To determine the usefulness of MR enterography in the detection of recurrence in the ileocolonic anastomosis in patients with Crohn's disease that have undergone intestinal resection.
Material and methodsWe used MR enterography and ileocolonoscopy to study 30 patients with Crohn's disease who had undergone intestinal resection. To determine the degree of relapse, the findings at MR enterography were quantified using our own index of Crohn's disease activity and the findings at ileocolonoscopy were quantified using the Rutgeerts scale. Ileocolonoscopy was considered the gold standard.
ResultsCompared to the gold standard, MR enterography yielded 100% sensitivity, 60% specificity, 92.6% positive predictive value (PPV), 100% negative predictive value (NPV), and 93.3% diagnostic accuracy. The concordance between the degree of recurrence determined with MR enterography and with ileocolonoscopy was moderate (κ=0.41). However, when patients were classified into two groups (high or low grade) according to outcome and the possibility of repeat surgery, the concordance was excellent (κ=0.87). Using this classification, MR enterography had 85% sensitivity, 100% specificity, 100% PPV, and 76.9% NPV.
ConclusionsMR enterography is a useful imaging method for detecting recurrence of Crohn's disease after surgery and for differentiating between patients with higher or lower risk of poor outcome. MR enterography has good concordance with ileocolonoscopy and is an alternative to ileocolonoscopy in determinate occasions.
Demostrar la utilidad de la RM-enterografía (RM-E) en la detección de recurrencias en la anastomosis ileocolónica en pacientes con enfermedad de Crohn (EC) que han sufrido una resección intestinal previa.
Material y métodosSe estudió a 30 pacientes con EC e historia de resección intestinal mediante RM-E e ileocolonoscopia. Para determinar el grado de la recurrencia, los hallazgos se cuantificaron mediante un índice propio de actividad de la EC en RM y mediante el índice endoscópico de recurrencia de Rutgeerts, respectivamente. Se consideró a la ileocolonoscopia como el patrón de referencia.
ResultadosLa RM-E mostró para la detección de recurrencia sensibilidad del 100%, especificidad del 60%, valor predictivo positivo (VPP) del 92,6%, valor predictivo negativo (VPN) del 100% y exactitud diagnóstica del 93,3%. La concordancia entre el grado de la recurrencia determinado por RM-E y por ileocolonoscopia fue moderada (κ=0,41). Sin embargo, después de establecer solo dos grupos (alto o bajo grado) que indican el comportamiento evolutivo y la posibilidad de nueva cirugía, la concordancia pasó a ser excelente (κ=0,87). Para este supuesto se obtuvo sensibilidad del 85%, especificidad del 100%, VPP del 100% y VPN del 76,9%.
ConclusionesLa RM-E es un método de imagen útil para detectar la recurrencia posquirúrgica en la EC y diferenciar entre grupos de mayor o menor riesgo evolutivo. Su concordancia con la ileocolonoscopia es alta, por lo que puede ser una alternativa en determinadas ocasiones.
About 80% of patients with Crohn's disease (CD) require bowel resection at some point in their life to address complications. Unfortunately, surgery does not cure the disease and recurrence is generally the norm, usually at the anastomosis and neoterminal ileum. In the absence of treatment, 65–90% of patients will have endoscopic recurrence at one year and 80–100% at 3 years. Regarding clinical recurrence, 20–30% of patients will have symptoms of recurrence at 1 year, with a 10% increase in each of the subsequent years, and 40–50% of patients will need repeat surgery at 10 years.1 Early detection of endoscopic recurrence, even in asymptomatic patients, and the use of the most appropriate treatment for each case aim at modifying the course of CD and avoiding repeat surgery.2 To that end, protocolized use of ileocolonoscopy 6–12 months after surgery is indicated.
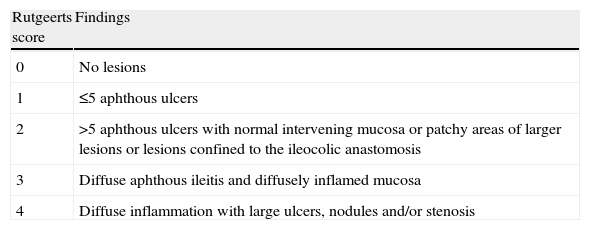
The diagnosis of postoperative recurrence should be established by ileocolonoscopy, considered the reference standard. The presence and severity of the lesions are defined by a specific scoring system described by Rutgeerts et al., who demonstrated the correlation between severity of endoscopic lesions, clinical recurrence and behaviour after recurrence.3 Thus, patients with no mucosal lesions or minor endoscopic abnormalities will have a good outcome, while severe endoscopic abnormalities are related to higher clinical recurrence rates and worse outcome.
Cross-sectional imaging modalities have proved very useful in the study of patients with CD.4 They emerge as alternative or complementary techniques to endoscopy, which may be difficult or even impossible to perform in some patients. Nonetheless, in order to evaluate the usefulness of a given imaging modality, this has to be correlated with any of the accepted reference standards: endoscopy, histological findings or histopathological examination of surgical specimens.5 In this respect, the modalities used in the diagnosis of postoperative recurrence that have been correlated with ileocolonoscopy include ultrasonography (US),6,7 MR-enteroclysis,8 CT-enterography and CT-enteroclysis,9,10 and oral contrast-enhanced US,11 but we have found no references in the literature regarding the usefulness of MR-enterography (MR-E). Given the fact that MR-E is reproducible, well tolerated, free of ionizing radiation and validated for the study of CD,12–14 we decided to demonstrate if its results, taking endoscopy as the reference standard, were similar to those reported for the imaging techniques mentioned above.
Materials and methodsA total of 33 patients with CD who underwent previous bowel resection were prospectively studied. Between November 2008 and December 2009, 15 cases were incorporated into a larger study on the use of MR-E in ileal CD.15 Between January and April 2010, and in order to study specifically the role of MR-E in postoperative recurrence, 18 patients who had undergone bowel resection were also enrolled, without taking into account their clinical status. Three patients were excluded: two (from the first group) because they had undergone resection of the jejunum or proximal ileum (areas that are not depicted with standard ileocolonoscopy), and in one patient the RM-E study could not be completed because of incoercible vomiting after ingestion of the oral solution. The age of the 30 patients who were finally enrolled in the study ranged from 17 to 64 years (median 40). Of these patients, 67% were women (n=17) and 40% were smokers (n=12). Of them, 47% (n=14) had clinical symptoms compatible with a flare-up of CD, while 53% (n=16) were asymptomatic. The elapsed time between surgery and RM-E ranged from 2 months to 11 years (median, 4 years and 10 months). It was considered “anastomosis” any ileal segment of up to 4cm proximal to the site of surgical connection. All patients gave written consent, and the study was approved by the local ethics committee.
MR-E studies were performed on a 1T MR scanner (Philips Intera; Best, Netherlands), with a 15mT/m gradient amplitude and a multichannel coil covering the abdomen, from the xiphoid process to the symphysis pubis.
After fasting for at least 8h, each patient ingested 1.5l of polyethylene glycol-electrolyte solution over 45min. Bowel cleansing preparation was not prescribed. The patients were imaged supine, and the field of view was adjusted to the anatomy of each patient.
First, dynamic images were obtained for “MR-fluoroscopy” using coronal 80 mm-thick SS-TSE (TR 8000/TE 90) fat-suppressed sequences that allow for the monitoring of the degree of bowel loop filling, as well as for the evaluation of their peristalsis and distension.
If loop filling was adequate, 20mg hyoscine butylbromide or 0.5mg glucagon intravenously were given in order to eliminate motion artifacts from bowel peristalsis. Next, axial and coronal images were obtained using fast SS-TSE (TR 2500/TE 240) sequences with a 6mm slice thickness and a 1mm interslice gap with a 512×205 matrix and axial and coronal B-FFE (coherent gradient echo) sequences (TR 7.5/TE 3.7) with a 60° flip angle, a 5mm slice thickness, a 1mm interslice gap, and a 560×272 matrix. Lastly, a coronal 3D-THRIVE (T1-EG with fat suppression and isotropic resolution) sequence (TR 6.2/TE 3.2) was obtained with a 10° flip angle, a 4.2mm thickness, and a 256×141 matrix, before and after the administration of an IV bolus injection of gadopentetate dimeglumine (Magnevist®, Bayer) at 0.1mmol/kg. Patients with high body mass index, or when motion artifacts from bowel peristalsis were detected, were given a second dose of spasmolytic immediately before the 3D-THRIVE sequence.
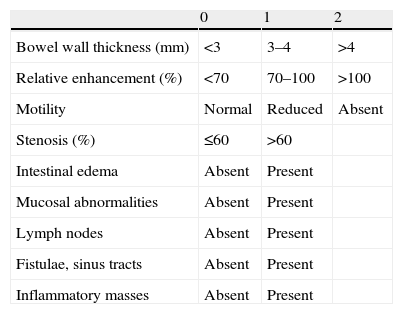
Two radiologists with experience in abdominal MRI interpreted the results and the differences were resolved by consensus. The degree of recurrence was assessed at the anastomosis site using a CD activity index that is regularly used in our hospital, whose calculation method is shown in Table 1. This index, already described in detail in a previous paper,15 is a modification of that developed by Girometti et al.,16 is multifactorial and allows us to assign a score from 0 to 12 to each patient. Scores≤2 are considered inactive disease. For the purposes of the present study and to compare the value of the MRI index with the degree of endoscopic recurrence, three more groups were considered with scores 3–5, 6–8 and ≥9.
Scoring for MR-E index.
| 0 | 1 | 2 | |
| Bowel wall thickness (mm) | <3 | 3–4 | >4 |
| Relative enhancement (%) | <70 | 70–100 | >100 |
| Motility | Normal | Reduced | Absent |
| Stenosis (%) | ≤60 | >60 | |
| Intestinal edema | Absent | Present | |
| Mucosal abnormalities | Absent | Present | |
| Lymph nodes | Absent | Present | |
| Fistulae, sinus tracts | Absent | Present | |
| Inflammatory masses | Absent | Present |
Modified from Girometti et al.16
Ileocolonoscopy was performed for all patients within 15 days of the MRI study and was performed by gastroenterologists with experience in inflammatory bowel disease, blinded to the MR findings and without modification of the treatment the patients received between both examinations. The anastomosis was reached in the 30 patients included in the study, and the neoterminal ileum (at least 10cm) in 13. In the remaining patients, the presence of stenosis at the anastomosis site prevented passage of the endoscope. All 30 patients were scored according to the Rutgeerts classification (shown in Table 2), where group i0 includes patients without recurrence and group i4 patients with severe recurrence.
Classification of endoscopic findings in postoperative recurrences of Crohn's disease.3
| Rutgeerts score | Findings |
| 0 | No lesions |
| 1 | ≤5 aphthous ulcers |
| 2 | >5 aphthous ulcers with normal intervening mucosa or patchy areas of larger lesions or lesions confined to the ileocolic anastomosis |
| 3 | Diffuse aphthous ileitis and diffusely inflamed mucosa |
| 4 | Diffuse inflammation with large ulcers, nodules and/or stenosis |
For the statistical analysis of the results, ileocolonoscopy was used as the reference standard, where the Rutgeerts score i0 included patients with inactive disease, scores i1 and i2 included patients with low disease activity, and i3 and i4 included patients with high disease activity. Based on this premise, the following statistical parameters were calculated for the results obtained by applying the RM-E index: sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy. Cross tabulation and Cohen's κ coefficient were used to calculate the degree of concordance between ileocolonoscopy and RM imaging.
ResultsEndoscopic studies revealed recurrence at the anastomosis site in 25 patients (score i1–i4), while 5 patients were free of recurrence (i0). Of the 25 patients with recurrent CD, one scored an i1, 4 scored an i2, 8 scored an i3, and 12 scored an i4. The neoterminal ileum could be imaged in 13 patients, with 8 cases of recurrence.
MR-E examinations (Figs. 1–4) showed signs of recurrence (score≥3) in 27 patients. Two of them showed no endoscopic recurrence and they were therefore considered false positives. No false negative results were detected. These results correspond to a sensitivity of 100%, specificity of 60%, PPV of 92.6%, and NPV of 100%. The diagnostic accuracy of MR-E for the detection of activity was 93.3%.
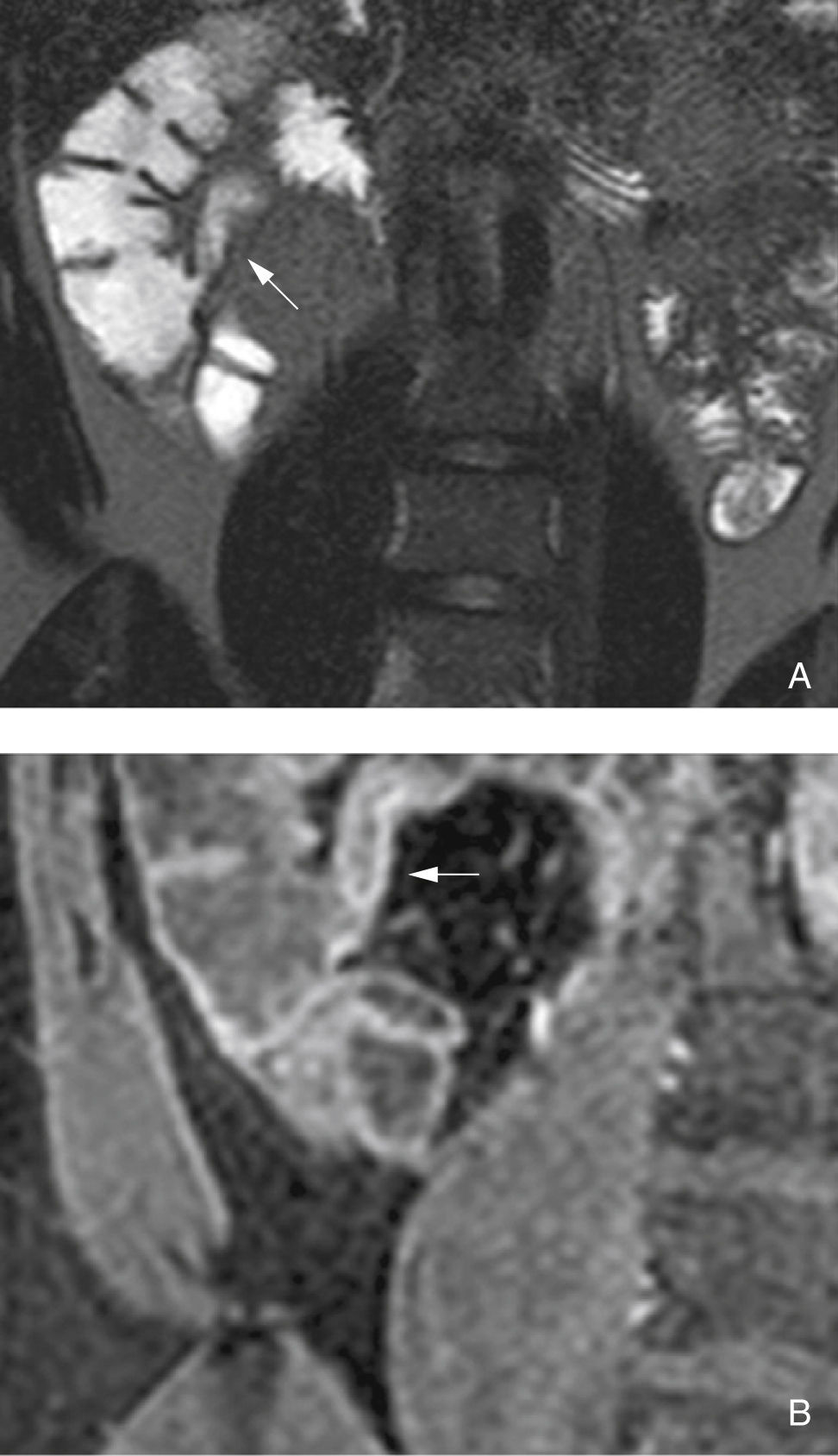
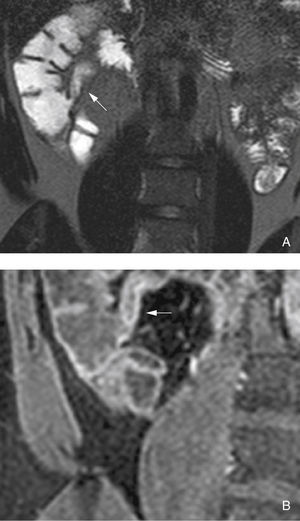
Anastomosis with no signs of recurrence (Rutgeerts i0). (A) Coronal SS-T2-TSE image shows no wall thickening and no hyperintense signal at the anastomosis site (arrow). (B) Coronal fat-suppressed postgadolinium T1-EG image shows normal enhancement (<70% in comparison with the study without contrast, not shown).
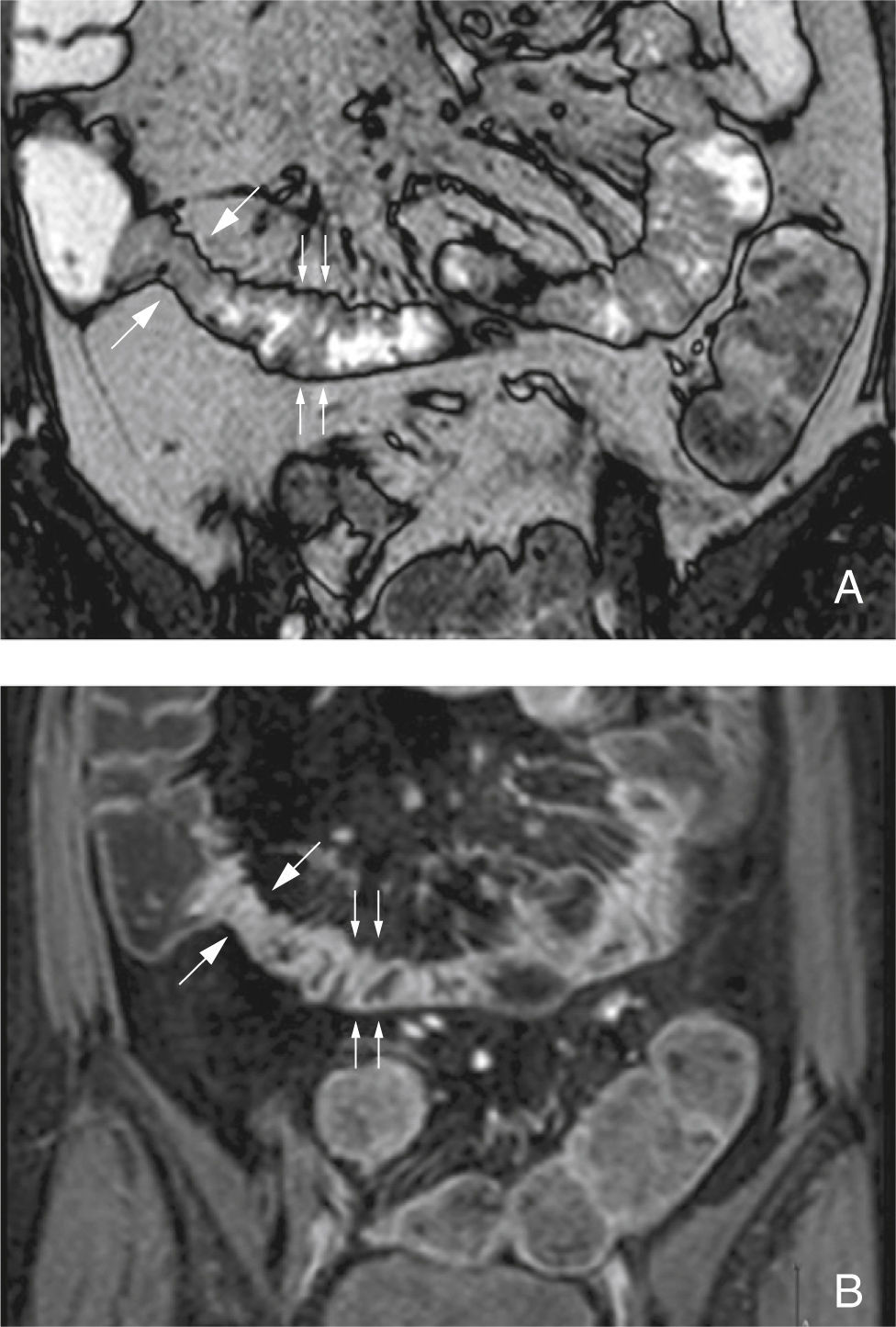
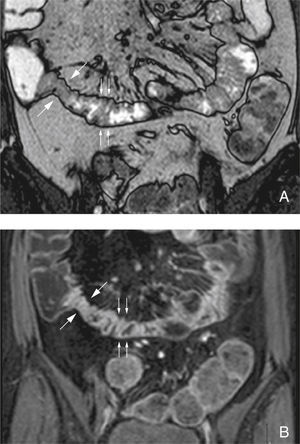
Low-grade recurrence (Rutgeerts i2) involving the anastomosis (large arrows) and the neoterminal ileum (small arrows). (A) Coronal B-FFE image shows wall thickening and irregular mesenteric margin of the anastomosis (large arrows), adjacent to a segment of neoterminal ileum of about 8cm (small arrows), with focal wall thickening seen as pseudopolyps. (B) Coronal fat-suppressed postgadolinium T1-EG sequence shows hyperenhancement of both structures.
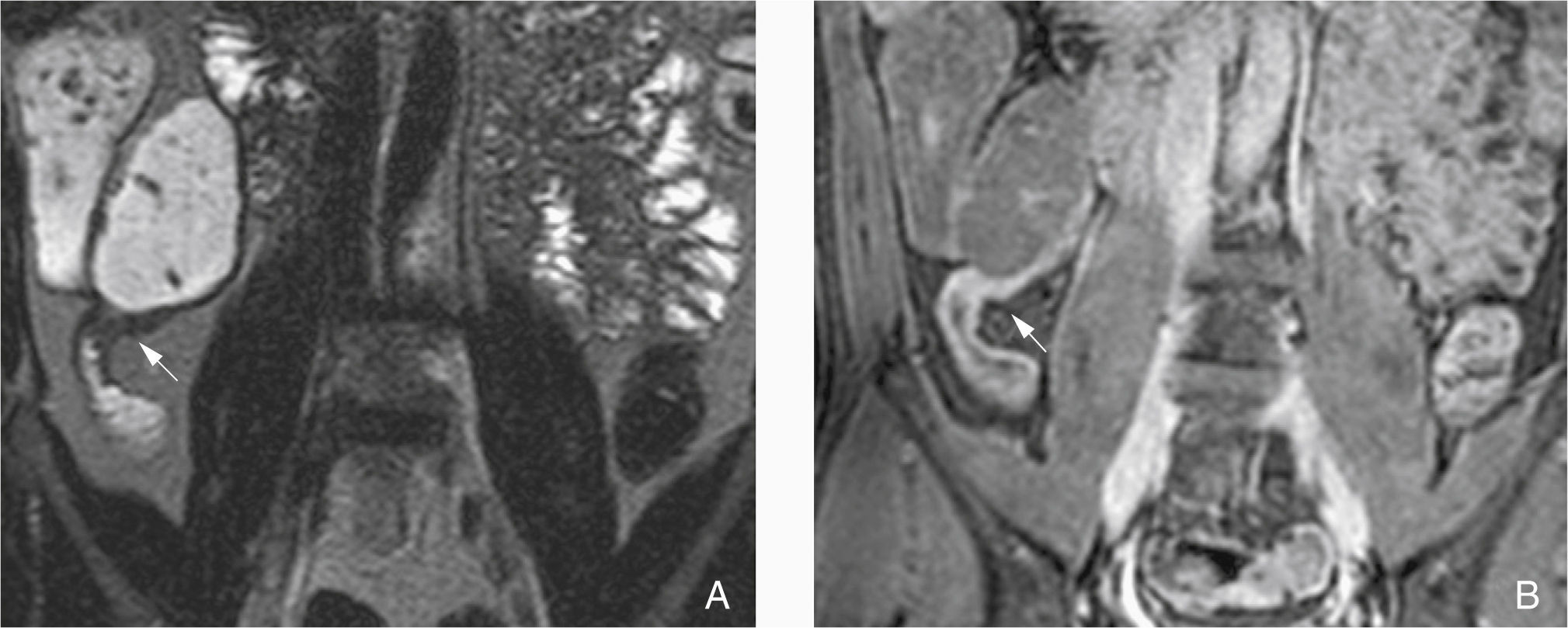
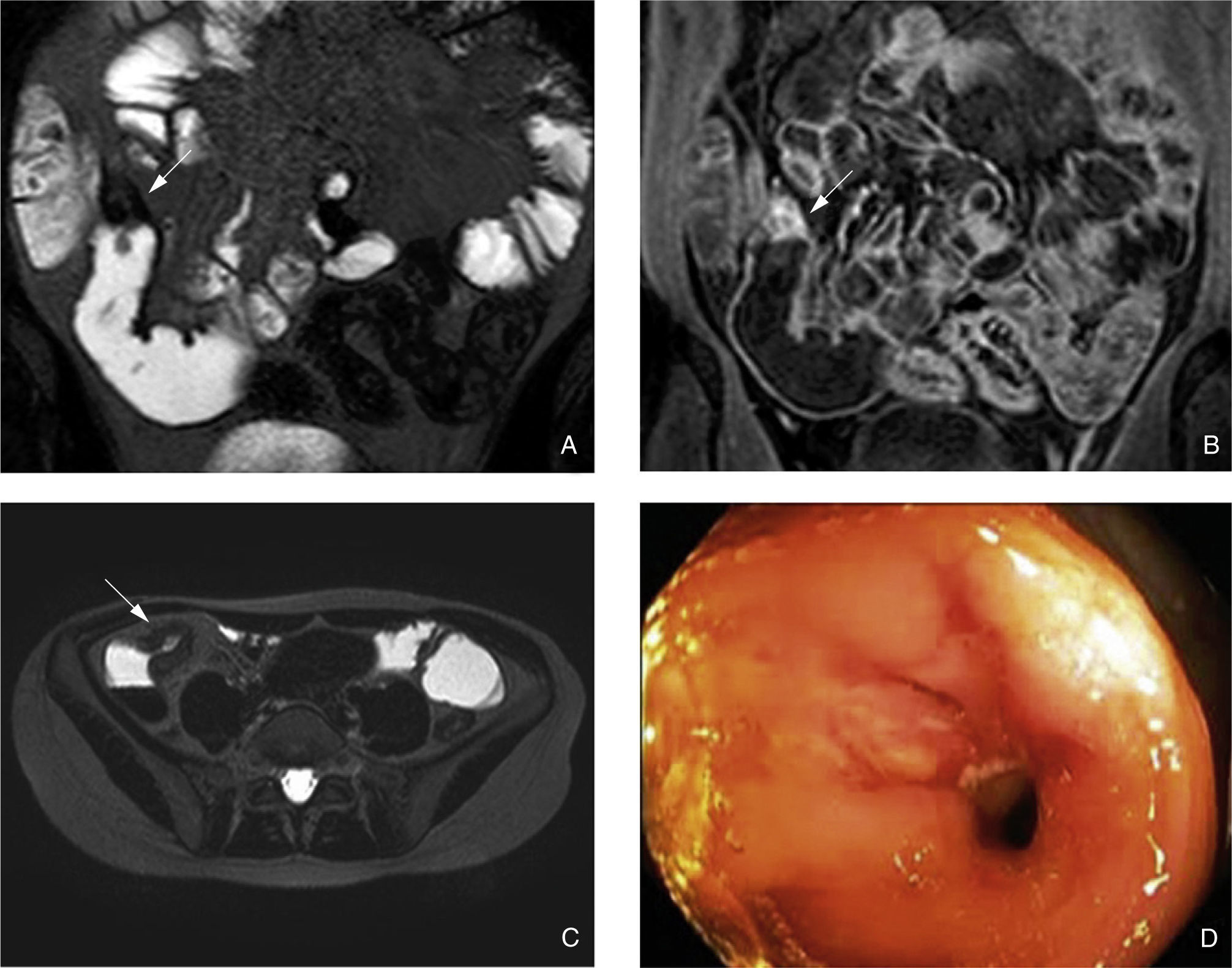
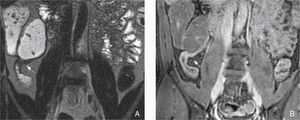
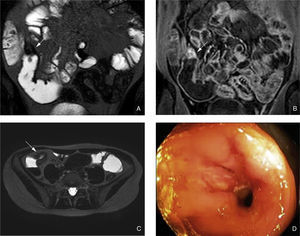
High-grade recurrence (Rutgeerts i4) confined to the anastomosis (arrow). (A and C) SS-T2-TSE sequences show wall thickening of a short segment at the level of the ileocolic anastomosis. (B) Coronal fat-suppressed postgadolinium T1-EG sequence shows enhancement of the thickened segment. (D) Endoscopic image of the anastomosis shows a large geographic ulcer that involves 1/3 of the lumen circumference, causing partial stenosis.
MR-E revealed that in 21 of the 25 patients with recurrent CD the neoterminal ileum was also involved. These corresponded to the 8 cases confirmed by ileocolonoscopy and to 13 cases where the endoscope was not able to go through the anastomosis.
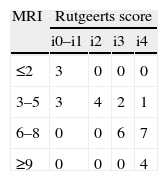
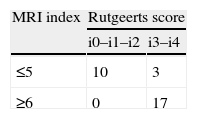
Determination of the degree of recurrenceWhen comparing the MR-E index with the Rutgeerts endoscopic score, it should be taken into account that aphthous ulcers practically cannot be visualized on MR imaging. This forces us to group Rutgeerts scores i0 and i1 together into one single group in order to establish the degree of concordance, resulting in four degrees of endoscopic severity that would correlate with the four degrees of the MR-E index (no recurrence, ≤2; mild recurrence, 3–5; moderate recurrence, 6–8; and severe, ≥9). Based on this grading system (Table 3), the concordance between both techniques was moderate (κ=0.41).
However, if the patients are classified into two main groups, as done by other authors,5,6 patients with no recurrence or mild recurrence (low grade) and with moderate or severe recurrence (high grade) (Table 4), based on a worse prognosis and on the need of a more aggressive treatment, the concordance between both techniques was excellent (κ=0.87). By using this classification, a diagnostic accuracy of 90%, a sensitivity of 85%, a specificity of 100%, a PPV of 100%, and a NPV of 76.9% were obtained. Nonetheless, it should be noted that in this case, the degree of recurrence was underestimated in 3 patients (the only non-concordant cases), since they were classified as having low-grade MR recurrence, even though they actually had high-grade endoscopic recurrence.
DiscussionThe use of a cross-sectional imaging technique in CD is mandatory due to the ability of these techniques to depict lesions beyond the bowel mucosa, that is, lesions that might have extended to deeper layers or to extraenteric structures, which could be overlooked on barium or endoscopic studies. Additionally, cross-sectional techniques can detect changes in regions inaccessible to ileocolonoscopy. None has proven clearly superior to the others for such purposes17 and, when possible, those techniques that do not expose the patient to ionizing radiation are recommended.
There are no studies that compare different imaging techniques to assess the recurrence of CD in patients with previous bowel resection, as is the case in the present paper. Moreover, we have not found any reference on the use of MR-E for such purpose, but it is known that this technique yields similar diagnostic accuracy to RM-enteroclysis in CD.18,19
Ultrasonographic evaluation of postoperative recurrence,6,7,11 through the assessment of wall thickness at the anastomosis, has a sensitivity of 79–92.5%, a specificity of 20–95%, a PPV of 95–95% and a NPV of 16.6–80%. However, by establishing a cut-off of 5mm for bowel wall thickness, Rispo et al.7 obtained an excellent correlation between ultrasonography and endoscopy in differentiating mild from severe recurrence (κ=0.9).
Using CT, Minordi et al.9 reported a statistically significant correlation between certain imaging parameters (basically, mural thickening with a “layered enhancement” pattern and signs of extraenteric involvement) and different degrees of endoscopic recurrence. Based on these findings, they establish four degrees of activity, reporting a sensitivity, specificity and diagnostic accuracy of 96.9%, 100%, and 97%, respectively, in the detection of recurrences. However, they do not provide information regarding the concordance of the degrees of activity with endoscopy. In their study, CT-enteroclysis and CT-enterography were used interchangeably, without providing the data from each technique separately, although the authors point out that CT-enteroclysis should be the first-choice technique. More recently, using CT-enteroclysis Soyer et al.10 have carried out a study in 40 patients to differentiate inflammatory from fibroestenotic recurrent lesions. The authors claim that the presence of five variables simultaneously (anastomotic stenosis, wall thickening, absence or mild enhancement, absence of comb sign and absence of fistula) is characteristic of fibroestenosis.
Regarding MR imaging, there is only one reference on the use of MR-enteroclysis by Sailer et al.8 They do not provide data on sensitivity, specificity or diagnostic accuracy, but they do provide information on the concordance with endoscopic scores. The MRI score system that they have developed has four degrees of recurrence and a good concordance (κ=0.63) with the endoscopic Rutgeerts score, somewhat lower for the anastomosis (κ=0.49). When establishing only two groups, low and high activities, the concordance between MR and endoscopy rises to a κ=0.85, that is, excellent concordance. In a more recent study, this working group concludes that, given the existing concordance, MR-E may have a similar prognostic value to that of ileocolonoscopy for predicting recurrence.20
In our study, MR-E has a sensitivity and a NPV of 100% for the detection of recurrence, findings that seem to support its use as an alternative or as a complement to endoscopy in the study of these patients. The presence of false positive results (patients without recurrence who are classified as having mild activity) may be explained by the difficulty to evaluate the anastomosis site, an extremely short bowel segment that has undergone surgical manipulation, a difficulty that has also been acknowledged by other studies.8 Of course, other modalities such as US or CT can be used for this same purpose; however, in comparison with US, MRI has the advantage of providing an easier assessment of the rest of the small bowel, and unlike CT, it does not use ionizing radiation.
On the other hand, our results seem to support the use of MR-E in the assessment of the degree of recurrence, which is ultimately the most relevant issue, with very similar results to those reported for MR-enteroclysis.8 Overall, although the concordance between our MR-E score and the endoscopic score is somewhat lower (κ=0.41), when patients were categorized into high and low grade, which determines whether therapeutic intervention is required or not, the concordance was excellent (κ=0.87). However, some patients with severe recurrence were classified as having mild recurrence on RM-E, which represents a serious limitation to this examination.
Other limitations to this study include, first, the fact that the elapsed time from surgery to MR-E varied among patients and, second, the relatively small number of patients included, although it falls within the range of other studies, with high prevalence of recurrence, which is characteristic of CD. Despite its general acceptance, the Rutgeerts score also seems to have limitations, as severe stenoses may not have inflammatory activity. The results regarding the correlation with MR-enteroclysis should be interpreted with caution as the methods for assessing the activity with MR imaging are different, and the populations may differ in other characteristics such as the elapsed time from bowel resection or the surgical technique used. Lastly, a limitation inherent to the present study and to all the studies discussed here is the fact that endoscopy can only depict mucosal lesions, while MR imaging has the ability to depict the entire bowel wall and extraenteric structures. Nonetheless, we believe that these limitations do not affect significantly the results of our study or the findings reported.
In conclusion, we find that MR-E is a useful imaging technique for the detection of CD recurrence in patients with small bowel resection. The concordance of MR-E with endoscopy is similar to that of other imaging techniques, in particular, of MR-enteroclysis. However, although in very few cases, MR-E is not able to differentiate between mild and severe recurrence; for this reason, in cases of postoperative recurrence detected by MR-E, the use of endoscopy remains mandatory to determine more accurately the degree of recurrence.
Authorship- 1.
Responsible for the integrity of the study: J.C. Gallego.
- 2.
Conception of the study: J.C. Gallego, A.I. Echarri and A. Porta.
- 3.
Design: J.C. Gallego, A.I. Echarri and A. Porta.
- 4.
Acquisition of data: J.C. Gallego, A.I. Echarri and A. Porta.
- 5.
Analysis and interpretation of data: J.C. Gallego, A.I. Echarri and A. Porta.
- 6.
Statistical analysis: J.C. Gallego, A.I. Echarri and A. Porta.
- 7.
Bibliographic search: J.C. Gallego, A.I. Echarri and A. Porta.
- 8.
Drafting of the manuscript: J.C. Gallego, A.I. Echarri and A. Porta.
- 9.
Critical appraisal with intellectually relevant contributions: J.C. Gallego, A.I. Echarri and A. Porta.
- 10.
Approval of the final version: J.C. Gallego, A.I. Echarri and A. Porta.
The authors declare not having any conflict of interests.
Please cite this article as: Gallego Ojea JC, et al. Enfermedad de Crohn: utilidad de la RM-enterografía en la detección de recurrencias posquirúrgicas. Radiología. 2011;53:552–9.