Many patients with coronavirus disease 2019 (COVID-19) have been diagnosed with computed tomography (CT). A prognostic tool based on CT findings could be useful for predicting death from COVID-19.
ObjectivesTo compare the chest CT findings of patients who survived COVID-19 versus those of patients who died of COVID-19 and to determine the usefulness the clinical usefulness of a CT scoring system for COVID-19.
MethodsWe included 124 patients with confirmed SARS-CoV-2 infections who were hospitalized between April 1, 2020 and July 25, 2020.
ResultsWhereas ground-glass opacities were the most common characteristic finding in survivors (75%), crazy paving was the most characteristic finding in non-survivors (65%). Atypical findings were present in 46% of patients. The chest CT score was directly proportional to mortality; a score ≥18 was the best cutoff for predicting death, yielding 70% sensitivity (95%CI: 47%–87%).
ConclusionsOur results suggest that atypical lesions are more prevalent in this cohort. The chest CT score had high sensitivity for predicting hospital mortality.
Muchos pacientes con enfermedad por coronavirus 2019 (COVID-19) han sido diagnosticados mediante tomografía computarizada (TC). Una herramienta de pronóstico obtenida de esta podría ser un predictor útil de mortalidad.
ObjetivosEvaluar los hallazgos de la TC de tórax entre los pacientes sobrevivientes y no sobrevivientes con COVID-19 y la utilidad clínica de una puntuación de TC.
MétodosDel 1 de abril al 25 de julio de 2020 se incluyeron 124 pacientes hospitalizados con infección confirmada por SARS-CoV-2.
ResultadosLas opacidades en vidrio deslustrado fueron el principal hallazgo típico en los sobrevivientes (75%), mientras que el patrón de pavimento loco fue el principal hallazgo típico en los no sobrevivientes (65%). Los hallazgos atípicos estuvieron presentes hasta en el 46% de los pacientes. Hubo una relación directamente proporcional entre la puntuación de la TC de tórax y la mortalidad, teniendo en cuenta un punto de corte óptimo de la puntuación de la TC de 18 para predecir la muerte con una sensibilidad del 70% [intervalo de confianza (IC) del 95%: 47%–87%].
ConclusionesNuestros datos sugieren una mayor prevalencia de lesiones atípicas en esta cohorte. La puntuación de la TC de tórax tuvo una alta sensibilidad para predecir la mortalidad hospitalaria.
The pandemic originated by SARS-CoV-2, which causes the coronavirus disease 2019 (COVID-19), has promoted research in early diagnostic and prognostic tools. A significant proportion of COVID-19 patients have been diagnosed through computed tomography (CT) with characteristic tomographic patterns changing and affected by severity and time of presentation of COVID-19.1,2 A recent comparative study reported a sensitivity of 98% in COVID-19 diagnosis with chest CT compared to 71% with reverse transcriptase-polymerase chain reaction (RT-PCR),1 although with lower specificity (37%) and negative predictive value (90%).2
It has been reported typical tomographic lesions for COVID-19, including ground-glass opacities (GGO) (97%), alveolar consolidations (30%–63%), linear/reticular opacities (65%), interlobular septal thickening (62%), and tomographic pattern in cobblestone “crazy paving” (70%–81%).3,4 The atypical or less frequent tomographic lesions reported in COVID-19 are diverse, such as the inverted halo sign, pulmonary nodules, cavitary lesions, pleural effusion, pleural thickening, mediastinal lymphadenopathy and bullous emphysema.3–6
Moreover, some of these findings are poor prognosis factors to the disease.3,5,6 This study focused on the imaging characteristics of COVID-19 patients, describing its broad spectrum of tomographic lesions and comparing the prevalence of typical and atypical lesions between the survivor and non-survivor patients. We also evaluated the clinical utility to predict in-hospital mortality of a chest CT score described and validated previously.7,8
MethodsDesign, setting and study populationThis was a single-center retrospective cohort study of COVID-19 consecutive adult patients hospitalized due to oxygen requirements in our center's general ward, between April 1, 2020, and July 25, 2020. This hospital was converted into a COVID-19 hospital, receiving suspected and confirmed COVID-19 cases. Wards redistribution due the pandemic was made, consisting of three isolated floors with 120 beds in the general ward. The hospital is in the Metropolitan area of Mexico City, the epicenter of the COVID-19 pandemic.
We included subjects who had available outcomes of this hospitalization and complete medical records. Data collection was made in worksheets accessing electronic health records from all patients. All patients that underwent CT-Scan were asked to sign informed consent to use the information for this study. The local ethical committee approved this retrospective study (number, R-2020-3501-158).
Chest CT evaluationAll chest CT scans were performed using a multi-detector GE Lightspeed 16 PRO Slice CT Scanner. Two senior radiologists with >6 years of experience evaluated the scanned images separately to identify each patient's chest CT characteristics; in case of disagreement, a consensus between them was made. Radiological terms were based on the standard glossary for thoracic imaging reported by the Fleischner Society.9 Typical lesions were GGO, linear/reticular opacities, interlobular septal thickening, alveolar consolidation and the “crazy paving” patterns. Atypical lesions were defined as pleural effusion, pneumatocele, mediastinal lymphadenopathy, tree-in-bud image, fibrotic steaks, cavitation and pleural thickening. Based on the CT score proposed by Pan et al.7 and validated by Francone et al.,8 we calculated a semi-quantitative CT severity score for each of the 5 lobes considering the extent of anatomic involvement; the score was calculated as follows: 0, no involvement; 1, <5%; 2, 5%–25%; 3, 26%–50%; 4, 51%–75%; and 5, >75% involvement. The resulting global CT score was the summation of each lobar score (0–25).
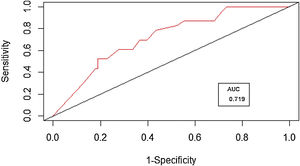
Statistical analysisCategorical variables were described as proportions, and continuous data were expressed as mean (with standard deviation) or median (with interquartile range). The χ2 test and Fisher exact test were used for comparisons of categorical variables as appropriate. Quantitative variables normally distributed were analyzed by Student's t-test; otherwise, Wilcoxon rank-sum test and Kruskal-Wallis rank-sum test were used. Sensitivity and specificity were calculated, and receiver operating characteristic (ROC) curve was used to determine the best cutoff value of the CT score. All the statistical analyses were performed using R software 3.6.3 (R-Foundation).
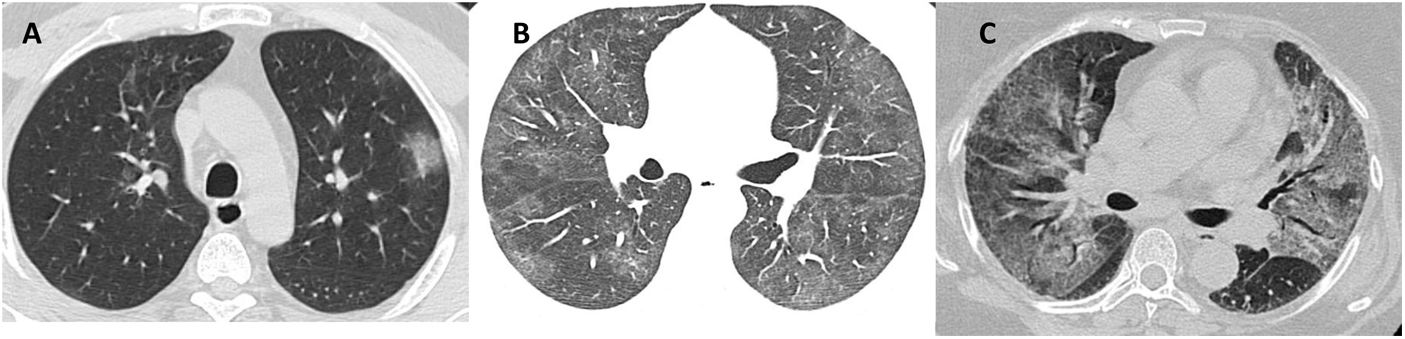
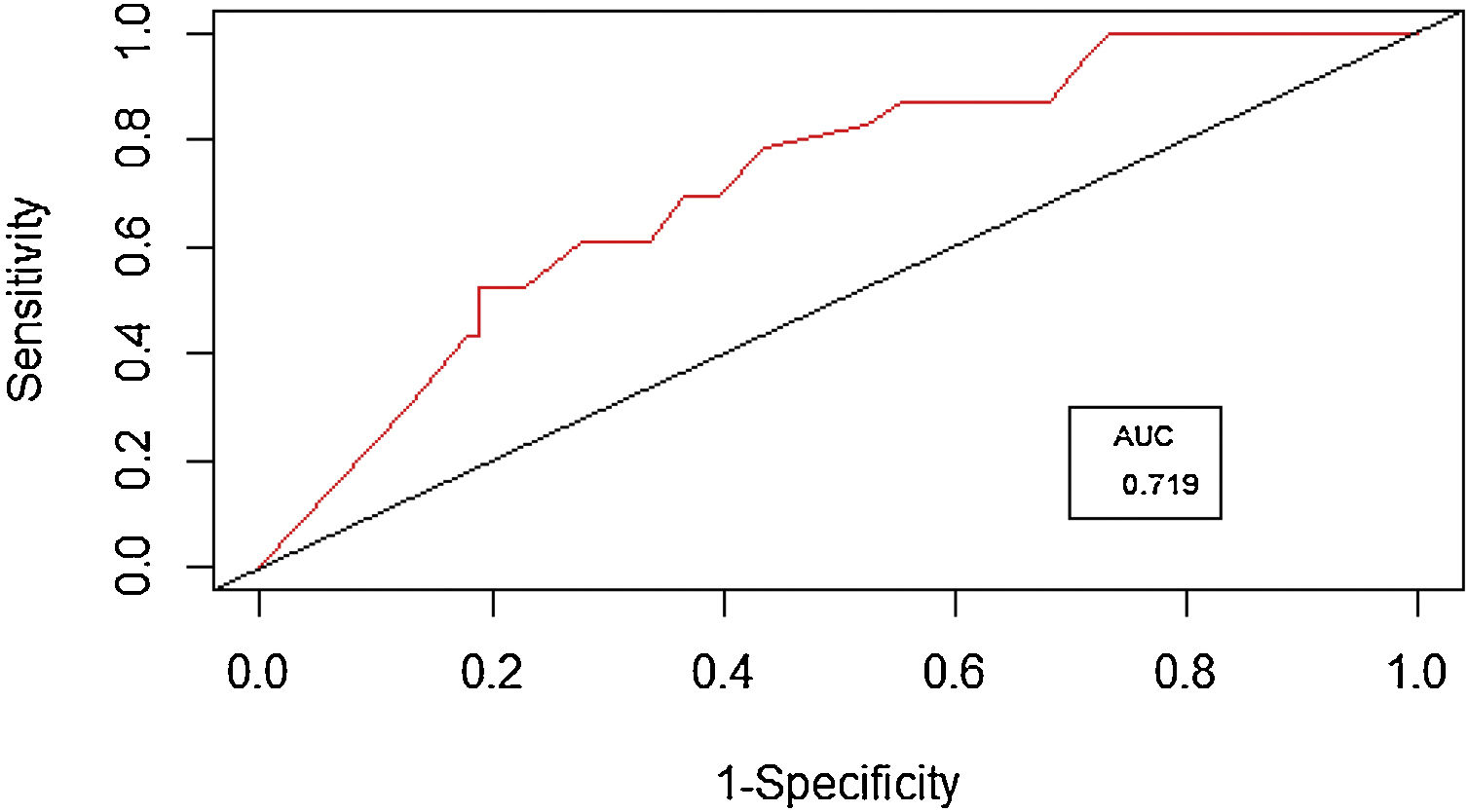
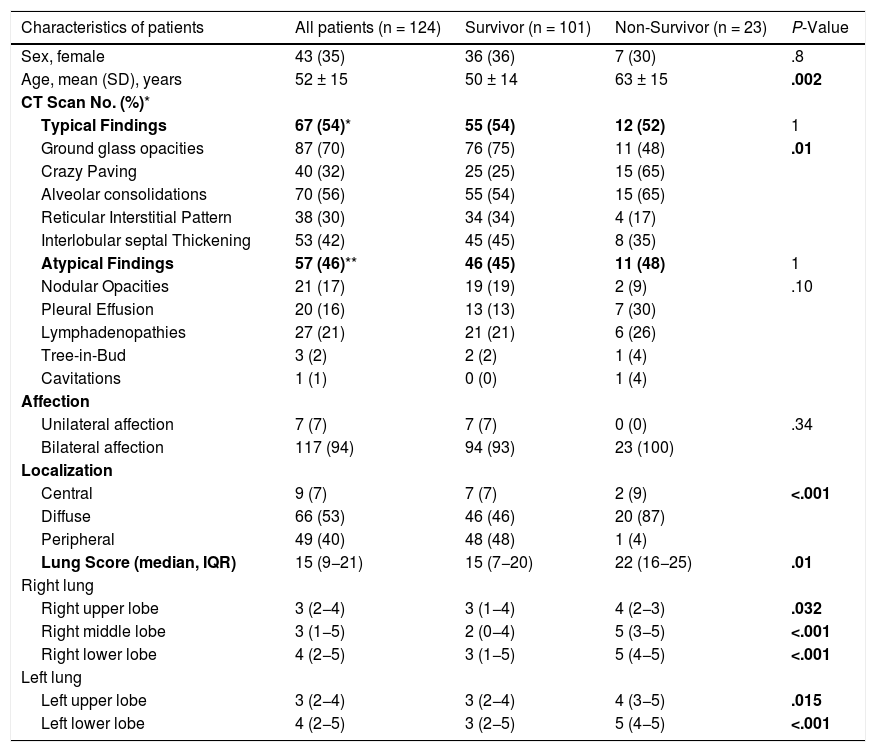
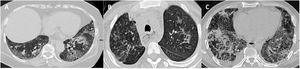
ResultsOverall, 130 patients were evaluated, of whom six were not included because of incomplete medical records. In the final analysis, we included one hundred twenty-fourth patients, the mean age of the overall population was 52 years (±15 years), and 65% (81/124) were male patients. There were 81% (101/124) survivors, and 19% (23/124) were non-survivor. The median time since onset of symptoms to chest CT was 10 days (IQR, 8–14). The survivor patients had a significantly lower mean of age (50 vs. 63 years). The number of male patients was higher in both the survivor (64%) and non-survivor patients (69%) without achieving statistical significance. In the overall population of the study, GGO were the main typical tomographic finding with 70%, and it was predominantly in the group of survivors (75%) followed by interlobular septal thickening (45%) and reticular interstitial pattern (34%) (Fig. 1). However, the crazy-paving pattern and consolidations had a significantly higher proportion (65%) in non-survivor patients (Table 1). Atypical CT lesions (Fig. 2) were present in up to 46%, with a higher proportion of pleural effusion (30%) and lymphadenopathies (26%) among non-survivor patients, although without achieve significance. In 94% of patients, the CT involvement was bilateral, and the predominant localizations were peripheral (40%) and diffuse (53%). The latter was the main finding in 87% (20/23) of non-survivor patients. The distribution of lung disease in the right lung had a higher percentage in the right lower lobe (RLL) (90%) than the right middle lobe (RML) (76%) and the right upper lobe (RUL) (87%). The involvement of the left lower lobe (LLL) (90%) was similar to the left upper lobe (LUL) (89%). The median CT score was 15 (interquartile range, 9−21) in the overall population. However, the median CT score was significantly higher in non-survivor than in survivor patients (22 vs. 15, P = .01); this difference remained in the comparisons among each lobe between survivor and non-survivor patients, as shown in Table 1. Interestingly, there was a significant difference among the median CT score of RLL (median, 4) in comparison with RML and RUL (both with a median of 3), P < .001. This difference was found between LLL and LUL (median, 4 vs. 3; P = .01). In the ROC analysis of the optimal CT score cutoff for prediction of death, we found that a score of 18 had the highest sensitivity (70%; 95% CI: 47%–87%) with a moderate specificity (64%; 95% CI: 54%–74%). The ROC area was 0.719 (95% CI: 0.612−0.824) (Fig. 3).
Chest CT Images of COVID-19 patients (A) A 40 years old man with a ground-glass opacity of peripheral distribution. (B) 57 years-old patient with a CT scan showing ground-glass opacities of bilateral distribution. (C) 67 years-old patient CT scan showing a crazy-paving pattern of central distribution.
Demographic data and chest computed tomography findings of patients with COVID-19.
| Characteristics of patients | All patients (n = 124) | Survivor (n = 101) | Non-Survivor (n = 23) | P-Value |
|---|---|---|---|---|
| Sex, female | 43 (35) | 36 (36) | 7 (30) | .8 |
| Age, mean (SD), years | 52 ± 15 | 50 ± 14 | 63 ± 15 | .002 |
| CT Scan No. (%)* | ||||
| Typical Findings | 67 (54)* | 55 (54) | 12 (52) | 1 |
| Ground glass opacities | 87 (70) | 76 (75) | 11 (48) | .01 |
| Crazy Paving | 40 (32) | 25 (25) | 15 (65) | |
| Alveolar consolidations | 70 (56) | 55 (54) | 15 (65) | |
| Reticular Interstitial Pattern | 38 (30) | 34 (34) | 4 (17) | |
| Interlobular septal Thickening | 53 (42) | 45 (45) | 8 (35) | |
| Atypical Findings | 57 (46)** | 46 (45) | 11 (48) | 1 |
| Nodular Opacities | 21 (17) | 19 (19) | 2 (9) | .10 |
| Pleural Effusion | 20 (16) | 13 (13) | 7 (30) | |
| Lymphadenopathies | 27 (21) | 21 (21) | 6 (26) | |
| Tree-in-Bud | 3 (2) | 2 (2) | 1 (4) | |
| Cavitations | 1 (1) | 0 (0) | 1 (4) | |
| Affection | ||||
| Unilateral affection | 7 (7) | 7 (7) | 0 (0) | .34 |
| Bilateral affection | 117 (94) | 94 (93) | 23 (100) | |
| Localization | ||||
| Central | 9 (7) | 7 (7) | 2 (9) | <.001 |
| Diffuse | 66 (53) | 46 (46) | 20 (87) | |
| Peripheral | 49 (40) | 48 (48) | 1 (4) | |
| Lung Score (median, IQR) | 15 (9−21) | 15 (7−20) | 22 (16−25) | .01 |
| Right lung | ||||
| Right upper lobe | 3 (2−4) | 3 (1−4) | 4 (2−3) | .032 |
| Right middle lobe | 3 (1−5) | 2 (0−4) | 5 (3−5) | <.001 |
| Right lower lobe | 4 (2−5) | 3 (1−5) | 5 (4−5) | <.001 |
| Left lung | ||||
| Left upper lobe | 3 (2−4) | 3 (2−4) | 4 (3−5) | .015 |
| Left lower lobe | 4 (2−5) | 3 (2−5) | 5 (4−5) | <.001 |
aPulmonary Nodules, Fibrotic lines and reverse halo were not presented as CT findings; SD, standard deviation; IQR, interquartile range.
Chest CT images of COVID-19 pneumonia patients. (A) 70-year-old female patient with traction bronchiectasis and peripheral emphysema observed in the left basal region, associated with a crazy-paving pattern and septal thickening. (B) 40 years-old female with multiple small nodules and a tree-in-bud pattern in the lower right lobe. (C) 57-years-old-male patient with septal thickening alternates with irregular consolidations of central and peripheral distribution and bilateral pleural effusion.
This study found typical lesions such as GGO, interlobular septal thickening and reticular interstitial pattern as the most commons. Crazy-paving and consolidations are the most frequent lesions in non-survival patients. There were a high proportion of atypical lesions such as lymphadenopathies and pleural effusion. The non-survivors patients had a higher proportion of tomographic lung involvement, bilateral, diffuse and multilobar. Among this group of patients, the overall semi-quantitative CT scores were higher than the survivor group. A CT scores ≥18 had the best sensitivity for the prediction of in-hospital mortality in COVID-19 pneumonia.
Since the first report of chest CT findings,10 the GGO in initial stages and consolidations later have been the hallmark of COVID-19 pneumonia, as shown in this study. However, with the worldwide increase in COVID-19 cases, there were several reports with additional findings such as intralobular septal thickening,11 linear/reticular opacities and crazy paving pattern3,4 thus becoming, typical lesions by expert consensus.12
Our study found a higher frequency of atypical lesions than other reports, where atypical lesions were reported in a proportion of 8.4%.3,4,11 It could be explained by the technical difficulty in their interpretation and the absence of intentional search. Among the atypical findings, we had a proportion as high as 27% of lymphadenopathy, which is a poor prognosis factor and is associated with higher mortality.3 However, in our study, this finding was similar between the survivor and non-survivor patients. Another remarkable finding was pleural effusion (16%), which had a higher proportion in non-survivor patients. A recent study reported a higher prevalence of pleural thickening and pleural effusions than the reported previously; in that study, the associated factors with these findings were heart failure, pulmonary embolism and co-infections.6 The presence of tree-in-bud lesions had a low prevalence (2%) in our report, and it was similar in both survivors and non-survivors. Patel et al.5 suggested this finding could be associated with immuno-thrombosis and pulmonary thrombotic angiopathy secondary to SARS-CoV-2, and this finding has been scarcely reported in recent literature reviews.11
There are no definitive prognostic biomarkers to identify patients requiring immediate medical attention and estimate their mortality risk. In this regard, the chest CT affection with the bilateral and diffuse disease was present in a higher proportion in the non-survivor group in our study. These findings have been reported in severe/critical patients resulting in higher mortality.3 Moreover, because of the high sensitivity of chest CT for COVID-19 pneumonia,1 a prognostic tool obtained from the initial CT is helpful; the CT score, which has been validated by Francone et al.,8 was a good predictor of mortality in our center, and a CT score ≥18 was strongly associated with in-hospital mortality.
This study has some limitations, such as its retrospective design and that the chest CT was performed by the physician's decision, based on the clinical requirement and the patient's status. Therefore, the heterogeneities of CT time unable us to make a longitudinal comparison between the groups. In the patients developing severe acute respiratory distress syndrome (ARDS), a CT was not obtained for most of them. Thus, there was no enough CT data in the course of ARDS.
ConclusionsIn conclusion, the most common CT typical manifestation were GGO, interlobular septal thickening, and reticular interstitial infiltrates. A higher proportion of a crazy-paving pattern with bilateral and diffuse distribution was present in the non-survivor group. The presence of a CT score ≥ 18 was associated with a predictive role of in-hospital mortality from this disease. The most common atypical lesions were lymphadenopathies and pleural effusion, whose importance in COVID-19 are to be determined. Finally, the CT in COVID-19 is a strong tool in the diagnosis and prognosis of this disease, and its usefulness would be improved with further research in this field.
Authorship1. Responsible for study integrity: BALL, RCC, AON.
2. Study conception: BALL, RCC, AON.
3. Study design: BALL.
4. Data acquisition: HHC, DCC, JGQM, EGV.
5. Data analysis and interpretation: BALL, RCC, HCC, EGV, AON.
6. Statistical processing: BALL, AON.
7. Literature search: HHC, DCC, JGQM, EGV.
8. Drafting of the manuscript: BALL, RCC, AON.
9. Critical review of the manuscript with intellectually significant contributions: HHC, DCC, JGQM, EGV.
10. Approval of the final version: RCC, HCC, AON, DCC, JGQM, EGV, BALL.
Conflict of interestsThe authors declare that they have no conflict of interests.
Please cite this article as: Collado-Chagoya R, Hernández-Chavero H, Ordinola Navarro A, Castillo-Castillo D, Quiroz-Meléndez JG, González-Veyrand E, et al. Hallazgos tomográficos entre sobrevivientes y no-sobrevivientes con COVID-19 y utilidad clínica de una puntuación de tomografía torácica. Radiología. 2022;64:11–16.