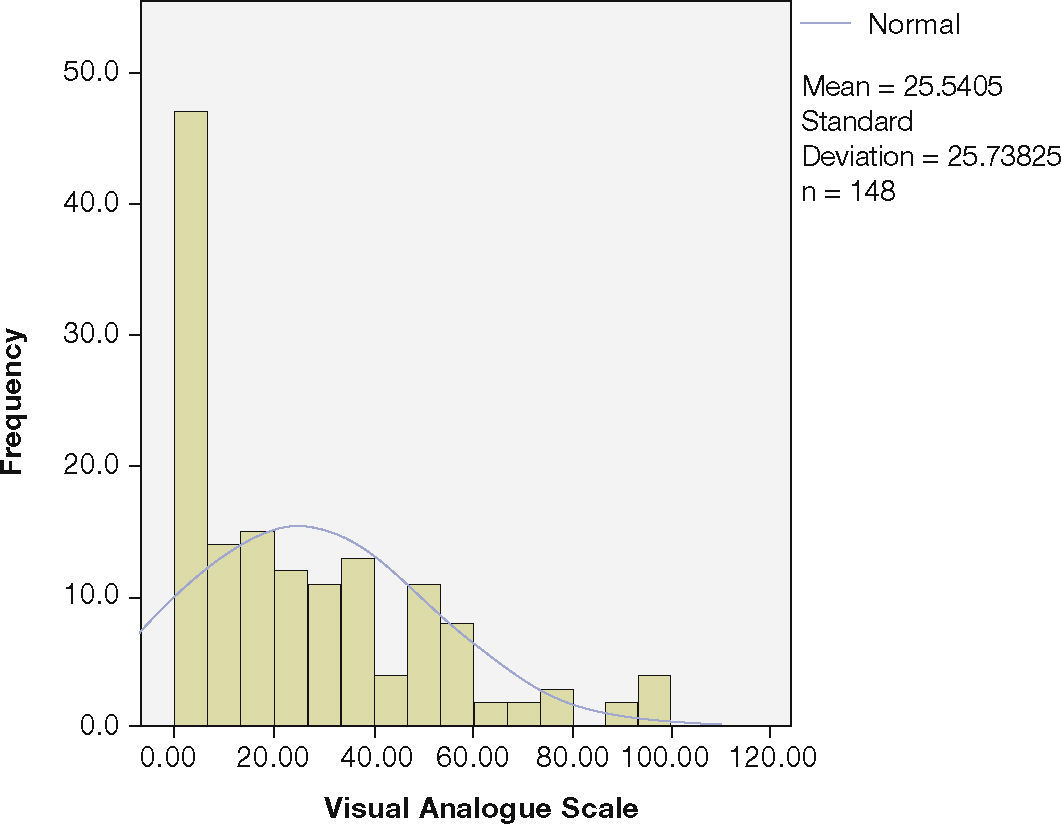
The classification of spasm by the interventionist was zero in 53 cases (35.8%); 1 in 67 cases (45.3%); 2 in 24 cases (16.2%); 3 in 3 cases (2.0%); and 4 in 1 case (0.7%). Pain assessment by the patient using the VAS was possible in all patients, and showed a mean of 25.5 ± 25.7mm, with a median of 20.00mm and interquartile range of 40.00mm. The distribution of pain assessment by the VAS is shown in Figure 1.
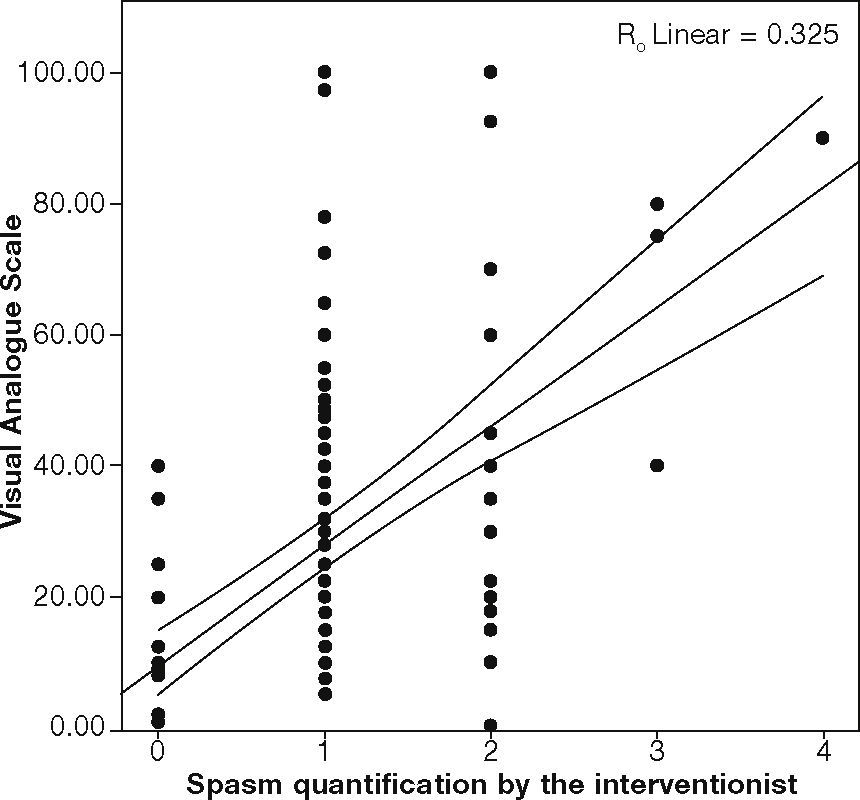
Kendall's tau-b and Spearman's rho correlation coefficients showed a moderate positive correlation between the VAS and spasm assessment by the interventionist. Kendall's tau-b was 0.527 and Spearman's rho was 0.647 (p < 0.05). The dispersion and linear regression of variables are shown in Figure 2.
DiscussionThe use of transradial access for diagnostic and therapeutic cardiovascular procedures has gained increasing popularity, mainly due to the lower rate of vascular complications and the increased comfort for patients.
The radial artery is a muscular artery whose tunica media consists almost exclusively of smooth muscle cells. There is a predominance of alpha-1-adrenergic receptors that respond with the contraction of muscle cells to catecholaminergic or mechanical stimulation.10 Thus, there is a risk of spasm during transradial interventions, leading to patient discomfort and difficulty in handling catheters and guidewires, therefore reducing the chance of procedural success.
Spasm evaluation is still performed using subjective criteria, which include mainly the interventionist's feeling of difficulty manipulating the catheter associated with the patient's feeling of pain, and there is no gold standard to evaluate it. To obtain an objective classification of spasm, the use of a device that performs the automatic withdrawal of the sheath at a constant speed and the associated record of the required force has been described. This method demonstrated a good correlation with clinical symptoms.11
During the procedure, pain is the indirect indication of spasm. Because pain is a subjective symptom with multiple dimensions that can not be objectively measured, the use of scales for one-dimensional assessment (pain intensity) has been proposed to standardize responses and allow correlations.
In the present study, the use of a pain assessment scale, the VAS, was possible in all 148 patients. This scale is considered a valid and reliable tool for acute and chronic pain measurements.9 Applying it for pain assessment during catheterization allows its use as a tool in studies comparing strategies that seek spasm reduction during transradial catheterization.
The correlation with the spasm assessment scale by the interventionist was positive and moderate. However, spasm assessment by the interventionist is subjective and susceptible to bias. Although used in several studies that evaluated spasm, there is no consensus classification to be applied. Thus, an easily reproducible method, such as the VAS, would show advantages in comparative assessments.
The main limitation of this study is the lack of an objective method for correlation with the VAS. The only objective method described to date is the automatic sheath removal system, which is not universally available and therefore is not routinely used in studies assessing spasm.
ConclusionsThe visual analogue scale was an easy-to-use, reliable, and reproducible tool, which could be used to evaluate spasm during percutaneous transradial access procedures. It also showed to be a less subjective tool in the evaluation of new strategies able to minimize radial spasm.
Funding sourceNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.