Home mechanical ventilation (HMV) practice has changed with publication of new evidence and introduction of new technologies, and varies between countries. This study investigated current HMV use and practices in Spain and Portugal.
Methods94 healthcare professionals identified as regularly performing HMV-related activities were sent an e-mail link to an online questionnaire. The questionnaire included 40 items relating to responder demographics, non-invasive ventilation (NIV) care structure, ventilated patient profile, work habits, and potential future practice improvements.
Results66 questionnaires (70%) were returned (Spain, 36; Portugal, 30). The majority of respondents were physicians (Spain, 95%; Portugal, 63%). Overall, 83% of hospitals had a dedicated NIV unit (Spain, 100%; Portugal, 63%). The most common indication for HMV was neuromuscular disorders in Spain and obstructive diseases in Portugal. Homecare providers (HCPs) and pulmonologists were usually responsible for managing HMV; HCPs were involved more often in Portugal. Choice of ventilator was most often based on usage hours/day; the most important device features were ‘ease of use’ (Spain) and ‘adjustment range’ (Portugal). HMV monitoring practices varied between countries. Telemonitoring was used more often in Portugal (20%; vs. Spain, 3%). Follow-up frequency and practices also differed markedly between Spain and Portugal. Respondents highlighted identification of new patient groups and patient phenotyping to optimize treatment and personalize therapy as future HMV strategies.
ConclusionsImportant differences in the management of HMV were observed between two similar European countries. Better understanding of clinical practices can facilitate targeted education and training to ensure optimal management of patients using HMV.
El manejo de la ventilación mecánica domiciliaria (VMD) ha cambiado tras la publicación de información nueva y la introducción de nuevas tecnologías, y varía entre países. Este estudio investigó el uso y el manejo actuales de la VMD en España y Portugal.
MétodosNoventa y cuatro profesionales de la salud que realizaban actividades relacionadas con la VMD con regularidad recibieron un enlace mediante correo electrónico a un cuestionario en línea. El cuestionario incluyó 40 ítems relacionados con la demografía de los encuestados, la estructura de cuidados de la ventilación no invasiva (VNI), el perfil del paciente ventilado, los hábitos de trabajo y las posibles mejoras en el futuro manejo de la VMD.
ResultadosSe respondieron 66 cuestionarios (70%) (España, 36; Portugal, 30). La mayoría de los encuestados eran médicos (España, 95%; Portugal, 63%). En total, el 83% de los hospitales tenían una unidad dedicada a la VNI (España, 100%; Portugal, 63%). La indicación más frecuente de VMD fueron los trastornos neuromusculares en España y las enfermedades obstructivas en Portugal. Los prestadores de servicios médicos domiciliarios (SMD) y los neumólogos generalmente fueron los responsables del manejo de la VMD. Los SMD participaron con mayor frecuencia en Portugal. La elección del ventilador se basó con mayor frecuencia en las horas de uso/día; las características más importantes del dispositivo fueron «facilidad de uso» (en España) y «rango de ajuste» (en Portugal). El manejo del seguimiento de la VMD varió entre países. La telemonitorización se utilizó con mayor frecuencia en Portugal (20%; frente a España, 3%). La frecuencia y la forma de seguimiento también difirieron notablemente entre España y Portugal. Los encuestados destacaron la identificación de nuevos grupos de pacientes y el fenotipado de los pacientes para optimizar el tratamiento y personalizar la terapia como estrategias futuras en la VMD.
ConclusionesSe observaron diferencias importantes en el manejo de la VMD entre dos países europeos similares. Una mejor comprensión de las prácticas clínicas puede facilitar la educación y la formación específicas para garantizar un manejo óptimo de los pacientes que utilizan VMD.
Home mechanical ventilation (HMV) has been used to treat chronic hypercapnic respiratory failure secondary to obstructive and restrictive diseases for the last 20 years.1 Use of HMV has increased markedly worldwide over the last 25 years, but utilization rates vary widely between centers2 and countries.3 The first large-scale evaluation of home NIV usage in Europe, the EuroVent survey,3 was published almost 15 years ago, and showed that management of HMV across a range of indications varied widely between geographical areas, particularly with respect to duration of ventilation, ventilatory modes, type of ventilators, and pathologies treated. Other studies also showed a differences in clinical practice in non-invasive ventilation (NIV) for the management of acute respiratory failure.4 In some diseases, variability in NIV practice is very high,4 despite the availability of national5 and international6,7 guidelines and recommendations. Nevertheless, there are a number of important topics that have not previously been evaluated, including the differing healthcare professionals (HCPs) involved in the care of patients undergoing HMV, monitoring protocols, healthcare infrastructure, and the use and impact of new technology such as built-in monitoring software, telemonitoring and new ‘intelligent’ ventilation modes. As a result, there is a need for survey data to determine the real-world application of the latest HMV technologies and differences in clinical practice between countries. This could highlight potential limitations in training and technology availability between similar countries.
The Iberian Respiratory Care (iCARE) program was initiated in 2013 to facilitate better knowledge of HMV through the collaboration of a group of experts and different activities, and generate consensus on HMV practices through debate. As part of the iCARE program, this study investigated and compared current management and usage of HMV in Spain and Portugal.
Material and methodsStudy designThis prospective study was conducted in Spain and Portugal. On 17 September 2015 an e-mail was sent directly to healthcare professionals identified as regularly performing NIV-related activities in their practice. The e-mail included a link to an online questionnaire that healthcare professionals were asked to complete. A reminder e-mail was sent on 24 September 2015, and the last date for questionnaire completion was 15 January 2016. Management of all legal documents, the questionnaire platform, project and anonymized data analyses were managed by an independent third party (MK Media).
QuestionnaireThe questionnaire was developed by an Advisory Board including five experts in the field (three pulmonologists from Spain, one pulmonologist and one physiotherapist from Portugal). These experts defined the areas of interest and developed questions based on currently available literature and daily clinical practice experience. It included 40 separate items and was designed to gather information about the following: responder demographics; support for HMV; availability of a pediatric HMV program; existence of a specific NIV unit; timing and location of NIV initiation; personnel responsible for initiation of NIV; location of NIV delivery; procedure for NIV titration; control, management and monitoring of HMV; procedure for changing NIV settings; availability of home care services; type of ventilators available and ventilator ownership. Healthcare professionals could complete the questionnaire on their computer or smart phone.
Statistical analysisQuestionnaire responses were collated by MK Media and analyzed using descriptive statistics (frequency of responses were reported as a percentage of total responses, overall and for each country). Support for data analysis was provided by IQVIA.
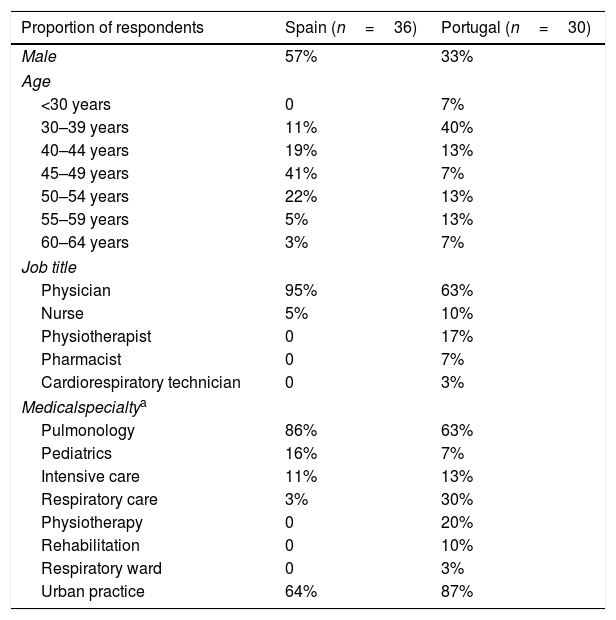
ResultsRespondentsA total of 94 questionnaires were sent out, and 66 were returned (36 from Spain and 30 from Portugal); the response rate was 70%. The majority of respondents from both countries were physicians, but there was a wider variety of jobs and specialties among those from Portugal (Table 1). The mean number of HMV patients seen per week was 14.24 (13.51 in Spain and 15.12 in Portugal).
Characteristics of questionnaire respondents by country of origin.
| Proportion of respondents | Spain (n=36) | Portugal (n=30) |
|---|---|---|
| Male | 57% | 33% |
| Age | ||
| <30 years | 0 | 7% |
| 30–39 years | 11% | 40% |
| 40–44 years | 19% | 13% |
| 45–49 years | 41% | 7% |
| 50–54 years | 22% | 13% |
| 55–59 years | 5% | 13% |
| 60–64 years | 3% | 7% |
| Job title | ||
| Physician | 95% | 63% |
| Nurse | 5% | 10% |
| Physiotherapist | 0 | 17% |
| Pharmacist | 0 | 7% |
| Cardiorespiratory technician | 0 | 3% |
| Medicalspecialtya | ||
| Pulmonology | 86% | 63% |
| Pediatrics | 16% | 7% |
| Intensive care | 11% | 13% |
| Respiratory care | 3% | 30% |
| Physiotherapy | 0 | 20% |
| Rehabilitation | 0 | 10% |
| Respiratory ward | 0 | 3% |
| Urban practice | 64% | 87% |
The majority of workplaces in both countries offered an HMV assistance structure with adequate resources, although access was better in Spain (97% in Spain, 83% in Portugal). Overall, respondents noted that 53% of hospitals had a dedicated HMV program (58% in Spain, 47% in Portugal), and 83% of hospitals had a specific HMV unit (100% in Spain, 63% in Portugal). Approximately half of the hospitals represented by respondents had a pediatric HMV program.
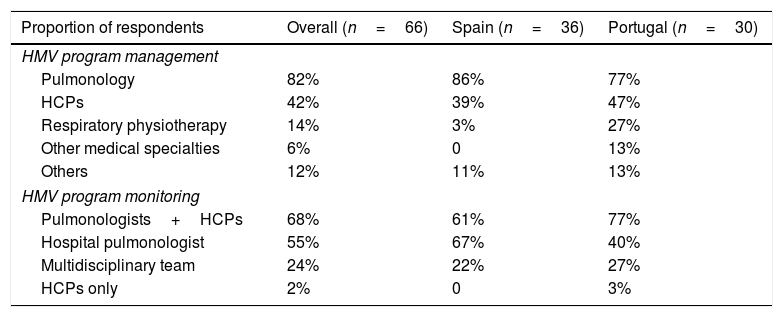
Management and monitoring of HMV programsPulmonologists were the most common managers of HMV in both Spain and Portugal, followed by home care providers (HCPs), who were involved more often in Portugal than in Spain (Table 2). Overall and in Spain, monitoring of HMV programs was most often done by pulmonologists coordinated with HCPs, followed by a hospital pulmonologist, whereas the pulmonologist/HCP collaboration was most common in Portugal (Table 2).
Management and monitoring of home mechanical ventilation (HMV) programs.
| Proportion of respondents | Overall (n=66) | Spain (n=36) | Portugal (n=30) |
|---|---|---|---|
| HMV program management | |||
| Pulmonology | 82% | 86% | 77% |
| HCPs | 42% | 39% | 47% |
| Respiratory physiotherapy | 14% | 3% | 27% |
| Other medical specialties | 6% | 0 | 13% |
| Others | 12% | 11% | 13% |
| HMV program monitoring | |||
| Pulmonologists+HCPs | 68% | 61% | 77% |
| Hospital pulmonologist | 55% | 67% | 40% |
| Multidisciplinary team | 24% | 22% | 27% |
| HCPs only | 2% | 0 | 3% |
HCPs, home care providers.
There was a wide range of devices available in both Spain and Portugal, including NIV and invasive home ventilators with battery (94% and 90%), home ventilators without a battery (78% and 83%), life support and hybrid ventilators (75% and 83%), and vital support ventilators with NIV and invasive capabilities (72% and 83%). Three of the four types of devices were most likely to be leased (53–77%) or a mix of leasing and workplace property (13–25%), but leasing was more common in Spain. Overall, life support ventilators with NIV and invasive modes were more likely to be workplace property (37%) or workplace property or leased (37%), with no marked between-country differences.
Choice of device for HMV was primarily based on a patient's ventilatory dependence (number of hours of ventilation required per day; 73% of respondents), followed by the respiratory disease indication (62%), clinical situation (52%) and patient tolerance of NIV (42%), with no differences between the two countries. ‘Ease of use’ was rated as the most important feature of an HMV system by respondents from Spain, whereas this was ranked third by respondents from Portugal, who said that range of adjustment was the most important feature of an HMV device. The second-rated feature in Spain was versatility, and in Portugal it was monitoring possibilities. Respondents from both countries ranked telemonitoring last of their top nine features for an HMV device.
The majority of respondents used an oronasal mask (41%) or nasal mask (37%) as the interface for HMV delivery. An oronasal mask was more popular in Portugal (45%) than in Spain, whereas a nasal mask was used more often in Spain (41% vs. 31% in Portugal). Mouthpieces were used infrequently (2% overall, 1% in Spain and 3% in Portugal). Spontaneous-timed (ST) was the most commonly used ventilation mode (76% overall, 81% in Spain, 70% in Portugal), followed by volume-assured pressure support (VAPS; 33% overall and in each country). Use of pressure-assisted controlled (PAC) ventilation was more common in Spain (19%) than in Portugal (3%).
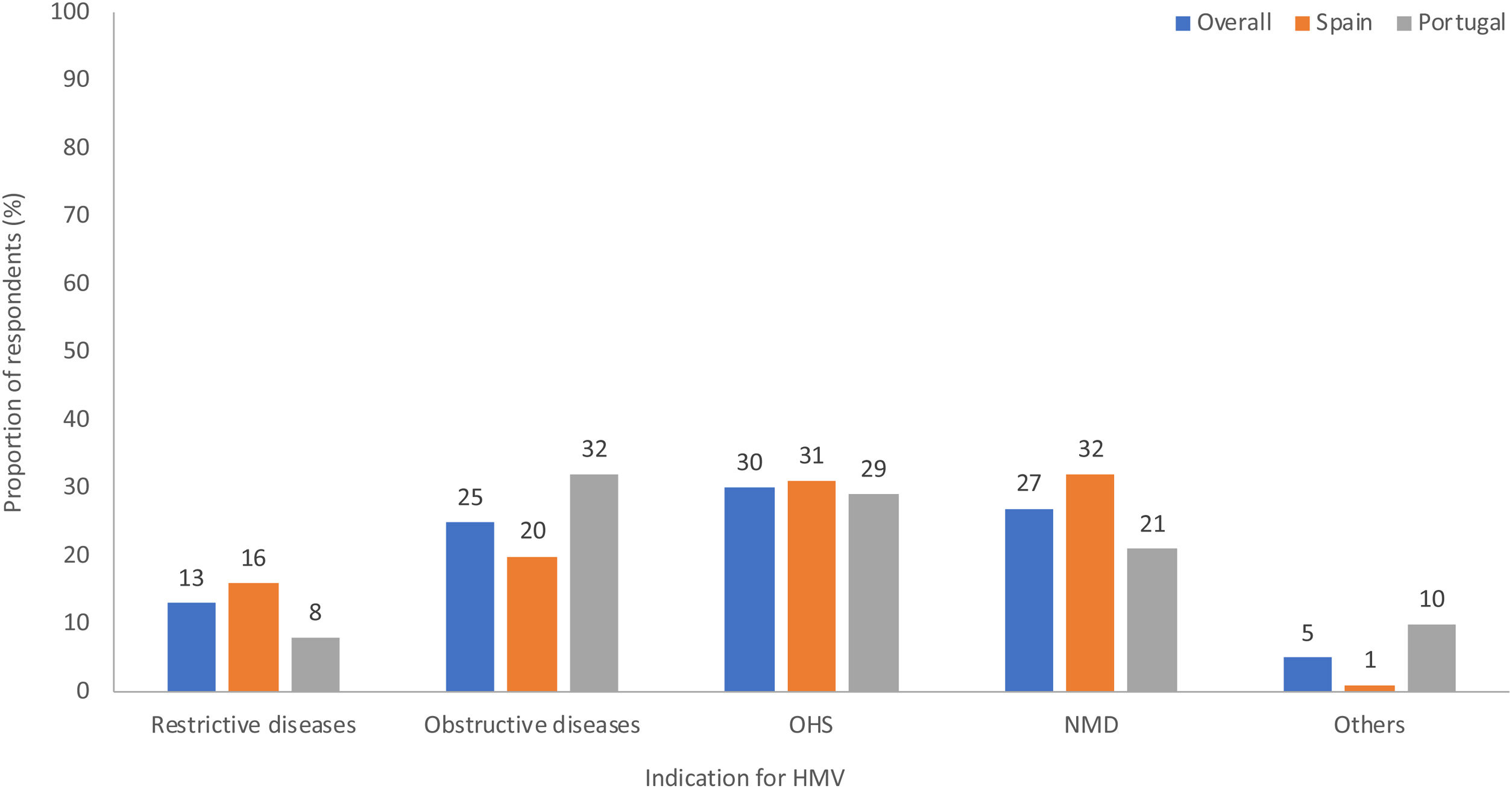
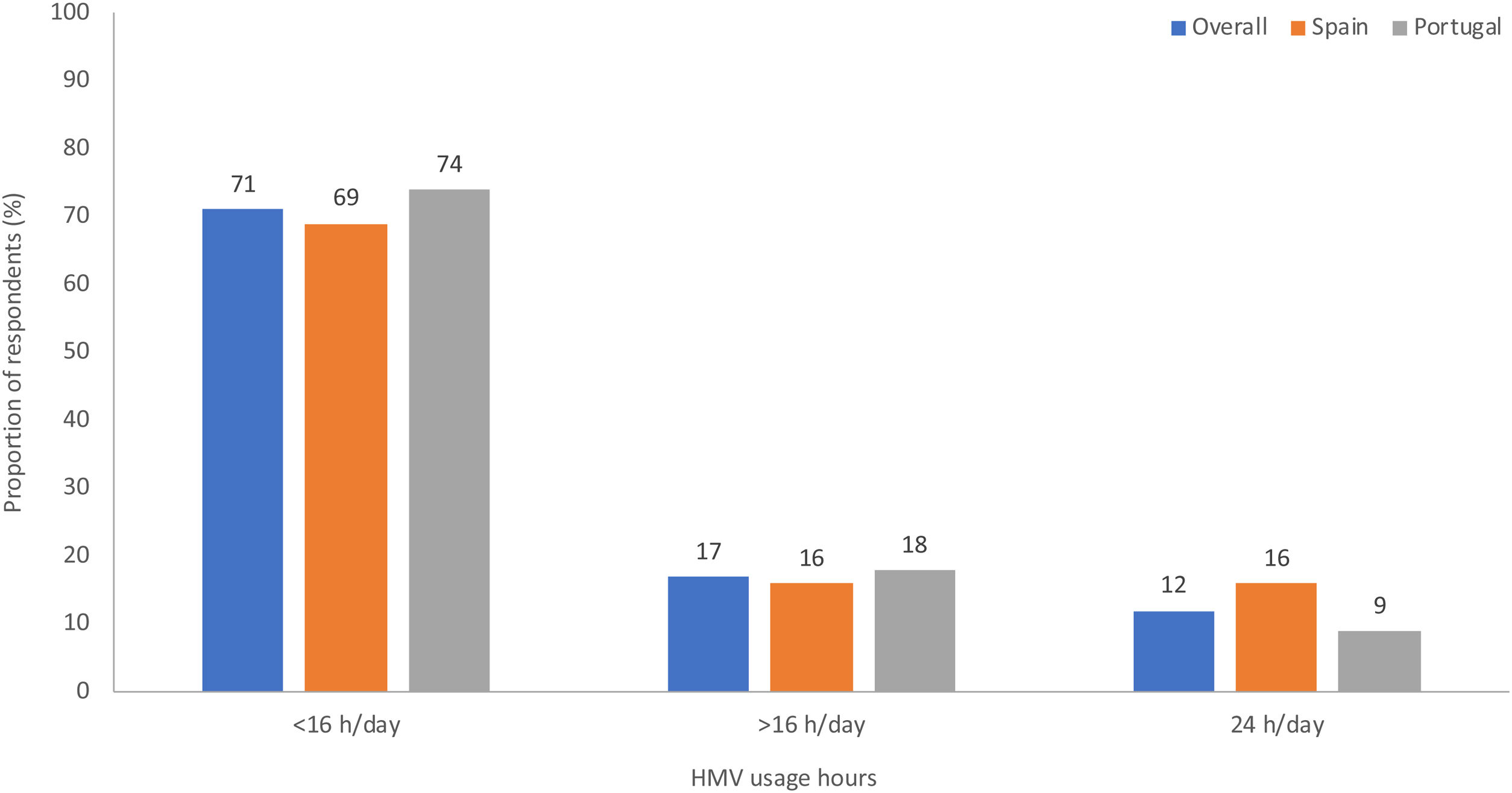
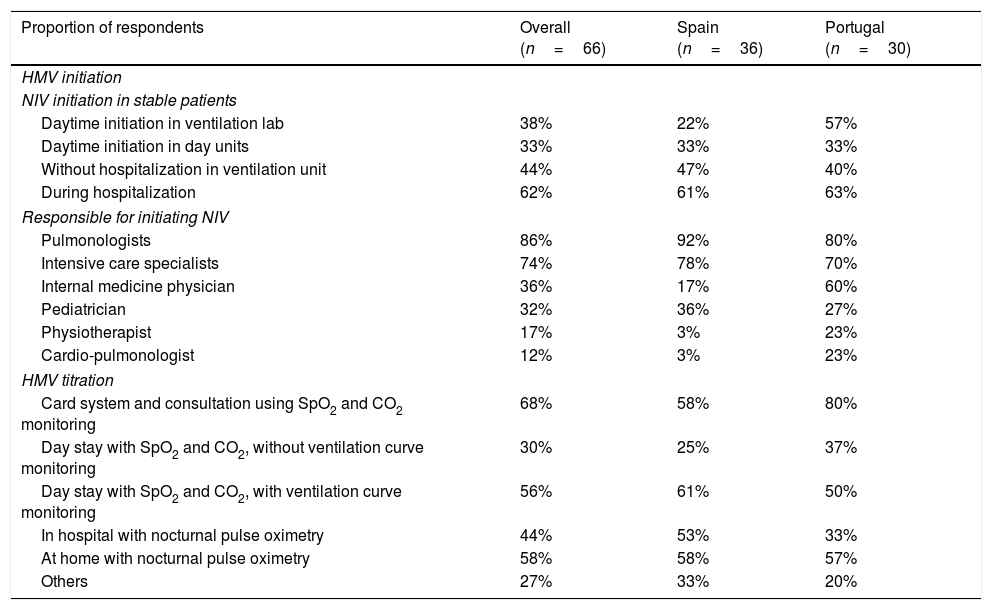
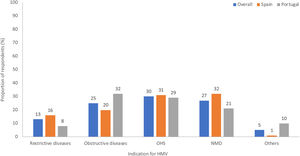
HMV indications and usageObstructive lung diseases, obesity hypoventilation syndrome (OHS) and neuromuscular diseases (NMD) were the most common indications for HMV. Use of HMV for NMD occurred more often in Spain than in Portugal, whereas obstructive lung diseases were the main indication for HMV in Portugal (Fig. 1). The majority of patients in both countries used NIV for <16h/day (Fig. 2).
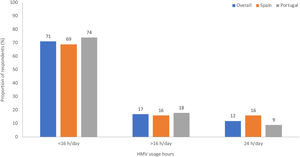
Daytime initiation of NIV and adjustment of ventilatory parameters in the ventilation lab was much more common in Portugal (57%) versus Spain (22%); other approaches to NIV initiation in stable patients were similar between countries (Table 3). In both countries, pulmonologists or intensive care specialists were the most likely to be responsible for initiating NIV (Table 3). In Portugal, internal medicine physicians also played an important role in NIV initiation (Table 3). There were a variety of approaches to NIV titration; the most common approach in Portugal was a card download system and consultation using oxygen saturation (SpO2) and carbon dioxide (CO2) monitoring, whereas day stay with SpO2-CO2 and direct monitoring of ventilation waves was most common in Spain (Table 3).
Initiation and titration of home mechanical ventilation (HMV) programs.
| Proportion of respondents | Overall (n=66) | Spain (n=36) | Portugal (n=30) |
|---|---|---|---|
| HMV initiation | |||
| NIV initiation in stable patients | |||
| Daytime initiation in ventilation lab | 38% | 22% | 57% |
| Daytime initiation in day units | 33% | 33% | 33% |
| Without hospitalization in ventilation unit | 44% | 47% | 40% |
| During hospitalization | 62% | 61% | 63% |
| Responsible for initiating NIV | |||
| Pulmonologists | 86% | 92% | 80% |
| Intensive care specialists | 74% | 78% | 70% |
| Internal medicine physician | 36% | 17% | 60% |
| Pediatrician | 32% | 36% | 27% |
| Physiotherapist | 17% | 3% | 23% |
| Cardio-pulmonologist | 12% | 3% | 23% |
| HMV titration | |||
| Card system and consultation using SpO2 and CO2 monitoring | 68% | 58% | 80% |
| Day stay with SpO2 and CO2, without ventilation curve monitoring | 30% | 25% | 37% |
| Day stay with SpO2 and CO2, with ventilation curve monitoring | 56% | 61% | 50% |
| In hospital with nocturnal pulse oximetry | 44% | 53% | 33% |
| At home with nocturnal pulse oximetry | 58% | 58% | 57% |
| Others | 27% | 33% | 20% |
CO2, carbon dioxide; SpO2, oxygen saturation.
Monitoring of HMV therapy differed between the two countries. In Portugal, HMV was most often managed using the card download system sent by HCPs to the hospital specialist (90%) whereas use of this system was only reported by 39% of respondents from Spain. Monitoring in Spain was usually conducted in the chronic ventilation unit or HMV-specific consultancy (97%, vs. 70% in Portugal). Use of telemonitoring was more common in Portugal (20%) versus Spain (3%). Just over half of all respondents from both countries informed patients about HMV monitoring results (58% in Spain, 53% in Portugal).
There were two main approaches to changing HMV parameters; requesting changes from the HCP was most common in Portugal (67%), whereas change in Spain were more likely to be undertaken through external consultancy or day stay by a physician or therapist (75%). Remote changes using telemonitoring were used by 13% of respondents from Portugal and only 3% from Spain.
There was a wide range of patterns for follow-up of patients receiving long-term HMV, from every week (6% in Spain, 13% in Portugal) to every 6 months (8% in Spain, 3% in Portugal). Respondents also said that follow-up frequency was sometimes tailored to the patient, clinical situation and/or response, particularly in Spain. Follow-up evaluations were most likely to include SpO2 (83% in Spain, 70% in Portugal) and patient comfort (75% in Spain, 70% in Portugal), followed by ventilator software (64% and 53%) and arterial blood gases (61% and 53%).
Future useMost respondents (72%) did not perceive the need to improve knowledge about how NIV works in different patients, and 64% said that they saw the role of NIV, especially HMV, increasing in the future. Many (59%) also felt that the availability of interfaces permitting well-fitting ventilation in the majority of patients would reduce the need for intubation. A slightly higher proportion (70%) thought that device software will be an important tool for patient monitoring. New patient groups to benefit from NIV and patient phenotyping to optimize treatment and provided personalized therapy were identified as future NIV strategies. Better and more versatile equipment were cited as being the most important factors for promoting use of NIV during exercise and daily activities; specifically, devices need to be portable and light, with greater autonomy. The most important role for telemonitoring was seen to be evaluating patient-ventilator interactions.
DiscussionDespite the increasing use of HMV there is a lack recent data on real-life use of this technology. To the best of our knowledge, this is the first survey that provides a detailed analysis of therapeutic habits in HMV in the context of up-to-date technology in two countries with a similar socio-health context. The findings revealed several differences between Spain and Portugal in how HMV was used and managed. These mainly related to the main indication for HMV, the level of involvement of HCPs, practices for initiation and monitoring of NIV, and approach to patient follow-up.
The response rate to our questionnaire was quite good, at 70%, and was similar to that in other surveys.3,4 Our findings were also consistent with those of the EuroVent survey, which showed several differences between European countries in the number of centers per user, profile of the institution, duration of ventilation, ventilators used, and the pathologies submitted to NIV.4 Given the geographic and cultural similarities between Spain and Portugal, it might be expected that differences in practice would be less, but this was not the case. One of the most notable differences between the two countries was in the profile of the HCP in charge of monitoring patients using HMV. In Portugal, physiotherapists played a prominent role while in Spain, this role was taken almost exclusively by pulmonologists. This is most likely due to the historical role of respiratory physiotherapists and respiratory function/sleep technologists in the management of patients using HMV in Portugal.8 There are a number of other factors that could potentially contribute to between-country differences in HMV practice. Although generally similar, subtle variations in the healthcare systems and professional profiles between Spain and Portugal might have driven practice decisions. Practices may also vary by region within countries (e.g. rural versus urban), and any differences between countries in the proportions of patients managed in more remote areas could potentially influence our findings.
The results of another recently published survey showed that COPD was a common indication for home NIV, but prescription rates varied between countries.9 In that survey, which did not include Portugal, Spain had one of the lowest rates of home NIV prescription for COPD (approximately 20% of all HMV prescriptions were for this indication). This was similar to our findings where the most common indications for NIV in Spain were NMD (32% of respondents) and OHS (31%), with obstructive diseases (including COPD) less commonly reported as an indication for HMV (20% of respondents). A survey of all Madrid area public hospitals found that OHS was the most common pathology for which home NIV was prescribed, although there was variation between centers.10 This was consistent with our data from Spanish respondents. In contrast, respondents from Portugal in our survey cited obstructive diseases as the most common HMV indication (32%). This is consistent with data from the HMV group of the Portuguese Respiratory Society showing that most patients receiving HMV had obstructive lung diseases.8 At the time our survey was conducted, physicians should have been aware of randomized clinical trial data showing significant reductions in mortality and hospital readmission with HMV in stable COPD patients with chronic hypercapnia.11,12 Therefore, lack of evidence should not have been a valid reason for non-use of HMV in this patient group by our respondents.
Access to new NIV technology, such as the built-in respiratory software analysis,13,14 was a well-accepted and widespread clinical practice in both countries according to our survey. However, the use and interest in intelligent modes of ventilation15 was very low. Classic modes of ventilation still appeared to be preferred by HCPs in both countries.
Overall rates of telemonitoring use in our survey were very low. This was particularly the case in Spain where use of this technology was almost non-existent. Crimi et al. also identified low usage of telemedicine solutions for ongoing monitoring of HMV in Europe (reported by only 5% of respondents in their survey).9 Nevertheless, over the last 4 years telemonitoring has been progressively adopted into daily practice routines, which was exponentially accelerated over last year due to the Covid19 pandemic in Spain, but also in Portugal. As a consequence of this evolution and practice change, the Spanish Society of Pulmonology and Thoracic Surgery published a position paper on telemedicine use for sleep-disordered breathing and mechanical ventilation establishing recommendation from diagnostics to patient monitoring which reflect significant changes in clinical practice for the management of HMV in Spain, that are not reflected in our study. In this document, for example, the use of telemedicine is recommended in all patient with HMV particularly in the beginning of treatment or according to medical criteria, surely, still outside the reality of care.16
Education to improve physician awareness and knowledge of telemonitoring in the setting of HMV might help to improve uptake of this technology, contributing to improvement in clinical practice.16,17 Respondents did identify improvements in HMV equipment and technology as one of their hopes for the future. Personalized medicine, rather than just the underlying pathology, should guide use of HMV to manage patients with ventilatory failure.18
With improvements in technology over time and the growth of HMV as a valid treatment option for patients with a variety of underlying conditions, there is an important need to increase physician competency in this field to facilitate provision of ventilator equipment and consumables, ongoing management of ventilator settings, and careful risk management. The competence in sleep medicine although it is advisable,19 it is about to establish its real utility in the adaptation to the mechanical ventilation home.20 In addition, the requirement to adequately train caregivers and their patients about HMV should not be underestimated.
A number of limitations need to be taken into account when interpreting the results of our study. The data are based on reports from healthcare professionals rather than actual clinical data and may therefore be subject to bias (e.g. recall bias). In addition, the inclusion of healthcare professionals with experience in NIV is a biased sample but this is the most relevant group for determining NIV practice. The questionnaire used was developed for this study only and has not been widely validated, therefore the findings are descriptive only. In addition, the results are only applicable to the two countries in which they were obtained and cannot be generalized more widely. Furthermore, the majority of respondents to our survey were from urban areas, limiting the applicability of the findings to rural settings in the countries studied. Use of HMV patient databases might be an alternative approach to help overcome this issue.21
ConclusionsThe present study highlighted significant differences in clinical practice for the management of HMV between Spain and Portugal, which are most likely due to different training processes, and differences in administrative and health infrastructure. Increasing use of HMV will require the implementation of appropriate training and guidelines to ensure optimization and standardization of practices, both between centers and between countries, so that the between-country differences in practices seen in our study are minimized. In addition, better understanding of NIV-related clinical routines should help facilitate targeted education and training to ensure optimal management of patients using HMV.
Funding and role of the funding sourceThis work was funded by ResMed. Representatives and scientists from the ResMed participated in the study including design, data collation, data analysis, and critical review of the paper.
Conflict of interestsA Antóna, S Díaz Lobatob, MJ Guimarãesc, ML Alonso-Álvarezd and M Gonçalvesf report grants from the ResMed iCare program in 2015.
S. Correia is an employee of ResMed.
Medical writing assistance was provided by Nicola Ryan, independent medical writer, funded by ResMed.