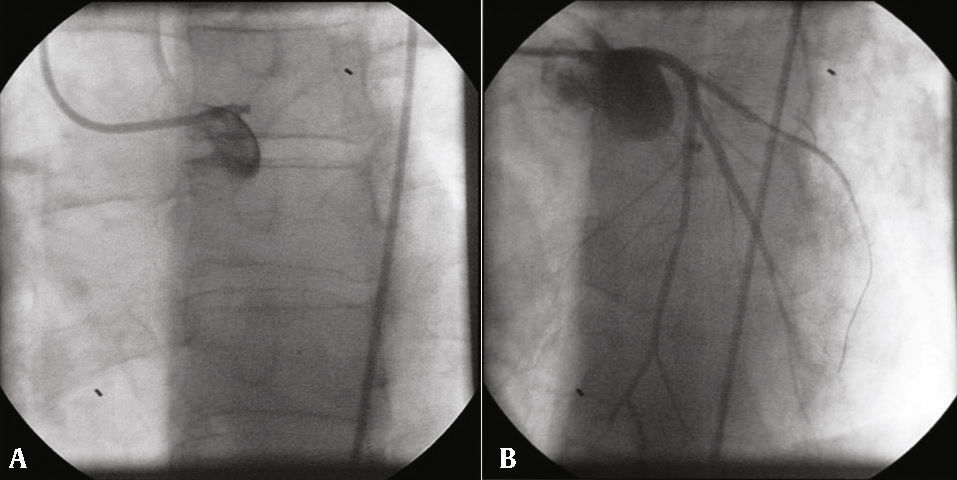
A 45-year old man with a previous history of active smoking and fibrillary astrocytoma (in remission) was admitted to the emergency department with upper abdominal pain and mild dyspnea lasting for 12hours. One year before he had been submitted to percutaneous coronary intervention (PCI) in the context of ST segment elevation myocardial infarction and received two drug eluting stents (DES), using a T-stenting technique, in left main coronary artery to the left anterior descending artery and the left main coronary artery to the left circumflex artery, with a good final result (Fig. 1). At admission he was under dual anti-platelet therapy, beta-blocker, angiotensin-converting enzyme inhibitor and statin.
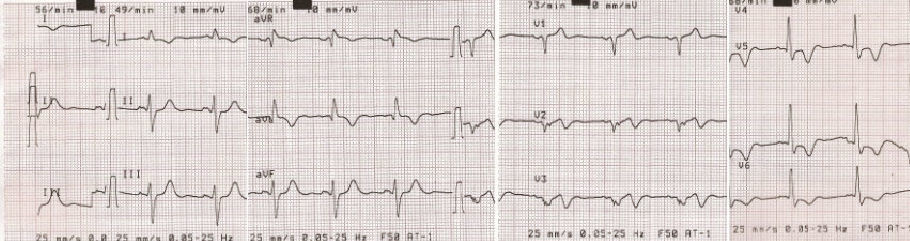
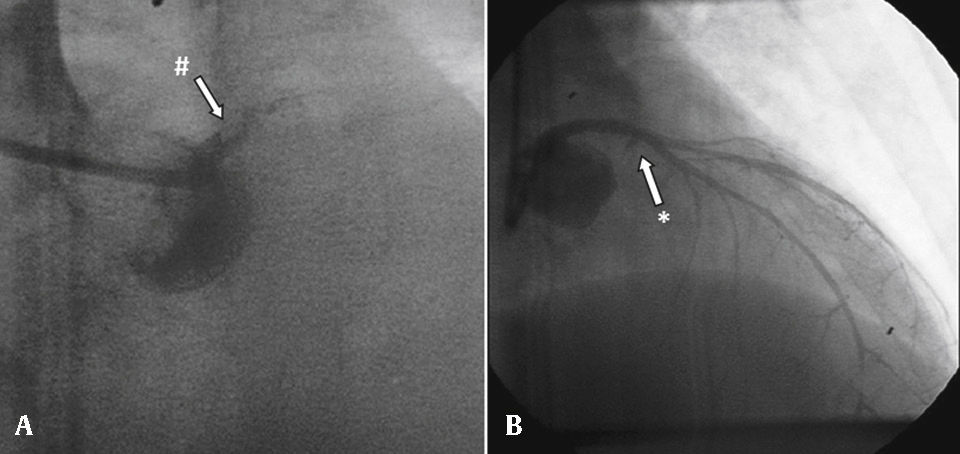
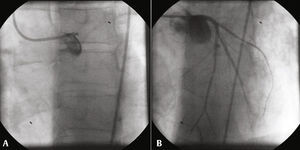
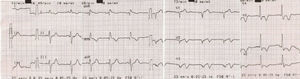
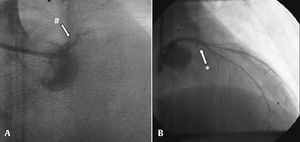
The 12-lead electrocardiogram (Fig. 2) presented Q waves in anteroseptal leads and negative T waves in I, aVL, V2-V6. He was sent to primary PCI, and the initial angiography showed thrombosis of both stents implanted in left main coronary artery (Fig. 3). Angioplasty was performed with implantation of a DES in left main coronary artery to left anterior descending artery, but the attempt to restore blood flow to left circumflex artery failed. Final result showed Thrombolysis in Myocardial Infarction (TIMI) 3 flow in left anterior descending artery and no flow in left circumflex artery (Fig. 3). Discharge electrocardiogram kept admission changes. Echocardiogram revealed severe left ventricular dysfunction. During in-hospital stay he had evolved into a Killip-Kimball class II and was discharged after 8 days. A cardioverter defibrillator was implanted 3 months later. At 3-year follow-up patient was clinically stable and event-free.
Percutaneous coronary intervention of the second event. (A) In-stent thrombosis (#) and occluded left main coronary artery; (B) result showing Thrombolysis in Myocardial Infarction (TIMI) 0 flow in left circumflex artery (*) and TIMI 3 flow in left anterior descending artery, with a distal left anterior descending artery lesion.
Left main coronary artery stent thrombosis is a rare event with most studies reporting rates < 2%. Factors that may have contributed to stent thrombosis are cessation of dual platelet therapy (denied by the patient) and stent malapposition. Use of coronary imaging techniques allow for a better assessment of the vessel size, adequate stent expansion, and absence of stent malapposition as well as improved outcomes. The new anti-platelet agents (prasugrel and ticagrelor) may contribute further to a reduction in stent thrombosis and overcoming clopidogrel resistance. Unprotected left main coronary artery bifurcation PCI is a challenging percutaneous procedure and there is no systematic data supporting a specific stenting technique, although it has been reported that a two-stent technique (excluding double kissing crush technique) may be associated with worse rate of stent thrombosis and major adverse cardiac events.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.