To evaluate the frequency of acute pulmonary embolism, the use of clinical probability scores, and the appropriateness of the management of patients for whom computed tomography angiography (CTA) was requested from the emergency department for suspected acute pulmonary embolism.
Materials and methodsThis was a retrospective observational study of CTA studies requested from the emergency department to rule out acute pulmonary embolism. We analyzed clinical variables and the explicit use of clinical probability scores. We determined the appropriateness of management according to the Wells Score and Geneva Score and the simplified versions of these two scores, calculated retrospectively.
ResultsWe included 534 patients (52.8% women; mean age, 73 years). The frequency of acute pulmonary embolism was 23.0% and the Wells Score was explicitly used in 15.2%. The appropriateness of the management varied depending on the clinical probability score used to assess it (54.5%–75.8%) and on whether the standard d-dimer or age-adjusted d-dimer was used.
ConclusionsThe failure to use the Wells Scores in all cases does not necessarily imply inappropriate management, and the performance of global clinical judgment can be similar to that of clinical probability scores; however, specific studies are necessary to confirm this hypothesis.
Evaluar la frecuencia de tromboembolismo pulmonar agudo (TEPA), el uso de escalas de probabilidad clínica (EPC) y la adecuación del manejo de los pacientes a los que se solicitó angiografía pulmonar por tomografía computarizada (angio-TC) por sospecha de TEPA desde el servicio de urgencias.
Materiales y métodosEstudio observacional retrospectivo de las angio-TC solicitadas desde el servicio de urgencias para descartar TEPA. Se analizaron variables clínicas y el uso explícito de EPC. Se determinó la adecuación del manejo en función de las escalas de Wells (EW) y Ginebra (EG) y sus versiones simplificadas (EWs y EGs), calculadas retrospectivamente.
ResultadosSe incluyeron 534 pacientes (52,8% mujeres, mediana de edad: 73 años). La frecuencia de TEPA fue del 23,0% y el uso explícito de la EW, del 15,2%. La adecuación del manejo fue variable dependiendo de la EPC (54,5-75,8%) y del dímero D estándar o ajustado por edad.
ConclusionesLa baja utilización explícita de la EW no conlleva un manejo inadecuado, y el juicio clínico global puede ofrecer un rendimiento similar a las EPC, pero es necesario realizar estudios específicos para comprobar esta hipótesis.
Acute pulmonary thromboembolism (APTE) is one of the most frequent cardiovascular emergencies and is associated with significant morbidity and mortality, surpassed only by myocardial ischaemia and stroke.1 No significant differences have been demonstrated between the sexes and its prevalence increases exponentially with age.2–4 The spectrum of clinical manifestations is very varied and routine complementary tests (blood tests, chest X-ray, electrocardiogram), performed in the emergency department have low specificity, which is why specialised techniques are necessary for detection.2,3 The test of choice for the diagnosis of APTE is pulmonary computed tomography angiography (CT angiogram),5,6 which also enables other alternative diagnoses.7 However, this involves significant costs, radiation risks, and the use of intravenous iodinated contrast, so it should only be used following a suitable risk-benefit analysis.8,9
Despite the undoubted advances in the diagnosis of APTE in recent decades, prognosis has not improved to the same degree.6,10,11 Clinical probability scales (CPS), such as the Wells Scale (WS) and the revised Geneva Scale (GS) (Table 1), have been validated to identify patients at risk of APTE, which has helped clinical decision-making.6,12,13 The simplified versions of these CPSs (sWS and sGS, respectively) offer a similar diagnostic yield9,14 and are recommended by clinical practice guidelines (CPG) in combination with the determination of d-dimer (DD) levels to indicate the performance of CT angiography.4,6
Items of the reconstructed clinical probability scales.
| Items | Score | |
|---|---|---|
| Original version | Simplified version | |
| Wells Scale | ||
| Previous DVT or APTE | 1.5 | 1 |
| HR>100bpm | 1.5 | 1 |
| Surgery or immobilisation in the last month | 1.5 | 1 |
| Haemoptysis | 1 | 1 |
| Active cancer | 1 | 1 |
| Clinical signs of DVT | 3 | 1 |
| Alternative diagnosis less likely than APTE | 3 | 1 |
| Clinical likelihood of APTE | ||
| APTE unlikely | ≤4 | ≤1 |
| APTE likely | >4 | >1 |
| Geneva Scale | ||
| Previous DVT or APTE | 3 | 1 |
| HR: | ||
| 75–94bpm | 3 | 1 |
| ≥95bpm | 5 | 2 |
| Surgery or fracture in the last month | 2 | 1 |
| Haemoptysis | 2 | 1 |
| Active cancer | 2 | 1 |
| Unilateral pain in lower limb | 3 | 1 |
| Pain on palpation in the deep veins of the lower limbs and unilateral oedema | 4 | 1 |
| Age >65 years | 1 | 1 |
| Clinical likelihood of APTE | ||
| APTE unlikely | ≤5 | ≤2 |
| APTE likely | >5 | >2 |
APTE: acute pulmonary thromboembolism; DVT: deep vein thrombosis; HR: heart rate.
However, several studies have found scant use of CPS in the management of this entity,4,8,15 which could imply that CPGs are not adequately followed.8,9,12 Furthermore, in a recent study,4 variable adherence has been described depending on the age of the patients, although the reasons why this may occur have not been identified. The lack of application of CPSs can have negative consequences, such as an increase in unnecessary tests and associated costs, a delay in patient care, and increased morbidity and mortality.12
Despite the knowledge of and interest in APTE, there are discrepancies between studies in terms of sociodemographic variables, use of CPSs, adherence to CPG, and diagnostic yield of CT angiography, particularly between European and North American series.16 In our country, adherence to CPGs and their implications in the diagnostic process of APTE have rarely been studied, although there are some recent studies in this regard in our setting.17 The main objective of this study is to evaluate the frequency of APTE, the use of CPSs and the quality of management of patients undergoing CT angiography for suspected APTE requested by the emergency department.
Material and methodsStudy design and patient recruitmentA retrospective observational study (case series) was carried out by analysing CT angiographies requested by the emergency department of our hospital for suspected APTE between 1 January and 31 December 2018. The study was approved by our regional research ethics committee.
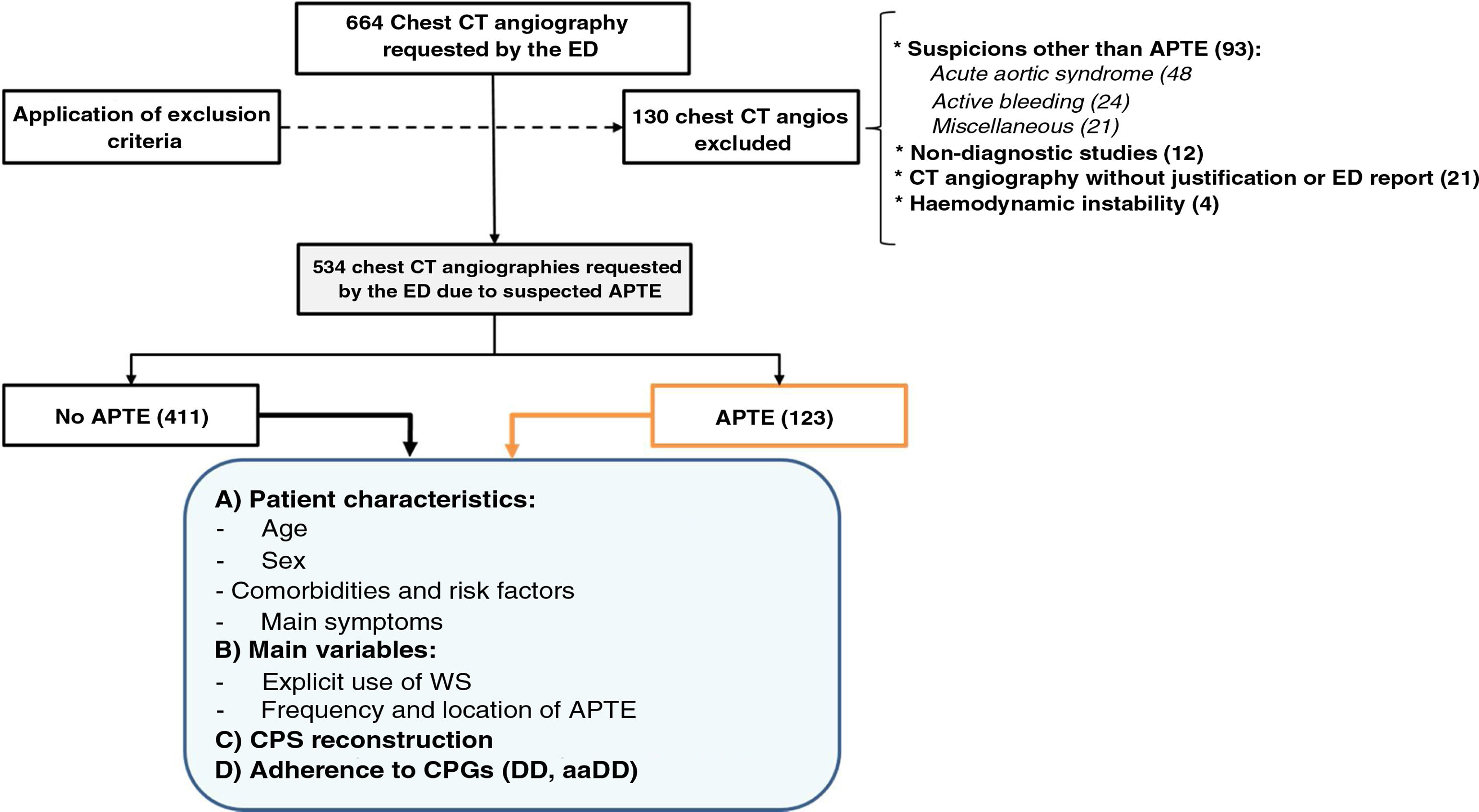
The cases were selected from the chest CT angiography registry in the PACS of our centre. All chest CT angiographies requested by the emergency department for suspected APTE were included. The exclusion criteria were: age less than 18 years, haemodynamic instability, suboptimal quality of the examination (non-diagnostic), suspicion other than APTE, lack of justification in the electronic request and unavailability of the emergency episode report. Fig. 1 shows the case selection flow chart.
Variables analysedMain variables: frequency of positive CT angiography for APTE according to the radiological report (“findings compatible with acute pulmonary thromboembolism” or equivalent); description of the CPS used per protocol in our centre (WS) in the electronic request for CT angiography or in the emergency report.
Patient characteristics: age and sex, associated diseases and risk factors (active neoplasia in the last 6 months, chronic obstructive pulmonary disease (COPD), diabetes mellitus, hypertension, obesity, active smoking, taking oral anticoagulants, taking oral contraceptives, prolonged immobilisation), main symptoms (dyspnoea, cough, syncope, chest pain, haemoptysis, signs of deep vein thrombosis [DVT]).
Standard and age-adjusted d-dimerThe DD value in our hospital is obtained using the ELISA method (reference standard),5 with a standard cut-off point of 500ng/ml to be considered positive. The intrinsic and extrinsic validity parameters of the standard and age-adjusted DD (aaDD) were analysed. With regard to the latter, the cut-off point was established in patients over 50 years of age according to the formula validated by Righini et al.18: age (years) ×10ng/ml.
Reconstruction of the clinical probability scales and adherence to clinical practice guidelinesUsing the data from the emergency report and/or the electronic CT angio request, two authors (AJLRB and RGL) collected the items from the different CPSs to reconstruct these scales in their complete (WS, GS) and simplified (sWS and sGS, respectively) versions independently and retrospectively (Table 1). Any disagreement was resolved by consensus. With this information, the patients were stratified dichotomously (“APTE likely” vs. “APTE unlikely”).14 The WS item “presence of a clinical diagnosis less likely than APTE” was scored positively if the first diagnostic orientation mentioned in the medical record was APTE.4
Management quality was evaluated using CPGs and internationally accepted algorithms based on risk stratification according to a validated CPS and the DD value to justify the performance of CT angiography.5,6,19 Thus, in the “APTE likely” group, adherence was considered adequate if CT angiography was performed without having previously requested DD levels, and in the “APTE unlikely” group, adherence to the CPG was adequate when the DD level was positive. Moreover, the difference in the appropriateness of management based on the use of standard DD and aaDD was evaluated.
As an indirect measure of the bias derived from retrospectively reconstructing the CPS, we determined the mismatch between the percentage of patients classified as “APTE likely” and “APTE unlikely” according to the explicit WS and according to the retrospective WS.
Statistical analysisThe cases were registered in a database anonymously. Qualitative variables were expressed as absolute and relative frequencies, and continuous quantitative variables as mean and standard deviation (SD). Uni- and bivariate analyses were performed on the variables studied according to the presence or absence of APTE. Student’s t tests were applied for comparison of means and χ2 for qualitative variables, after verification of the application conditions. If these conditions were not met, the corresponding non-parametric tests were applied. The statistical software package IBM SPSS Statistics version 22.0 was used. Values of p<0.05 were considered significant.
ResultsDescription of the seriesAfter eliminating cases that met the exclusion criteria (Fig. 1), a total of 534 patients (52.8% women) who underwent CT angiography due to suspected APTE requested by the emergency department were included. The median age was 73 years (range 18–101).
The most frequently associated pathologies were arterial hypertension (54.4%), diabetes mellitus (29.6%) and COPD (16.6%). Significant differences were found in the distribution of patients with COPD (p<0.05) and in the distribution of patients on anticoagulant treatment (p=0.001), which were more frequent in the group without APTE in both cases. On the other hand, signs of DVT (p=0.001) were more frequent in patients in the group with APTE. No significant differences were found between the APTE/no APTE groups for the remaining diseases, risk factors and symptoms studied. The detailed analysis of these data is shown in Table 2.
Characteristics and symptoms of the patients included in the study.
| Variable | N (%) | p (APTE vs. no APTE a) |
|---|---|---|
| Sex | ||
| Men | 252 (47.2) | – |
| Women | 282 (52.8) | – |
| Age x (s) | 69.6 (17.1) | – |
| Diseases and associated RF | ||
| AHT | 292 (54.4) | 0.196 |
| DM | 159 (29.6) | 0.109 |
| COPD | 89 (16.6) | 0.023b |
| Smoker | 72 (13.4) | 0.654 |
| Obesity | 50 (9.3) | 0.380 |
| Active neoplasia <6 months | 74 (13.9) | 0.892 |
| Taking oral anticoagulants | 51 (9.6) | 0.001b |
| Taking oral contraceptives | 6 (1.1) | 0.053c |
| Prolonged immobilisation | 80 (15.0) | 0.902 |
| Symptoms in the ED | ||
| Dyspnoea | 367 (68.7) | 0.430 |
| Cough | 137 (25.7) | 0.712 |
| Syncope | 110 (20.6) | 0.337 |
| Chest pain | 195 (36.5) | 0.233 |
| DVT signs | 57 (10.7) | 0.001d |
| Haemoptysis | 13 (2.4) | 0.319 |
AHT: arterial hypertension; APTE: acute pulmonary thromboembolism; COPD: chronic obstructive pulmonary disease; DM: diabetes mellitus; DVT: deep vein thrombosis; RF: risk factors.
In 123 patients (23.0%) the CT angiography was positive for APTE according to the radiological report — 68 were central and 55 peripheral. The WS was explicitly recorded in the case history in 81 patients (15.2%).
Reconstruction of the clinical probability scales and adherence to clinical practice guidelinesThe total frequency of cases in which CPGs were correctly followed (DD and CT angiography were justified), according to the stratification of each CPS, was higher in the WS (75.8%) followed by the sWS (68.4%), the sGS (55.4%) and the GS (54.5%).
According to the WS, 69 patients were stratified as “APTE likely” (12.9%), a frequency that, according to the sWS, amounted to 141 cases (26.4%). There was a discrepancy of 8 cases (9.8%) between the explicit WS stratification categories (in the patients in whom it was present) vs. those of the retrospective WS. On the other hand, the GS showed a total of 243 cases (45.5%) of “APTE likely”, a figure that dropped to just 232 (43.4%) in the sGS. When comparing the “APTE likely” and “APTE unlikely” according to whether CT angiography was positive for APTE or not, significant differences were found for all the CPSs used.
Regarding DD, of the 471 requests made, 409 were justified according to the WS because they were “APTE unlikely” and 62 DD were requested in patients classified as “APTE likely”. Of the justified requests according to the WS, 398 were positive and 11 negative according to the standard value (> 500ng/ml).
The proportion of unjustified CT angiographies (according to CPGs) was 2.3%–3.0%, using the standard DD, and 6.5%–7.0%, using the aaDD. The proportion of unjustified CT angiographies was higher when the sGS was used and lower with the sWS. Had the DD been adjusted for age, 10 and 14 unjustified CT angiographies could have been avoided, respectively. The detailed analysis of these data is shown in Tables 3 and 4.
Risk stratification, frequency of APTE and DD requested according to retrospective clinical probability scales.
| Retrospective CPS | N (%)a | APTE | p-Value | DD request |
|---|---|---|---|---|
| N (%)b | p (APTE vs. no APTE) | N (%)b | ||
| Wells Scale | ||||
| APTE unlikely | 465 (87.1) | 98 (21.1) | p=0.009 | 409 (88.0) |
| APTE likely | 69 (12.9) | 25 (36.2) | 62 (90.0) | |
| Simplified Wells Scale | ||||
| APTE unlikely | 393 (73.6) | 73 (18.6) | p<0.001 | 352 (89.6) |
| APTE likely | 141 (26.4) | 50 (35.5) | 119 (84.4) | |
| Geneva Scale | ||||
| APTE unlikely | 291 (54.5) | 45 (15.5) | p<0.001 | 263 (90.4) |
| APTE likely | 243 (45.5) | 78 (32.1) | 208 (85.6) | |
| Simplified Geneva Scale | ||||
| APTE unlikely | 302 (56.6) | 51 (16.9) | p<0.001 | 272 (90.0) |
| APTE likely | 232 (43.4) | 72 (31.0) | 199 (85.8) | |
The cut-off points for “APTE unlikely” were the same as those used by Douma et al.16: WS: <5; sWS: <2; GS: <6; sGS: <3; “APTE likely” otherwise.
APTE: acute pulmonary thromboembolism; CPS: clinical probability scale; DD: d-dimer.
Quality of management based on retrospective clinical probability scales.
| Retrospective CPS | Unjustified CT angiographies using DDa | Unjustified CT angiographies using aaDDa | Difference DD and aaDDb | Appropriate management according to CPGsc N (%) |
|---|---|---|---|---|
| Wells Scale | 11 (2.4) | 27 (6.6) | 16 (4.2) | 405 (75.8) |
| Simplified Wells Scale | 9 (2.3) | 23 (6.5) | 14 (4.2) | 365 (68.4) |
| Geneva Scale | 7 (2.4) | 18 (6.8) | 11 (4.4) | 291 (54.5) |
| Simplified Geneva Scale | 9 (3.0) | 19 (7.0) | 10 (4.0) | 296 (55.4) |
aaDD: age-adjusted d-dimer; CPG: clinical practice guideline; CPS: clinical probability scale; DD: d-dimer.
In our study, 23% of CT angiographies were positive for APTE. The WS was explicitly recorded in 81 patients (15.2%). The degree of adherence to CPGs varied depending on the CPS used, and was higher for the WS (75.8%). In addition, it was found that the DD age adjustment would have prevented between 4% and 4.4% of unnecessary CT angiographies. The frequency of APTE in our study (23%) coincides with that of Douma et al.14 and is similar to that of other studies from the European setting such as those of Lozano-Polo et al. (close to 25%),4 García-Gómez et al. (20.8%),17 Sanjuán et al. (18.23%)8 and Righini et al. (19%),18 and slightly higher than that found by Lekerika et al. (15.1%).21 However, in North American series, the frequency of positive CT angiography for APTE is lower (close to 10%),16,20,23 which has been attributed to various causes, such as an overuse of CT angiography (defensive medicine),12,24 haste during changes of shift or the demands of the patients themselves.20,25
The frequency of APTE according to risk stratification (“APTE unlikely” group’: 15.5%–21.1%; “APTE likely” group: 31.0%–36.2%) is similar to that of the European setting (“APTE unlikely”: 11.5%; “APTE likely”: 36.7%), and significantly higher compared to US series (6.5% and 32.9%, respectively).16 Furthermore, the frequency of APTE found in our study shows a slight variability between scales, corroborated by other authors. For example, Van der Pol et al.26 found a frequency of 15% and 42% (“APTE unlikely” and “APTE likely”, respectively) for the WS, while in the sWS these figures were 12% and 37%, respectively. Similarly, Gibson et al.27 found a frequency of 13% and 39% in the WS, and 11% and 36%, respectively, with the sWS. These slight divergences are consistent with our results and redound to the importance of knowing the most useful CPS at the different centres, since the predictive values of CT angiography vary according to risk7,28 and the therapeutic attitude is modified, with the administration of heparin being indicated in high-risk patients.5,21 Therefore, it is advisable to carry out prospective studies that can shed light on the most suitable CPS based on factors such as prevalence and local management.
In our series, a low record of WS was found in the patient's history (15.2%), in line with other studies.8,29 Of the cases in which the WS was included in the report, 9.8% were classified in a different category when the WS was reconstructed with data from the medical history, which can be interpreted as an indirect measure of the bias committed by the retrospective reconstruction. In this sense, the estimated bias derived from the retrospective CPS reconstruction (<10% of the cases) is not significant given the purpose of the study. However, our results should be confirmed by including all suspicions of APTE and not just the cohort of patients who underwent CT angiography.
The appropriateness of management of patients with suspected APTE was evaluated using the CPG, analysing the justified request for CT angiography based on the estimated risk according to the CPS used and the DD value.5,6,19 The appropriateness of management in our series was variable depending on the CPS used (55.4%–75.8%), and was higher with the WS. Other authors have found less adherence to the CPG. For example, Lozano-Polo et al. reported an adherence of 39.2% (according to the GS) and 53.2% (WS),4 Sanjuán et al. reported 45.8% (WS)8 and Molaee et al. reported 43.9% (WS).15 Meanwhile, the analysis of DD requests according to the WS shows that these were justified in a high number of patients with unlikely APTE in our study (88%), observing a similar trend with the other scales (89.6%–90.4%). The proportion of unjustified CT angiography was 2.3%–3.0%, using the standard DD, and 6.5%–7.0%, using the aaDD. Had the DD been adjusted for age, between 10 and 16 unjustified CT angiographies could have been avoided in our series. Several authors have pointed out the usefulness of aaDD, particularly from 75 years of age,30 and it is currently recommended in the management of APTE.6,31 There is evidence that the negative predictive value increases between 12.7%4 and 24.6%18 with respect to the standard DD value, which is why that imaging tests with negative aaDD are not recommended.12 In addition, a 7.6% increase in quality of management has been described when aaDD is combined with the sWS,4 a percentage that in our study was somewhat lower (2.8%). It should be noted again that the increase observed is with respect to the CT angiographies performed and not the suspected cases, where diagnostic yield could be even higher.
The discrepancy between the low explicit use of WS and the high percentage of cases in which management of the suspicion was appropriate according to the retrospective WS, could be fundamentally due to two reasons. On the one hand, emergency department doctors could use the WS implicitly, that is, without recording it in the electronic request or in the emergency report. Another possibility is that decision-making is based on global clinical judgement and largely coincides with what would have occurred when using the WS. Authors such as Righini et al.31 report that, although less reproducible, evaluation by expert clinicians is as reliable as the CPS. For their part, Lucassen et al.32 propose using the CPS with the highest sensitivity (sWS and GS) and clinical assessment in settings with a low prevalence of APTE. Be that as it may, CPS should not replace a good anamnesis, physical examination and synthesis of clinical information.33
In our series, the distribution of the socio-demographic variables and the comorbidity of the patients is similar to that of other studies.4,8,17,20,21 The high frequency of patients with COPD in the group without APTE could be due to the existence of common symptoms in the exacerbation of this pathology and APTE and the elevation of DD levels in both pathologies.22 The protective effect of anticoagulant treatment could explain the asymmetric distribution of anticoagulated patients found in our study. The most frequent symptoms of patients with suspected APTE also coincide with those reported by other authors4,17,21, although we found a higher frequency of patients with signs of DVT, especially in the group with APTE, compared to that described in previous studies.14,17,21
Our study has some limitations. The retrospective calculation of the WS could lead to bias,16 particularly the exclusion of cases in which there is insufficient information on the justification of CT angiography. In our study, a significant percentage of patients were excluded for this reason. Moreover, our results are not directly comparable with series in which all suspected cases of APTE were evaluated, since we only included patients who underwent CT angiography. Lastly, this is a single-centre study, so these data should be considered together with those described by other authors in other geographic locations and periods for the sake of greater representativeness.
ConclusionsOur results show that the quality of management in suspected cases of APTE varies according to the CPS used and age-adjusted DD. In addition, a low explicit use of the WS was found in the emergency department. However, this did not seem to lead to inappropriate management of patients with suspected APTE. Overall clinical judgement could offer a diagnostic yield similar to the use of CPS in our setting. However, our results must be verified in larger, ideally prospective, series.
Authorship- 1.
Responsible for the integrity of the study: AJLRB.
- 2.
Study concept: AJLRB and SMS.
- 3.
Study design: AJLRB, SMS and MCPG.
- 4.
Data collection: AJLRB and RGL.
- 5.
Data analysis and interpretation: AJLRB and MRI.
- 6.
Statistical processing: MRI.
- 7.
Literature search: MCPG, FGS and RGL.
- 8.
Drafting of the article: AJLRB and SMS.
- 9.
Critical review of the manuscript with intellectually relevant contributions: AJLRB, SMS, MCPG and FGS.
- 10.
Approval of the final version: AJLRB, SMS, MCPG, FGS and RGL.
This review received no specific grants from public agencies, the commercial sector or non-profit organisations.
Conflicts of interestThe authors declare that they have no conflicts of interest.
The authors wish to thank Drs. Antonio Medina Benítez and Luis Guzmán Álvarez, from the Radiodiagnosis Service of the Virgen de las Nieves University Hospital, for their valuable guidance, resolution of doubts and facilities offered in relation to the design and orientation of this manuscript.
Please cite this article as: Láinez-Ramos-Bossini AJ, Moreno-Suárez S, Pérez-García MC, Gálvez-López R, Garrido Sanz F, Rivera-Izquierdo M. Tromboembolismo pulmonar agudo: adecuación del manejo de pacientes según las guías de práctica clínica en el servicio de urgencias. Radiología. 2022;64:291–299.