Initial COVID-19 reports described a variety of clinical presentations, but lower respiratory abnormalities are most common and chest CT findings differ between adult and pediatric patients. We aim to summarize early CT findings to inform healthcare providers on the frequency of COVID-19 manifestations specific to adult or pediatric patients, and to determine if the sensitivity of CT justifies its use in these populations.
MethodsPubMed was searched for the presence of the words “CT, imaging, COVID-19” in the title or abstract, and 17 large-scale PubMed and/or Scopus studies and case reports published between January 1, 2020 and April 15, 2020 were selected for data synthesis.
ResultsInitial CT scans identified ground-glass opacities and bilateral abnormalities as more frequent in adults (74%, n = 698, and 89%, n = 378, respectively) than children (60%, n = 25, and 37%, n = 46). At 14+ days, CT scans evidenced varied degrees of improvement in adults but no resolution until at least 26 days after the onset of flu-like symptoms. In pediatric patients, a third (n = 9) showed additional small nodular GGOs limited to a single lobe 3–5 days after an initial CT scan.
ConclusionEarly adult CT findings suggest the limited use of CT as a supplemental tool in diagnosing COVID-19 in symptomatic adult patients, with a particular focus on identifying right and left lower lobe abnormalities, GGOs, and interlobular septal thickening. Early pediatric CT findings suggest against the use of CT if RT-PCR is available given its significantly lower sensitivity in this population and radiation exposure.
Los informes iniciales de la COVID-19 describieron diversas presentaciones clínicas, pero las anomalías de las vías respiratorias bajas son las más frecuentes y los hallazgos de la tomografía computarizada (TC) de tórax difieren entre pacientes adultos y pediátricos. Nuestro objetivo es resumir los hallazgos tempranos de la TC para informar a los profesionales sanitarios sobre la frecuencia de manifestaciones específicas de la COVID-19 en los pacientes adultos o pediátricos, y determinar si la sensibilidad de la TC justifica su uso en estas poblaciones.
MétodosSe buscó en PubMed la presencia de las palabras “TC”, “técnicas de imagen”, “COVID-19” en el título o en el resumen y se seleccionaron para la síntesis de datos 17 estudios a gran escala de PubMed y/o Scopus y casos clínicos publicados entre el 1 de enero de 2020 y el 15 de abril de 2020.
ResultadosLas TC iniciales identificaron que las opacidades en vidrio esmerilado (OVE) y las anomalías bilaterales eran más frecuentes en los adultos (74%, n = 698 y 89%, n = 378, respectivamente) que en los niños (60%, n = 25 y 37%, n = 46). A partir de los 14 días, las TC evidenciaron diversos grados de mejoría en los adultos, pero no se observó resolución hasta al menos 26 días después del inicio de los síntomas seudogripales. En los pacientes pediátricos, un tercio (n = 9) mostró pequeñas OVE nodulares adicionales limitadas a un solo lóbulo 3–5 días después de una TC inicial.
ConclusiónLos primeros hallazgos de la TC en adultos sugieren el uso limitado de la TC como herramienta complementaria en el diagnóstico de la COVID-19 en pacientes adultos sintomáticos, con especial atención a la identificación de las anomalías de los lóbulos inferiores derecho e izquierdo, las OVE y el engrosamiento del tabique interlobulillar. Los primeros hallazgos de la TC pediátrica desaconsejan el uso de la TC si se dispone de RT-PCR, debido a su sensibilidad significativamente menor en esta población y a la exposición a radiación.
The novel coronavirus disease 2019 (COVID-19) is an infectious respiratory disease caused by SARS-CoV-2, a member of the coronavirus (CoV) family Coronaviridae.1 This family comprises enveloped viruses containing positive-sense single-stranded genomes up to 32 kB — some of the largest known RNA viral genomes.2 The initial cases of COVID-19 can be traced to the Huanan seafood market in Wuhan, China. Common clinical manifestations among the earliest infected patients included fever, cough, dyspnea, and sputum production. Because relatively few patients presented with gastrointestinal (including diarrhea and vomiting) or upper respiratory symptoms (including rhinorrhea, sore throat, and sneezing), SARS-CoV-2 is thought to primarily, though not exclusively, affect the lower respiratory tract.3 In addition, several studies have demonstrated the ability of asymptomatic individuals to transmit the virus.4,5 Death reports and meta-analyses tracking the novel coronavirus suggest that the most vulnerable populations are the elderly and immunocompromised.6 Patients with pre-existing comorbidities (e.g., cardiovascular disease, diabetes mellitus, chronic respiratory disease, and oncological disease) are also at higher risk of complications.7
While most symptomatic adults present with acute lower respiratory tract infection-like symptoms, the majority of symptomatic children with COVID-19 present more mildly, and a greater proportion of infected children may be asymptomatic.8 Interestingly, preliminary data indicate that despite having lower symptom severity than adults, children are equally likely to become infected with the SARS-CoV-2 virus.9 Most children tend to recover one to two weeks after the onset of disease, and few progress to a more severe stage of lower respiratory infection.10 Infants, however, have been observed battling rarer symptoms, such as bronchopneumonia, at an incidence similar to that of elderly and immunocompromised patients.11
Here, we scrutinize and compare radiologic profiles of pediatric (up to the age of 18) and adult patients (which we group with elderly, as there is insufficient data on elderly patients specifically to separate the categories) infected with SARS-CoV-2 before two (2) million worldwide cases. The aim of the present review is to characterize these distinct risk groups and provide summary-level information on early COVID-19 case data.
Material and methodsThe search strategy involved using the advanced search tool for global articles published on PubMed or Scopus between January 1, 2020, and April 15, 2020. Keywords such as “CT” and “COVID-19” were searched for in the title or abstract (95 total search results, using MeSH terms “radiology” OR “imaging” to filter out irrelevant studies). Of these, seventeen (17) original case series were selected for the present review: thirteen (13) studies included only adult patients; three (3) studies included only pediatric patients; and one (1) study included a mixture of adult and pediatric patients. Included studies presented appropriate patient cohorts (i.e., pediatric/adult COVID-19-confirmed cases for retrospective studies) and well documented clinical data (i.e., the time point the CT scans were taken relative to the onset of symptoms). Excluded studies were missing patient age data or did not provide new information (e.g., other reviews). Selection bias was mitigated through the use of a four-member search team (KL, MD, JW, and TH). Authors KL and MD conducted the literary search; authors JW and TH vetted methodological biases, based on study population size and clinical presentation.
ResultsChest CT at initial presentation in adult patients. Typical radiographic imaging of COVID-19 infection in adults reveals parenchymal damage characterized by ground-glass opacities (GGOs) and lung consolidation.12,13 Pulmonary CT scans taken at initial symptom presentation displayed pleural effusion, cavitation, pulmonary nodules, or lymphadenopathy in less than 10% of patients, and, given their rarity, whether these findings were due to COVID-19 is unknown.14 Xu et al. found that non-contrast enhanced CT imaging of SARS-CoV-2-infected adult patients revealed GGOs in 72% of patients (n = 90). More than half of these adult patients presented with multilobar involvement (59%), pleural thickening (56%), and/or linear opacification (61%).15 Another study found the right lower lung lobe was involved in 76% of the cases (n = 21).12 Wu et al. also reported the most commonly affected areas of the lung to be the right lower lobe, specifically the dorsal and posterior segments.16
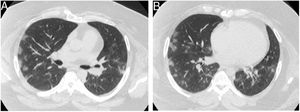
CT imaging suggests COVID-19 patients with severe pneumonia demonstrated GGOs and thickened intralobular septa more frequently than patients with mild pneumonia, as summarized in Table 1.17 In addition, CT abnormalities were variable in adult patients but commonly featured GGOs (Fig. 1) and consolidation (Table 2). In more advanced cases of COVID-19, crazy paving was also observed. Pure GGOs or GGOs with consolidation were consistently imaged in over 85% of diseased adults (n = 698) and, when reported, bilateral lung involvement was observed in 89% of patients (n = 378) (Table 2). Symptomatic patients demonstrated a significantly higher number of involved segments compared to asymptomatic patients, suggesting a correlation between lung involvement and disease severity.18 In total, 79% (64/81) of patients presented bilateral lung involvement, 54% (44/81) had peripheral distribution, and 44% (36/81) showed diffuse distribution of radiological abnormalities (n = 81). Consistent with previous findings, COVID-19 pneumonia typically presented as subpleural, bilateral GGOs with a modest predominance in the right lower lobe.19
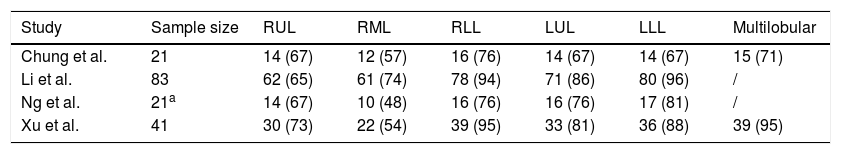
Lobar involvement in adult patients with COVID-19 pneumonia [n (%)].
| Study | Sample size | RUL | RML | RLL | LUL | LLL | Multilobular |
|---|---|---|---|---|---|---|---|
| Chung et al. | 21 | 14 (67) | 12 (57) | 16 (76) | 14 (67) | 14 (67) | 15 (71) |
| Li et al. | 83 | 62 (65) | 61 (74) | 78 (94) | 71 (86) | 80 (96) | / |
| Ng et al. | 21a | 14 (67) | 10 (48) | 16 (76) | 16 (76) | 17 (81) | / |
| Xu et al. | 41 | 30 (73) | 22 (54) | 39 (95) | 33 (81) | 36 (88) | 39 (95) |
RUL = right upper lobe, RML = right middle lobe, RLL = right lower lobe, LUL = left upper lobe, LLL = left lower lobe.
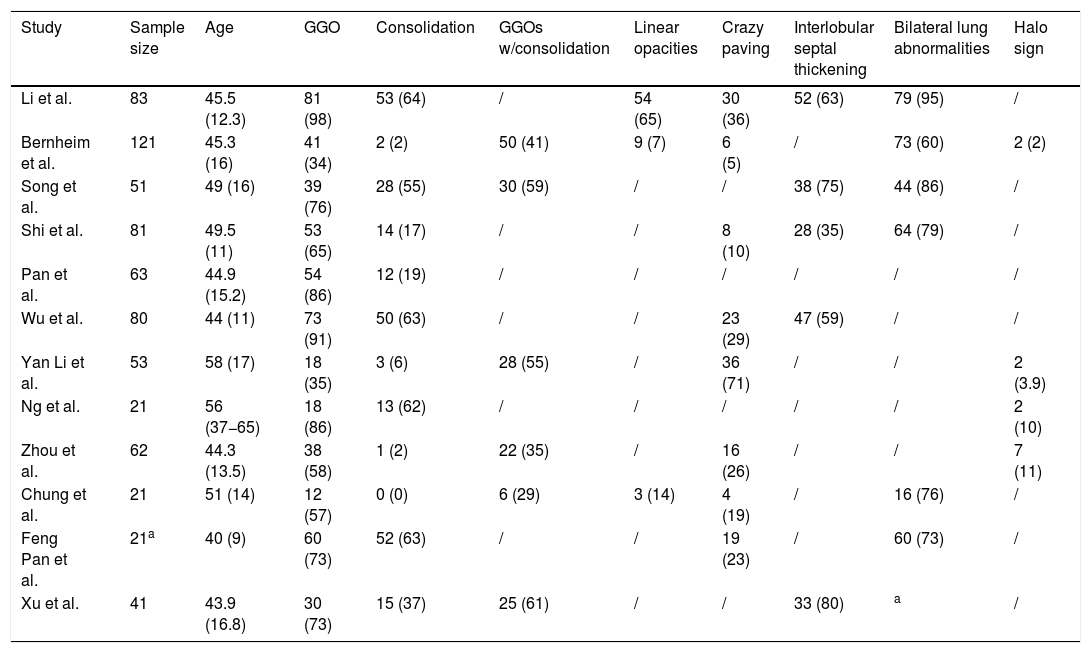
CT imaging features in adult patients with COVID-19 pneumonia [n (%)].
| Study | Sample size | Age | GGO | Consolidation | GGOs w/consolidation | Linear opacities | Crazy paving | Interlobular septal thickening | Bilateral lung abnormalities | Halo sign |
|---|---|---|---|---|---|---|---|---|---|---|
| Li et al. | 83 | 45.5 (12.3) | 81 (98) | 53 (64) | / | 54 (65) | 30 (36) | 52 (63) | 79 (95) | / |
| Bernheim et al. | 121 | 45.3 (16) | 41 (34) | 2 (2) | 50 (41) | 9 (7) | 6 (5) | / | 73 (60) | 2 (2) |
| Song et al. | 51 | 49 (16) | 39 (76) | 28 (55) | 30 (59) | / | / | 38 (75) | 44 (86) | / |
| Shi et al. | 81 | 49.5 (11) | 53 (65) | 14 (17) | / | / | 8 (10) | 28 (35) | 64 (79) | / |
| Pan et al. | 63 | 44.9 (15.2) | 54 (86) | 12 (19) | / | / | / | / | / | / |
| Wu et al. | 80 | 44 (11) | 73 (91) | 50 (63) | / | / | 23 (29) | 47 (59) | / | / |
| Yan Li et al. | 53 | 58 (17) | 18 (35) | 3 (6) | 28 (55) | / | 36 (71) | / | / | 2 (3.9) |
| Ng et al. | 21 | 56 (37−65) | 18 (86) | 13 (62) | / | / | / | / | / | 2 (10) |
| Zhou et al. | 62 | 44.3 (13.5) | 38 (58) | 1 (2) | 22 (35) | / | 16 (26) | / | / | 7 (11) |
| Chung et al. | 21 | 51 (14) | 12 (57) | 0 (0) | 6 (29) | 3 (14) | 4 (19) | / | 16 (76) | / |
| Feng Pan et al. | 21a | 40 (9) | 60 (73) | 52 (63) | / | / | 19 (23) | / | 60 (73) | / |
| Xu et al. | 41 | 43.9 (16.8) | 30 (73) | 15 (37) | 25 (61) | / | / | 33 (80) | a | / |
**Bilateral upper lobes involved in 27 (65.9%) patients. Bilateral lower lobes involved in 25 (61.0%) patients. Age provided as either mean (SD) or median (IQR).
Continuing, a 104-case study on the “Diamond Princess” cruise ship passengers observed that adult CT findings differed depending on if the patients were symptomatic or not. Symptomatic patients were more likely to show lung opacities (79%) and airway abnormalities (50%) than in asymptomatic patients (54% [p = 0.023] and 20% [p = 0.002], respectively). In contrast, asymptomatic patients more frequently showed GGOs over consolidation (83%), as opposed to consolidation over GGO, which was more frequently observed in symptomatic patients (41%, p = 0.038).20 Additionally, a retrospective study of 121 symptomatic adult COVID-19 patients and their chest CTs from four centers in China was reviewed. Bilateral and peripheral GGOs, as well as consolidative pulmonary opacities, were concluded to be the hallmarks of SARS-CoV-2 infection in this population.21 This study (n = 36) also found that 56% (95% CI: 47%–65%) of CT scans taken within 2 days of symptom onset were normal. In contrast, only one patient of those that received CT scans within 2 days had a negative result from an initial RT-PCR test.21 This points to the limited sensitivity of CT, especially compared to RT-PCR, in patients shortly after symptom onset and suggests CT would not make for a reliable standalone diagnostic test for COVID-19. In agreement with this sentiment, the “Diamond Princess” study found CT scans were normal in 46% (35/76) of asymptomatic patients and 21% (6/28) of symptomatic patients (p = 0.023).20
Chest CT at initial presentation in pediatric patients. Currently, pediatric COVID-19 is diagnosed via homologous viral genetic sequencing of respiratory or blood samples, or positive SARS-CoV-2 nucleic acid test results.22 Clinical presentation of COVID-19 infection in pediatric patients varies greatly but commonly includes fever, dyspnea, or dry cough; severe infection potentiates bronchopneumonia, a deadly pneumonia subtype which primarily afflicts infants. CT imaging of bronchopneumonia shows thickened lung texture and dense, patchy shadows of uneven density and fuzzy margin in the middle and lower lung fields of both lungs.11
In a small cohort of children diagnosed with COVID-19, Li et al. established the presence of modest patchy GGOs in three out of the five children evaluated, while the other two were asymptomatic and displayed no CT abnormalities (Table 3).6 In another study, Ji et al. examined two confirmed cases of pediatric COVID-19 wherein each child came from a separate family cluster. Both children had spent time in the Hubei Province, but one presented with upper respiratory symptoms whereas the other had diarrhea.23 Interestingly, their corresponding radiologic profiles differed too: chest CT imaging revealed GGOs in the former and severe pneumonia in the latter.23–25 However, pediatric patients may be asymptomatic or show mild symptoms even with CT abnormalities.26 Dong et al. reported that of the asymptomatic children tested for COVID-19, 13% were infected (n = 94).22 Other studies suggest that the vast majority of infected children are asymptomatic or have only mild symptoms.3,10,24
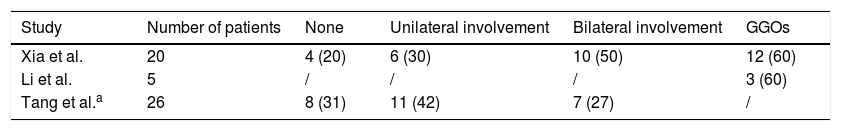
CT imaging features in pediatric patients with COVID-19 pneumonia [n (%)].
| Study | Number of patients | None | Unilateral involvement | Bilateral involvement | GGOs |
|---|---|---|---|---|---|
| Xia et al. | 20 | 4 (20) | 6 (30) | 10 (50) | 12 (60) |
| Li et al. | 5 | / | / | / | 3 (60) |
| Tang et al.a | 26 | 8 (31) | 11 (42) | 7 (27) | / |
Moreover, there exists a dissonance between symptom presentation and chest CT findings in pediatric cases thus far. For example, the first pediatric case in South Korea showed patchy consolidations with peripheral GGOs in the right lower lobe despite showing only mild symptom.27 In a recent study by Feng et al., ten of the 15 children with confirmed COVID-19 were asymptomatic while the remaining five presented with a fever. Pulmonary lesions were found on chest CT for nine of the patients, with small nodular GGOs being the most common finding.26 Fortunately, pediatric mortality is rare; out of 731 confirmed COVID-19 pediatric cases, the sole death was a 14-year-old boy from the Hubei province.22
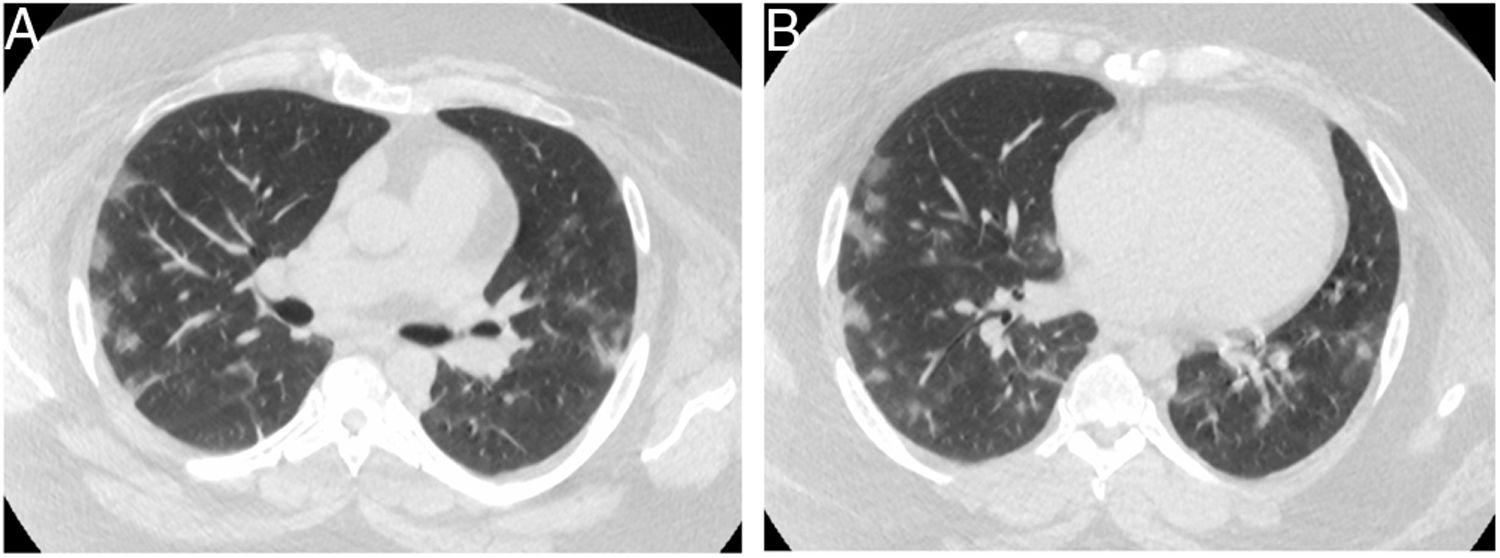
CT-identified COVID-19 progression in adult patients. One study delineated five distinct stages of COVID-19 disease progression on CT: “ultra early”, “early”, “rapid progression”, “consolidation”, and “dissipation”.28 The ultra early stage refers to lack of symptomatic clinical presentation but with imaging abnormalities including scattered focal ground-glass, patchy consolidation, and signs of intra-bronchial air-bronchogram. The early stage includes the 1–3 days after clinical manifestations are observed. CT imaging reveals single or multiple scattered patchy or agglomerated GGOs that are separated by grid-like thickening of interlobular septa.28 Most identified GGOs are peripheral focal or multifocal and affect both lungs (Fig. 2).29
The initial CT (A) obtained shows multiple ground-glass opacities in the posterior right upper lobe and left superior lobe. The follow-up CT scan (B) 3 days later shows that the GGO expanded in the posterior right upper lobe and left superior lobe. Reprinted with permission from Ref.29 Lei J, Li J, Li X, Qi X. CT Imaging of the 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology. 2020;295(1):18.
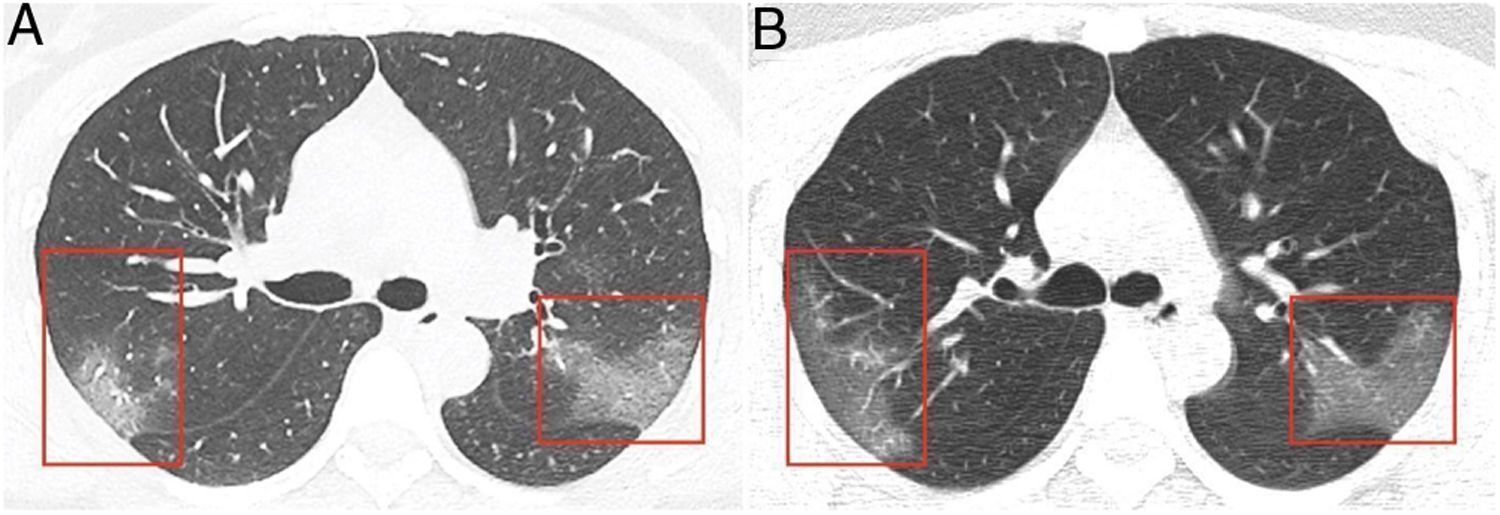
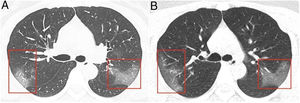
Over the week following initial onset of fever or dry cough, patients may exhibit rapid disease progression and corresponding clinical decline. Exacerbation of alveolar and interstitial edema leads to large-scale light consolidation with air-bronchogram. Crazy paving pattern also becomes a dominant CT manifestation.30 These crazy paving CT findings were observed in 19% (n = 36) of patients, as well as bilateral lung involvement in 86% (n = 36) of patients, 9–13 days post-onset of flu-like symptoms. The consolidation stage, characterized by multiple patchy and large lung consolidation, was observed 7–14 days after onset of symptoms. The dissipation stage was evidenced by fewer scattered patchy consolidations and lesion reduction (Fig. 3).28 At 14+ days, CT scans showed varied degrees of improvement in adults with no resolution until at least 26 days after the onset of flu-like symptoms. In addition, Chen et al. analyzed radiologic differences in disease progression after a median of 7 days following symptom onset and observed patients with worsening of original lesions both with and without the development of new lesions (n = 163).31 Across three independent studies, researchers have identified five unique cases of individuals testing positive for SARS-CoV-2 within a range of 3–13 days after their discharge.12,32,33
The initial scan (A) shows thickening of interlobular septa and patchy GGO in the tongue-like segment of the left upper lobe, along with patchy consolidation in the posterior segment of the right middle and lower lobes. The follow-up scan (B) taken 9 days after admission shows a reduction of lesions in the middle lobe, the right lower lobe, and the left upper lobe. Reprinted with permission from Ref.28 Jin Y-H, Cai L, Cheng Z-S, Cheng H, Deng T, Fan Y-P, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Military Medical Research. 2020;7(1).
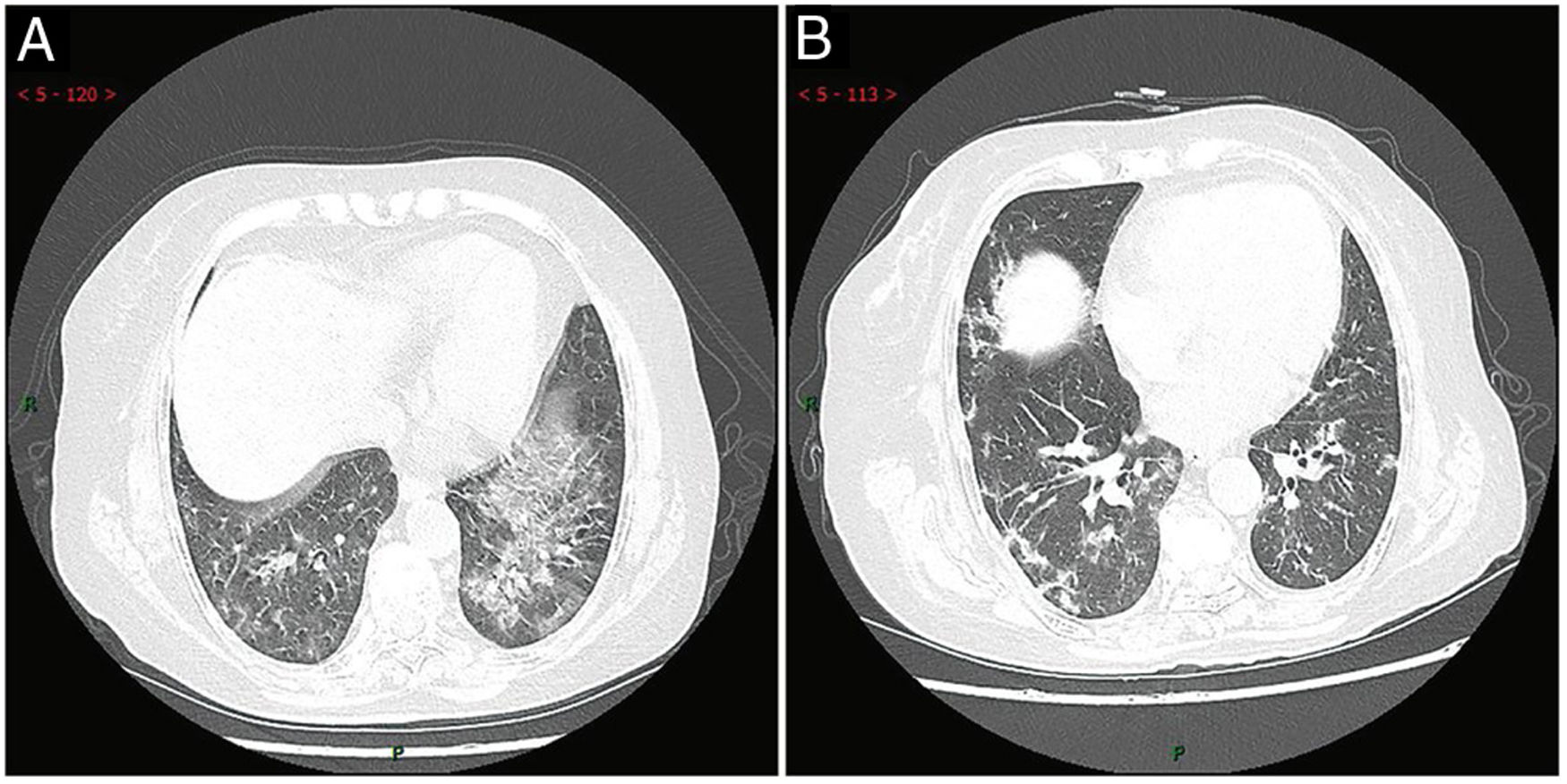
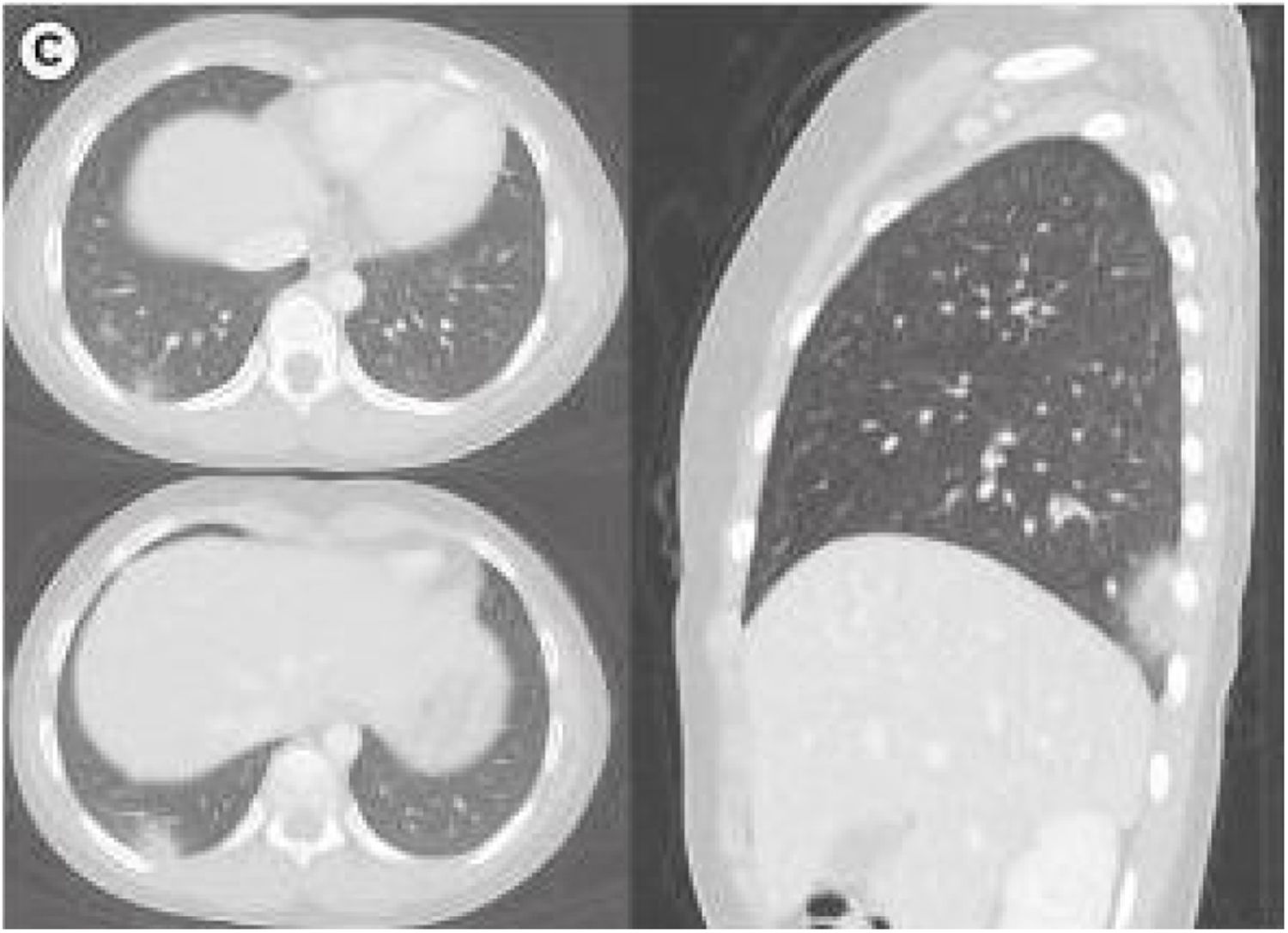
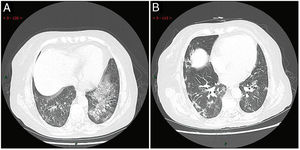
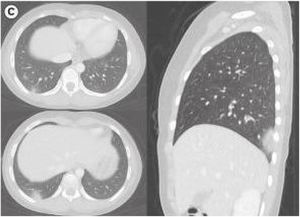
CT-identified COVID-19 progression in pediatric patients. A recent study by Feng et al. examined 15 children aged 4–14 years who were virologically confirmed to be infected with the novel coronavirus.26 Initial chest CT revealed no abnormal findings in six of the patients. The most common finding in the other nine patients were small nodular GGOs. Lesions were limited to less than two segments in 89% (8/9) of cases. Most of the lesions were sub-pleural with halo signs seen on some edges. The less common findings were speckled GGOs and patchy shadows. After 3–5 days of treatment, three of the nine cases that still tested positive for COVID-19 showed new lesions on chest CT, all of which were small nodular GGOs. All lesions were limited to a single lobe and were noticed in different areas compared to original lesions. The other six children exhibited similar chest inflammation compared to their initial CT scans.26 The lack of changes in progressive CT imaging amongst the pediatric population may be related to their relatively mild symptoms. Fig. 4 shows patchy nodular consolidations and peripheral GGOs in subpleural regions of the right lower lobe of a 10-year-old girl.34
Chest CT imaging in a 10 y/o female on the fourth day following symptom onset demonstrating patchy nodular consolidations with peripheral ground glass opacities in axial and sagittal views of the right lung. Reprinted with permission from Ref.27, which is open access and published under the Creative Commons License.
Similarly, Qiu et al. observed that 53% of pediatric patients presented with pulmonary GGOs consistent with characteristic COVID-19 pneumonia via chest CT (n = 36).35 Clinical presentation among these patients was variable, with 30% of pediatric patients having either fever or cough, 22% presenting with pneumonia, and 28% having no symptoms of pneumonia (n = 36). Differences in pulmonary GGOs between younger (0 to ≤5 years) and older (>5 to ≤16 years) pediatric patients were not statistically significant.35 The distribution of pulmonary lesions in pediatric COVID-19 patients is summarized in Table 3.
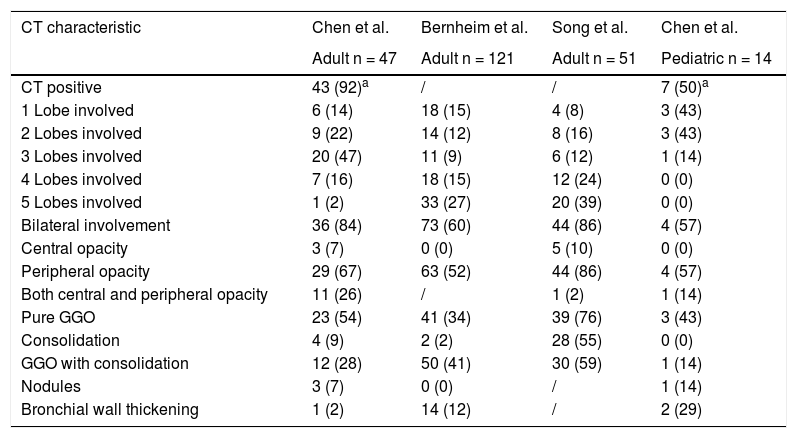
In a Zhejiang, China-based study, Liu et al. reported the following CT abnormalities: a consolidation lesion in the central region of the right lower lobe of an 11-month old with cough, fever, and fatigue; a GGO lesion in the interlobular subpleural area of the right middle lobe of a 9-year old with fever; pleural effusion and multiple consolidation lesions with air bronchogram in the right upper lobe of a 2-month old.36 Liu et al. also found that unlike those of adults, the non-specific CT abnormalities in pediatric COVID-19 (e.g., GGOs or consolidation) were distributed without peripheral predominance.36 Compared to adults, children and infants are generally at a higher risk for hospitalization following viral respiratory infections. The higher susceptibility in pediatric patients is thought to be due to children’s immature immune and respiratory systems.37 It is unknown, therefore, why pediatric cases of COVID-19 are typically less frequent and less severe than their adult counterparts.8–10Table 4 summarizes key differences in adult and pediatric CT findings, based on availability of comparable data.
Comparing CT findings between adult and pediatric patients with COVID-19 [n (%)].
| CT characteristic | Chen et al. | Bernheim et al. | Song et al. | Chen et al. |
|---|---|---|---|---|
| Adult n = 47 | Adult n = 121 | Adult n = 51 | Pediatric n = 14 | |
| CT positive | 43 (92)a | / | / | 7 (50)a |
| 1 Lobe involved | 6 (14) | 18 (15) | 4 (8) | 3 (43) |
| 2 Lobes involved | 9 (22) | 14 (12) | 8 (16) | 3 (43) |
| 3 Lobes involved | 20 (47) | 11 (9) | 6 (12) | 1 (14) |
| 4 Lobes involved | 7 (16) | 18 (15) | 12 (24) | 0 (0) |
| 5 Lobes involved | 1 (2) | 33 (27) | 20 (39) | 0 (0) |
| Bilateral involvement | 36 (84) | 73 (60) | 44 (86) | 4 (57) |
| Central opacity | 3 (7) | 0 (0) | 5 (10) | 0 (0) |
| Peripheral opacity | 29 (67) | 63 (52) | 44 (86) | 4 (57) |
| Both central and peripheral opacity | 11 (26) | / | 1 (2) | 1 (14) |
| Pure GGO | 23 (54) | 41 (34) | 39 (76) | 3 (43) |
| Consolidation | 4 (9) | 2 (2) | 28 (55) | 0 (0) |
| GGO with consolidation | 12 (28) | 50 (41) | 30 (59) | 1 (14) |
| Nodules | 3 (7) | 0 (0) | / | 1 (14) |
| Bronchial wall thickening | 1 (2) | 14 (12) | / | 2 (29) |
This paper reviews radiologic profiles of both pediatric and adult or elderly cases to comment on the role of CT imaging to reliably detect COVID-19 within these risk groups. Initial CT scans in adults routinely featured ground glass opacities (GGOs) in 74% (n = 698) and bilateral abnormalities in 89% (n = 378), while initial scans of pediatric patients evidenced 60% (n = 25) and 37% (n = 46), respectively. At 9–13 days post-onset of initial symptoms (e.g., fever, fatigue, cough), adult CT findings included crazy paving in 19% (n = 36) and increased rates of bilateral lung involvement in 86% (n = 36) of infected patients. At 14+ days, CT scans evidenced varied degrees of improvement in adults but no resolution until at least 26 days after the onset of symptoms. In pediatric patients, a third (n = 9) showed additional small nodular GGOs limited to a single lobe 3–5 days after an initial CT scan. Future research should focus on confirming the sensitivity and specificity results discussed in this appraisal of previous radiologic findings. How CT may affect clinical management may also be explored, although it seems to be limited to diagnosing complications (e.g., pulmonary embolism) as there is no treatment at present. Nevertheless, CT has provided a wealth of information to update providers on CT findings specific to patients based on their age and time of symptom onset.
CT imaging has demonstrated an ability to allow for the identification of pulmonary abnormalities underlying COVID-19 symptoms. However, age-related variability in symptom presentation and disease progression confers a challenge to clinical diagnosis. To date, there is no exhaustive list of common CT manifestations in pediatric cases of COVID-19, leading medical professionals to question the usefulness of CT imaging in such patients. If pediatric patients are generally asymptomatic or CT findings are nondescript, the risk benefit must be evaluated for exposing children to ionizing radiation. This lack of available peer-reviewed data on pediatric patients was our primary limitation and was why we chose to include a preprint in our review (Table 3). If sufficient studies on pediatric patients were available, we could conduct more meaningful analyses, such as analyzing the rate of CT findings reported in terms of the demography, the diagnostic gold standard, RT-PCR, and case selection algorithms, and presenting the aggregated typical and atypical findings at different stages of disease progression in pediatric patients.
Meanwhile, CT imaging of older individuals routinely features bilateral GGOs without consolidation, thickened intralobular septa, and pleural thickening. However, there have been reports that CT specificity in adults is as low as 19%–30%, much lower than the sensitivity in either adults (reported as 97% by this study, n = 601) or children (44%, n = 50).38 CT imaging has distinguished disease severities and stages; however, this level of scrutiny is not yet available for COVID-19 in children.39,40
CT has proven to be a useful imaging modality for distinguishing between mild and severe COVID-19 pneumonia. Current studies on CT imaging of individuals with COVID-19 have demonstrated higher incidence of abnormal sizing of GGOs and ill-defined margins than healthy patients.17,22 This characterization is crucial given the limited availability to viral testing kits, but due to variability in symptom presentation, it may be appropriate to view this imaging modality as a secondary confirmatory tool following the use of viral tests, as recommended by the American College of Radiology.41 Due to the novelty and variable symptom presentation of COVID-19, this disease is susceptible to both underdiagnosis and misdiagnosis. Furthermore, comparison of diagnostic tools is limited by the initial degree of sensitivity present in these modalities. It must also be mentioned that many of the imaging and procedural findings discussed in the current review are limited to preliminary, retrospective research on COVID-19 from China. As a result, these radiologic findings may not be representative of a larger, more diverse demographic.
Many of the studies examining the use of primary CT imaging support the notion that the imaging features of COVID-19 pneumonia are highly nonspecific and are more often bilateral with subpleural and peripheral distribution and range from GGOs in milder forms to consolidations in more severe forms.42 Similar radiologic findings are also present among those impacted by environmental pollution.43 Hansell and others demonstrate how abnormal lungs present on thin-slice CT are characterized by pleural thickening and aging lung parenchyma.44,45 This parallelism and ambiguity calls for additional comparative studies examining radiologic findings from affected populations in different geographic regions in order to enhance specificity and pattern recognition of these imaging techniques.
ConclusionOur study observes several limitations, including the limited number of studies comparing radiologic findings in adult and pediatric COVID-19 patients, methodological heterogeneity between studies, and relatively small sample sizes of included studies. In early SARS-CoV-2 cases, bilateral lung abnormalities, especially right lower lobe and left lower lobe abnormalities, and GGOs were found in 90%+ of patients, conferring with later study findings.46,47 Another common finding in adults, albeit less common, was interlobular septal thickening. There is some heterogeneity across studies suggesting limitations in how translatable typical findings are from one population or healthcare system to another (several articles quoted are Chinese or Korean in origin, for example). Observed inconsistencies in early COVID-19 reports may exist not only in testing algorithms, but also reporting and demography, contributing to the heterogeneity of results. For pediatric patients, the sensitivity of CT is significantly lower, perhaps because the radiologists were misdiagnosing abnormalities, or the scans were actually normal because the symptoms were non-respiratory. Although bilateral lung abnormalities and GGOs were also the most common findings in pediatric patients, even these findings were found in a maximum of 60% of patients from the studies reviewed. Above all, the available data supports chest CT for patients who are not progressing well, or for whom there are diagnostic doubts. The authors hope the age-sensitive findings described here will encourage more robust, initial data collection in the event of a future pandemic.
Authorship- 1.
Study integrity: JVW.
- 2.
Study concept: JVW.
- 3.
Study design: JVW.
- 4.
Data acquisition: KKL, MD.
- 5
Data analysis and interpretation: TM, AA, JVW.
- 6.
Statistical processing: REC.
- 7.
Literature search: ChA.
- 8.
Drafting of the paper: JVW, SB.
- 9.
Critical review of the manuscript with intellectually significant contributions: TH.
- 10.
Approval of the final version: TH.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.
Please cite this article as: Waller JV, Lin KK, Diaz MJ, Miao T, Amireh A, Agyemang Ch, et al. Comparación de los hallazgos en la tomografía computarizada de pacientes adultos y pediátricos con COVID-19. Radiología. 2021;63:495–504.