Despite the advent of drug-eluting stents (DES), diabetic patients still have increased risk of major adverse cardiovascular and cerebrovascular (MACCE) after percutaneous coronary intervention (PCI). Our aim was to evaluate the incidence of MACCE (death, stroke, non-fatal acute myocardial infarction, or target-lesion revascularization) during a follow-up of at least 1 year, in addition to the ability of the SYNTAX and residual SYNTAX scores to predict events.
MethodsSingle-center, retrospective study of diabetic patients with multivessel coronary disease, including left main coronary artery (LMCA) lesions treated with DES between 2012 and 2014.
ResultsA total of 158 patients were included, with a mean age of 65.1 ± 9.1 years. In 44.2% of the cases, there was a proximal lesion in the left anterior descending artery and 9% had a lesion in the LMCA. Most procedures were performed with second-generation DES (91.1%). Mean follow-up was 1,054 ± 725 days, and MACCE occurred in 17.4% of the patients. Among those with a low SYNTAX score (< 23), 10.2% had MACCE, while among those classified as having a moderate/high SYNTAX score (≥ 23), the incidence was 33.3% (p = 0.003). Of the patients with zero residual SYNTAX score (complete revascularization), 7.5% progressed with MACCE, compared with 22.0% with incomplete revascularization (p = 0.01).
ConclusionsThe present study points to the feasibility and safety of performing PCI in multivessel diabetic patients, especially among those with low angiographic complexity. Incomplete revascularization was a predictor of a higher occurrence of MACCE in the medium/long-term follow-up.
Apesar do advento dos stents farmacológicos (SF), diabéticos ainda experimentam risco aumentado de eventos cerebrovasculares e cardiovasculares maiores (ECCAM) após intervenção coronária percutânea (ICP). Nosso objetivo foi avaliar a incidência de ECCAM (óbito, acidente vascular cerebral, infarto agudo do miocárdio não fatal ou revascularização da lesão alvo) no seguimento de pelo menos 1 ano, além da capacidade de os escores SYNTAX e SYNTAX residual predizerem eventos.
MétodosEstudo unicêntrico, retrospectivo, de diabéticos com doença coronariana multiarterial, incluindo lesões de tronco de coronária esquerda (TCE), tratados com SF entre 2012 a 2014.
ResultadosForam incluídos 158 pacientes, com média de idades de 65,1 ± 9,1 anos. Em 44,2% dos casos, havia lesão proximal da artéria descendente anterior e 9% apresentavam lesão de TCE. A maioria dos procedimentos foi realizada com SF de segunda geração (91,1%). A média de seguimento foi de 1.054 ± 725 dias, e o ECCAM ocorreu em 17,4% dos pacientes. Entre aqueles com escore SYNTAX baixo (< 23), 10,2% apresentaram ECCAM, enquanto que entre os que foram categorizados como com SYNTAX moderado/alto (≥ 23), a incidência foi de 33,3% (p = 0,003). Dos pacientes com escore SYNTAX residual zero (revascularização completa), 7,5% evoluíram com ECCAM, comparados com 22,0% com revascularização incompleta (p = 0,01).
ConclusõesO presente estudo aponta para a factibilidade e a segurança da realização de ICP em diabéticos multiarteriais, especialmente entre aqueles com baixa complexidade angiográfica. A revascularização incompleta foi preditora da maior ocorrência de ECCAM no seguimento de médio/longo prazo.
The presence of diabetes mellitus increases by two to four times the risk of cardiovascular disease1 and worsens the prognosis of treated individuals,2,3 regardless of the type of coronary artery revascularization strategy adopted.
It is estimated that approximately 25% of patients treated with percutaneous coronary intervention (PCI) are diabetics.4 Even with the advent of drug-eluting stents (DES), which, compared to bare-metal stents, have greatly reduced restenosis rates,5–7 these individuals still have worse clinical outcomes, with higher rates of target-lesion reintervention, thrombosis, and acute myocardial infarction (MI) when compared with non-diabetic patients.8
Although some controlled clinical trials have demonstrated the superiority of second-generation DES over first-generation ones, especially regarding thrombosis reduction,9,10 it is still unclear whether this benefit extends to diabetic patients treated in daily clinical practice.
The present study aimed to evaluate the incidence of major adverse cardiovascular and cerebrovascular events (MACCE) in diabetic patients with multivessel coronary artery disease, including left main coronary artery (LMCA) lesion treated with percutaneous coronary intervention with DES implantation and clinically followed-up for a minimum period of 1 year. The ability of the SYNTAX and residual SYNTAX scores to predict events in this population was also analyzed.
MethodsStudy design and assessed populationThis was a single-center, observational, retrospective study that analyzed medical records and reviewed pre- and post-intervention coronary angiographies. The study included all patients diagnosed with diabetes according to the American Diabetes Association (ADA) diagnostic criteria,11 and significant coronary disease in at least two of the three major epicardial arteries, including LMCA lesions treated with PCI and DES implantation between January 2012 and August 2014. Patients treated in the acute phase of MI with ST-segment elevation (primary or rescue PCI) were excluded.
ProcedureAfter the diagnostic coronary angiography was performed, all cases were analyzed and discussed in a meeting by a team comprising interventional and clinical cardiologists. Low-complexity cases (SYNTAX < 23) with favorable anatomy were treated percutaneously. Cases of greater anatomical complexity were analyzed together with the team of cardiothoracic surgeons and physicians specialized in perioperative care, and the final proposal was decided after evaluation by the institution's Heart Team.
Coronary angioplasties were performed according to the current guidelines,12,13 and the final procedure strategy was left to the interventionist's discretion. The multivessel treatment through staged procedures was allowed and carried out in a maximum period of up to 60 days. Treatment was individualized, considering the risk/benefit ratio in terms of clinical stability, complexity, and severity of lesions, as well as ventricular dysfunction. The type of DES used was chosen by the interventionist according to the availability during the period of study enrollment.
The antithrombotic protocol consisted of the administration of two antiplatelet agents: acetylsalicylic acid and clopidogrel. Pretreatment with acetylsalicylic acid 200 to 500mg and clopidogrel 300mg was performed > 24hours prior to the intervention for elective cases or with 600mg of clopidogrel > 2hours prior to the procedure for acute coronary syndrome without ST-segment elevation. After the intervention, acetylsalicylic acid therapy was maintained indefinitely at a dose of 100mg daily, whereas clopidogrel was maintained for a 12-month period at a dose of 75mg daily. During the procedure, intravenous unfractionated heparin was administered (70 to 100 U/kg) to maintain an activated clotting time > 250seconds (or > 200seconds in case of glycoprotein IIb/IIIa inhibitor administration).
A 12-lead electrocardiogram was performed before and immediately after the intervention. Laboratory tests included creatine phosphokinase MB-isoenzyme pre-procedure, 18 to 24hours post-procedure, and daily, until hospital discharge.
This study was approved by the institution's Research Ethics Committee.
Objectives, definitions, and clinical follow-upThe primary objective of the study was to report the occurrence of MACCE in the late clinical follow-up (≥ 1 year) of multivessel diabetic patients treated with DES. This combined outcome included cardiac death, stroke, nonfatal MI, or ischemia-guided target-lesion revascularization.
As a secondary outcome, patient outcomes were compared according to baseline SYNTAX score, as well as according to the residual SYNTAX score.
As a rule, all deaths were considered cardiac, unless a non-cardiac cause could be clearly established by clinical and/or pathological study.
The diagnosis of periprocedural MI was based on elevated creatine phosphokinase MB isoenzyme > three times the upper limit of the normal range within 48hours of the procedure, and: (1) evidence of prolonged ischemia (> 20minutes), demonstrated by persistent chest pain; or (2) ischemic changes of the ST-segment or new pathological Q-wave in > two contiguous leads on the electrocardiogram; or (3) angiographic evidence of coronary flow limitation; or (4) imaging evidence of viable myocardial loss.
Nonfatal MI following hospital discharge was defined as an elevation in myocardial necrosis markers (mainly troponin) above the 99th percentile of the reference upper limit and at least one of the following parameters: (1) symptoms suggestive of myocardial ischemia; (2) development of new Q-waves on the electrocardiogram; (3) new or presumably new significant changes in the ST-segment, T-wave, or new left bundle-branch block; (4) evidence, on imaging exam, of loss of viable myocardium or a new segmental contractility alteration; (5) identification of intracoronary thrombus by angiography or at the necropsy.
Stent thromboses were defined according to the Academic Research Consortium (ARC)14 as definite, probable and possible. They were also classified according to temporal occurrence as acute phase (< 24hours of the procedure), subacute phase (between 24hours and 30 days), late phase (between 1 month and 12 months), and very late phase (> 12 months).
Hospital complications including no-reflow, retroperitoneal hematoma, pseudoaneurysm, acute renal failure (according to Risk, Injury, Failure, Loss, End-Stage - RIFLE),15 coronary perforation, and coronary dissection were also evaluated.
Patients were allocated according to the SYNTAX score into two groups, according to degree of angiographic complexity: group 1, defined as SYNTAX score < 23 (low complexity), and group 2, defined as SYNTAX score ≥ 23 (intermediate and high complexity).
Additionally, patients were also classified according to post-PCI outcome into two groups of residual SYNTAX score: residual SYNTAX score equal to zero (complete revascularization), and residual SYNTAX score > 0 (incomplete revascularization).16 Individuals who had undergone prior coronary artery bypass graft surgery were excluded from the analysis of the SYNTAX and residual SYNTAX scores, as these scores have not been validated in this population.
Clinical follow-up was carried out through scheduled medical consultations according to the predefined protocol of the Interventional Cardiology Service. The data were recorded in appropriate forms, developed for the study, and stored in electronic spreadsheets.
Statistical analysisThe categorical variables were shown as absolute and percentage numbers, and compared by Chi-squared test and, when indicated, by Fisher's exact test. Quantitative variables were shown as mean ± standard deviations and compared by the Student's t-test.
The occurrence of adverse events as a function of time was described using Kaplan-Meier curves, compared through the log-rank test. A value of p < 0.05 was considered significant. The statistical package used was the R program (The R Foundation for Statistical Computing, Vienna, Austria), version 3.1.1.
ResultsDuring the inclusion period, 158 diabetic patients with multivessel disease, including LMCA lesions, were treated with DES and met the criteria for inclusion in the study.
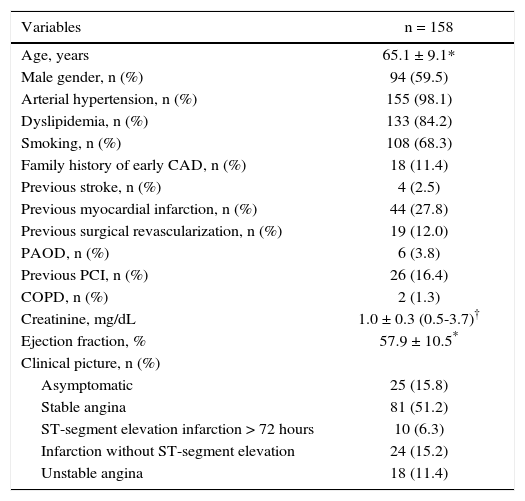
The mean age of the patients was 65.1 ± 9.1 years, of whom 59.5% were males and 28.5% used insulin. Regarding the initial clinical presentation, most patients (67.1%) were stable (asymptomatic patients with positive functional test or stable angina) and 12.0% had previously undergone coronary artery bypass graft surgery (Table 1).
Patients’ characteristics.
| Variables | n = 158 |
|---|---|
| Age, years | 65.1 ± 9.1* |
| Male gender, n (%) | 94 (59.5) |
| Arterial hypertension, n (%) | 155 (98.1) |
| Dyslipidemia, n (%) | 133 (84.2) |
| Smoking, n (%) | 108 (68.3) |
| Family history of early CAD, n (%) | 18 (11.4) |
| Previous stroke, n (%) | 4 (2.5) |
| Previous myocardial infarction, n (%) | 44 (27.8) |
| Previous surgical revascularization, n (%) | 19 (12.0) |
| PAOD, n (%) | 6 (3.8) |
| Previous PCI, n (%) | 26 (16.4) |
| COPD, n (%) | 2 (1.3) |
| Creatinine, mg/dL | 1.0 ± 0.3 (0.5-3.7)† |
| Ejection fraction, % | 57.9 ± 10.5* |
| Clinical picture, n (%) | |
| Asymptomatic | 25 (15.8) |
| Stable angina | 81 (51.2) |
| ST-segment elevation infarction > 72 hours | 10 (6.3) |
| Infarction without ST-segment elevation | 24 (15.2) |
| Unstable angina | 18 (11.4) |
* Standard deviation; † variation.
CAD: coronary artery disease; PAOD: peripheral arterial obstructive disease; PCI: percutaneous coronary intervention; COPD: chronic obstructive pulmonary disease.
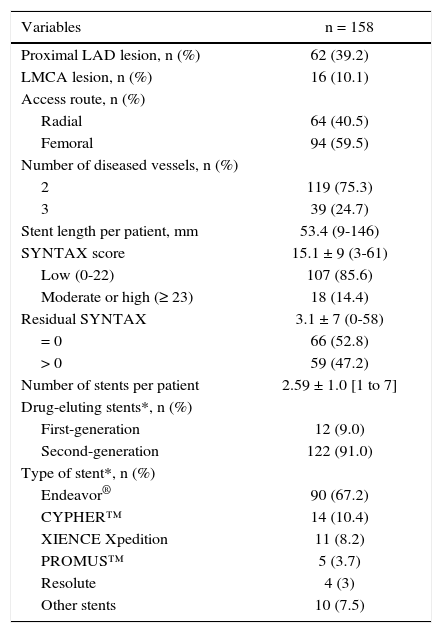
Regarding the angiographic characteristics (Table 2), 44.2% of the patients had a proximal lesion in the left anterior descending artery and 9% had an unprotected LMCA lesion. Most patients had two-vessel involvement (75.3%).
Angiographic and procedure characteristics.
| Variables | n = 158 |
|---|---|
| Proximal LAD lesion, n (%) | 62 (39.2) |
| LMCA lesion, n (%) | 16 (10.1) |
| Access route, n (%) | |
| Radial | 64 (40.5) |
| Femoral | 94 (59.5) |
| Number of diseased vessels, n (%) | |
| 2 | 119 (75.3) |
| 3 | 39 (24.7) |
| Stent length per patient, mm | 53.4 (9-146) |
| SYNTAX score | 15.1 ± 9 (3-61) |
| Low (0-22) | 107 (85.6) |
| Moderate or high (≥ 23) | 18 (14.4) |
| Residual SYNTAX | 3.1 ± 7 (0-58) |
| = 0 | 66 (52.8) |
| > 0 | 59 (47.2) |
| Number of stents per patient | 2.59 ± 1.0 [1 to 7] |
| Drug-eluting stents*, n (%) | |
| First-generation | 12 (9.0) |
| Second-generation | 122 (91.0) |
| Type of stent*, n (%) | |
| Endeavor® | 90 (67.2) |
| CYPHER™ | 14 (10.4) |
| XIENCE Xpedition | 11 (8.2) |
| PROMUS™ | 5 (3.7) |
| Resolute | 4 (3) |
| Other stents | 10 (7.5) |
*134 patients.
LAD: left anterior descending artery; LMCA: left main coronary artery.
A mean of 2.6 ± 1.0 stents was used per patient; most procedures were performed with second-generation DES (91.1%). The mean stent lenght per patient was 53.4mm, ranging from 9 to 146mm. Angiographic success rate was 98.7%, and clinical success was obtained in 94.3% of the population.
The SYNTAX and residual SYNTAX scores were evaluated in 125 (79.1%) study patients. The mean SYNTAX score was 14.2 ± 7.1, and most patients were classified as having low angiographic risk (85.6%). The post-intervention mean residual SYNTAX score was 2.1 ± 3.3. Most patients (52.8%) underwent complete anatomic revascularization (residual SYNTAX score equal to zero). Of the 107 patients with a low SYNTAX score, complete revascularization (residual SYNTAX score equal to zero) was observed in 63 (58.8%), while among higher-complexity patients (moderate/high SYNTAX score), 83.4% had incomplete revascularization.
There were one case of no-reflow (0.6%), one case of coronary dissection (0.6%), and two cases of renal failure after the intervention (1.3%). Seven patients (4.4%) suffered periprocedural MI and three (1.9%) developed femoral artery pseudoaneurysm. No retroperitoneal hematomas or coronary perforation were observed in this population.
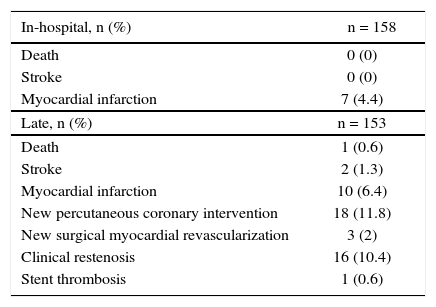
Table 3 presents the main adverse clinical outcomes at the in-hospital and late stages. Late clinical follow-up data was obtained for the entire population, with a mean of 1,054 ± 725 days.
Outcomes in the in-hospital and extra-hospital follow-up (non-cumulative).
| In-hospital, n (%) | n = 158 |
|---|---|
| Death | 0 (0) |
| Stroke | 0 (0) |
| Myocardial infarction | 7 (4.4) |
| Late, n (%) | n = 153 |
| Death | 1 (0.6) |
| Stroke | 2 (1.3) |
| Myocardial infarction | 10 (6.4) |
| New percutaneous coronary intervention | 18 (11.8) |
| New surgical myocardial revascularization | 3 (2) |
| Clinical restenosis | 16 (10.4) |
| Stent thrombosis | 1 (0.6) |
Most patients remained asymptomatic after PCI (77.8%). The overall MACCE rate in the long-term follow-up was 17.4%, with only one death (sudden death at 3 years and 6 days post-intervention). The occurrence of non-fatal MI was 6.4%, most of which without ST-segment elevation (5.9%), and the stroke rate was 1.3%. Clinical restenosis was observed in 10.4% of cases, and there only one only definite thrombosis (0.6%).
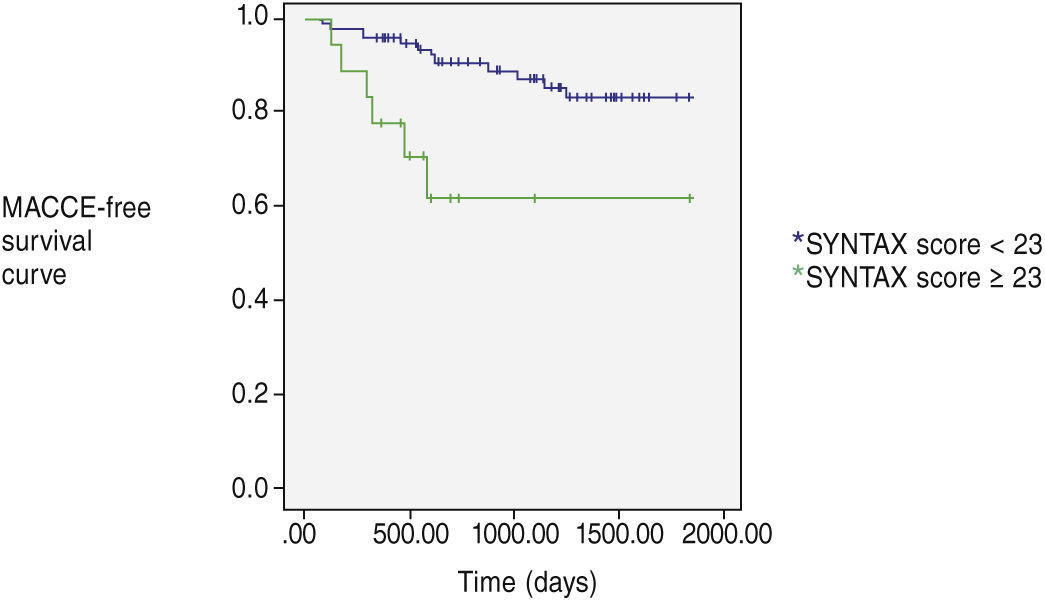
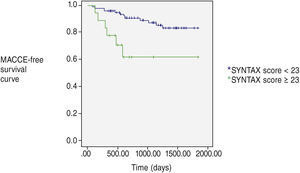
Figure 1 shows MACCE-free survival according to the baseline SYNTAX score. A more favorable evolution was observed among patients with low SYNTAX score. Among the 107 patients with a SYNTAX score < 23, 10.2% had MACCE, while among those with moderate/high angiographic complexity, 33.3% had MACCE in the late follow-up (p = 0.003).
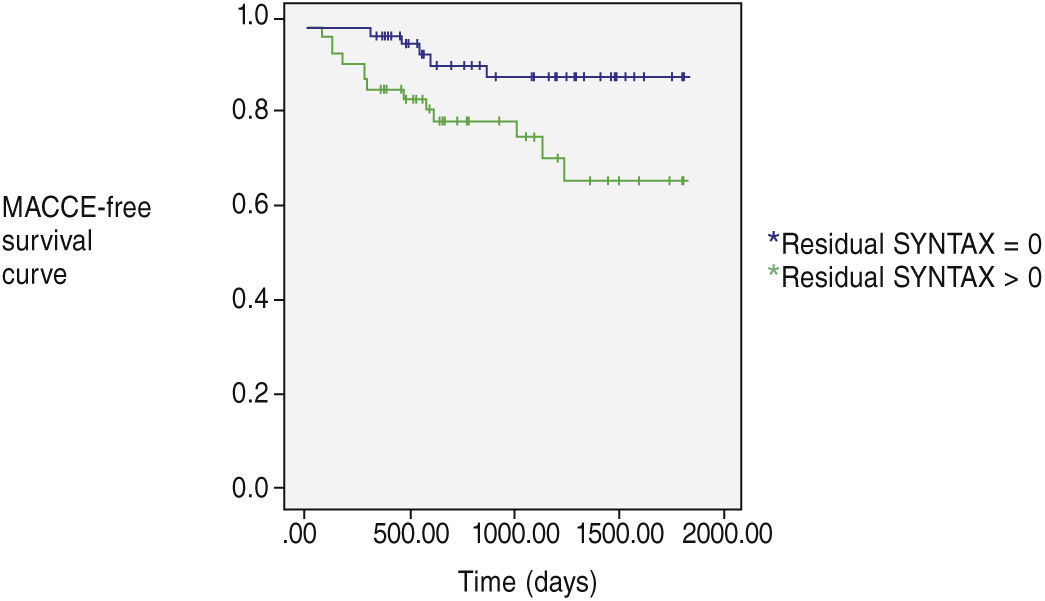
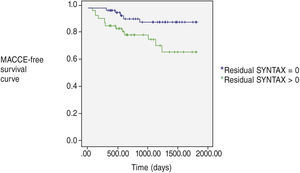
Similarly, there was a higher occurrence of MACCE during the evolution of patients who did not attain complete revascularization (Fig. 2). Of the 66 patients with a residual SYNTAX score equal to zero, 5 (7.5%) progressed with MACCE in the late follow-up, whereas among those with incomplete revascularization, the MACCE rate was significantly higher (22%; p = 0.01).
DiscussionThe present study indicates PCI with DES implantation as an alternative for revascularization in selected multivessel diabetic patients, with good clinical results in the medium-term follow-up. This study also reinforces the importance of the angiographic complexity and of the ability to attain complete revascularization in this population's outcome.
The indication of revascularization in patients with diabetes mellitus aims to reduce major cardiovascular events and/or improve quality of life.17 Most studies comparing percutaneous coronary intervention with coronary artery bypass graft surgery in patients with multivessel coronary disease have observed better outcomes in the surgical group. However, previous clinical trials were generally restricted to the use of first-generation DES.18 In contrast, in the present study second-generation DES were employed in almost all patients (91.1%).
The SYNTAX score is used to objectively extract information from the coronary angiography and determines the technical challenges to surgeons or interventionists for the used revascularization strategy. The follow-up analysis of the SYNTAX study (5 years) showed that patients (diabetics and non-diabetics) who underwent percutaneous coronary intervention with a low-complexity SYNTAX score showed non-inferior results in relation to coronary artery bypass graft surgery regarding cardiovascular outcomes.19 In the present study, patients with a low-complexity SYNTAX score had a lower rate of MACCE when compared to those with moderate and severe complexity, a statistically significant finding (p = 0.03), corroborating the findings of previous randomized trials.20
Complete coronary revascularization, although desirable, is not always feasible, especially in multivessel patients undergoing percutaneous coronary intervention.20 A previous analysis indicated that patients who attain complete revascularization have a better clinical evolution compared to those that do not.22 However, most registries that investigated the clinical impact of complete revascularization lack standardized definitions. In this context, the residual SYNTAX allows an objective quantitative evaluation of the revascularization extent in individuals treated with PCI. Additionally, the incremental value of residual SYNTAX on the predictive capacity of events makes the quantification of this score useful in the management of multivessel patients in daily practice.
When assessing the complete revascularization rate (zero residual SYNTAX score), only 16.6% of the group with greater angiographic complexity (SYNTAX ≥ 23) achieved this result, whereas in patients with lower angiographic complexity (SYNTAX < 23), this rate was 58.8%. Head et al.21 assessed the impact of revascularization on the 3-year results of the SYNTAX trial and demonstrated that incomplete revascularization occurred more frequently in patients with more complex coronary disease, corroborating the data of the present analysis.
In the present study, patients in whom PCI did not revascularize all lesions (residual SYNTAX > 0) had higher rates of adverse clinical events. It has been shown that the higher the residual SYNTAX, the greater the number of adverse clinical outcomes, including mortality.23 Residual SYNTAX is a new tool to quantify the extent and complexity of atherosclerosis after the treatment of coronary lesions, being a strong independent predictor of long-term adverse outcomes.12
LimitationsThis study has some limitations to be observed. First, it was a retrospective analysis. The number of patients included in the study is still relatively small for definitive conclusions. The rules of the Brazilian Unified Health System, which limit the number of stents used in the same patient, introduce a clear bias in the selection of patients referred to percutaneous treatment in this system. There is no systematic reimbursement for DES, so the treatment of patients with these devices was limited to their availability in the assessed period. Finally, this was the experience of a single center.
ConclusionsThe present study demonstrated the feasibility and safety of percutaneous coronary interventions in multivessel diabetic patients, especially among those with low angiographic complexity. Whenever possible, complete revascularization should be aimed; the degree of residual injury is a predictor of greater occurrence of adverse events in the medium/long-term follow-up.
Funding sourcesNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.