We recently described the short-term analgesic effects of an intrathecal baclofen bolus on neuropathic pain in patients with spinal cord injury.1 Other studies report significant, sustained relief of neuropathic pain secondary to traumatic or metabolic lesions to peripheral nerves with 3 monthly boluses of 50 µg intrathecal baclofen.2 Some researchers have described the long-term benefits of intrathecal baclofen for complex regional pain syndrome,3 postherpetic neuralgia,4 and chronic pain of different aetiologies.5 Zuniga et al.5 report that intrathecal baclofen may relieve chronic pain of central or peripheral origin, and Loubser and Akman6 describe the analgesic effects of the drug on chronic musculoskeletal pain associated with spasticity but not on neuropathic pain.
Evidence of the long-term analgesic effects of an intrathecal baclofen pump is based on case series exclusively.4–6 We present the long-term effects of intrathecal baclofen on neuropathic pain in 3 patients with spinal cord injury and severe spasticity who were administered a baclofen bolus test1 and subsequently underwent pump implantation (see online Supplementary Material). We used the Neuropathic Pain Symptoms Inventory (NPSI) to evaluate the severity of the different types of neuropathic pain and the Brief Pain Inventory (BPI) to study patient perception of the severity of neuropathic pain and its impact on activities of daily living.
Clinical casesPatient 1Our first patient was a 55-year-old man with chronic complete spinal cord injury (ASIA Impairment Scale grade A) (Table 1) who reported spontaneous pain and allodynia.
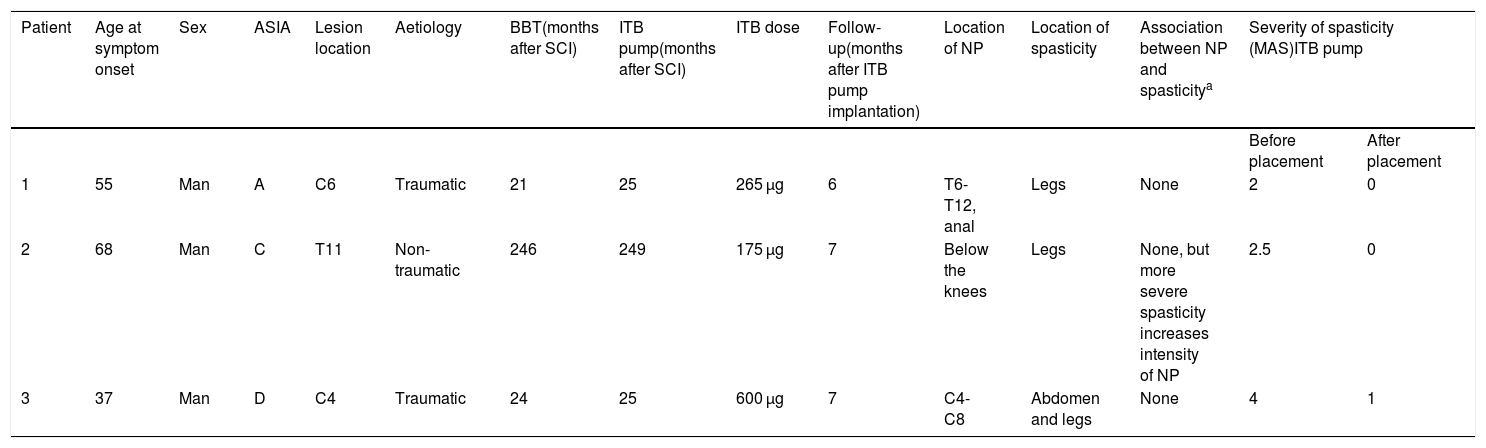
Demographic and clinical characteristics of our 3 patients, and characteristics of neuropathic pain and spasticity.
| Patient | Age at symptom onset | Sex | ASIA | Lesion location | Aetiology | BBT(months after SCI) | ITB pump(months after SCI) | ITB dose | Follow-up(months after ITB pump implantation) | Location of NP | Location of spasticity | Association between NP and spasticitya | Severity of spasticity (MAS)ITB pump | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before placement | After placement | |||||||||||||
| 1 | 55 | Man | A | C6 | Traumatic | 21 | 25 | 265 µg | 6 | T6-T12, anal | Legs | None | 2 | 0 |
| 2 | 68 | Man | C | T11 | Non-traumatic | 246 | 249 | 175 µg | 7 | Below the knees | Legs | None, but more severe spasticity increases intensity of NP | 2.5 | 0 |
| 3 | 37 | Man | D | C4 | Traumatic | 24 | 25 | 600 µg | 7 | C4-C8 | Abdomen and legs | None | 4 | 1 |
ASIA: American Spinal Injury Association Impairment Scale score; BBT: baclofen bolus test; ITB: intrathecal baclofen; MAS: Modified Ashworth scale; NP: neuropathic pain; SCI: spinal cord injury.
At 6 months, after implantation of an intrathecal baclofen pump, neuropathic pain improved by 70% and BPI scores decreased from 78 to 17 points.
Patient 2Our second patient was a 68-year-old man with chronic incomplete spinal cord injury (ASIA Impairment Scale grade C) who presented spontaneous, paroxysmal pain and dysaesthesia. The baclofen bolus test predicted a 100% decrease in neuropathic pain. At 7 months after pump implantation, neuropathic pain had decreased by 60% (BPI).
Patient 3Our third patient was a 37-year-old man with chronic incomplete spinal cord injury (ASIA Impairment Scale grade D) who presented spontaneous, paroxysmal pain, allodynia, and dysaesthesia. During the baclofen bolus test, the patient was administered physiological saline solution (placebo) and no improvements were observed in neuropathic pain. After implantation of the intrathecal baclofen pump, neuropathic pain improved by 80%.
Continuous infusion of intrathecal baclofen in 3 patients with spinal cord injury had a long-term analgesic effect on all types of neuropathic pain and substantially decreased the impact of the disease on activities of daily living; these effects persisted for several months. In addition to the benefits of this treatment for spasticity, our results suggest that the analgesic effects of intrathecal baclofen bolus treatment may be considered an indicator of positive response of neuropathic pain to an intrathecal baclofen pump. Previous studies suggest that decreased GABAergic tone in patients with spinal cord injury leads to long-term potentiation in nociceptive pathways,7 which may in turn promote the transmission of nociceptive stimuli. However, we cannot rule out that intrathecal baclofen may have an inhibitory effect in other areas of the central nervous system.8 In patients with spinal cord injury, an intrathecal baclofen bolus was found to induce changes in quantitative sensory tests and pain-related evoked potentials,9 which may point to transient compensation of reduced GABAergic inhibition. Considering that continuous infusion of intrathecal baclofen is currently limited to patients with severe spasticity who do not respond to conventional antispastic treatment, no specific recommendations for pain management have been issued to date.10
One of the limitations of our study is the lack of a control group or condition (eg, implanting a pump to administer saline solution instead of baclofen, or stopping the pump without informing patients), for obvious ethical reasons. In conclusion, our study shows significant, lasting improvements in neuropathic pain after implantation of an intrathecal baclofen pump in patients with spinal cord injury. Physicians should take into account the possible long-term analgesic effects of intrathecal baclofen and evaluate the need to adjust treatment in patients with refractory neuropathic pain. Randomised, controlled clinical trials including larger samples of patients with spinal cord injury should be conducted to expand our knowledge about the analgesic effects of intrathecal baclofen.
Conflict of interestThe authors do not have any conflict of interest.
Supplementary materialSupplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.nrl.2019.09.009.
Supplementary dataThe following is Supplementary data to this article:
Please cite this article as: Kumru H, Albu S, Kofler M, Vidal J. Efecto analgésico del baclofeno intratecal a largo plazo sobre el dolor neuropático en pacientes con lesión medular. Neurología. 2020;35:679–681.