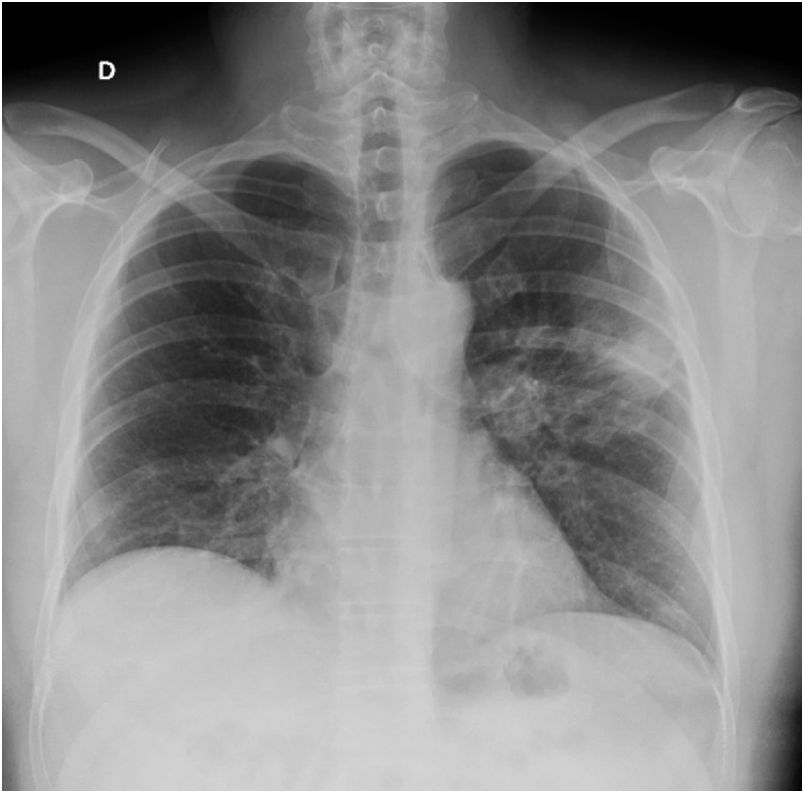
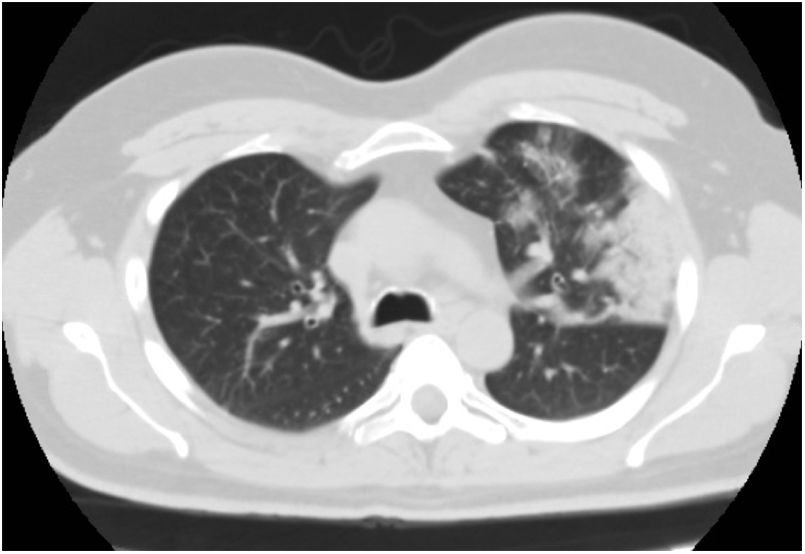
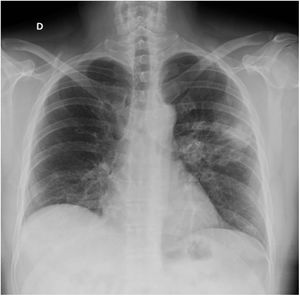
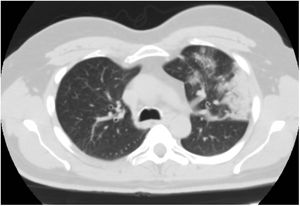
A novel coronavirus, SARS-CoV-2, was detected in Wuhan, China, in December 2019 and the associated disease, known as COVID-19, has quickly become a pandemic. Several reports suggest that SARS-CoV-2 may infect the central nervous system, causing neurological alterations.1 Some authors have reported cases of encephalopathy,2 acute necrotising haemorrhagic encephalopathy,3 meningoencephalitis,4 headache, myalgia, neuropathic pain, hyposmia, ageusia, ataxia, epileptic seizures, and cerebrovascular events.5 To our knowledge, no peripheral nervous system alterations other than those mentioned above have been reported to date. We present the case of a 48-year-old man with paranoid schizophrenia, under treatment with aripiprazole; inverse psoriasis; and no other relevant medical history. The patient came to the emergency department due to a 5-day history of binocular diplopia, which was more marked at long distance and with lateral gaze, with a tendency to improvement. He also reported presenting high fever, dry cough, dyspnoea, and myalgia 15 days previously; he self-isolated in view of the current epidemiological situation. Fever resolved 5 days prior to the consultation, but diplopia appeared; the remaining symptoms had improved. The physical examination revealed expiratory wheezing. The neurological examination revealed isochoric, reactive pupils; normal confrontation visual field test results; horizontal diplopia with gaze to the right; and no observable eye movement restriction. Results were normal for all other areas. A blood analysis detected high levels of acute-phase reactants (fibrinogen 885mg/dL, CRP 8.8mg/dL, d-dimer 1095ng/mL). The patient was admitted to the internal medicine department due to suspected COVID-19. PCR testing was negative for SARS-CoV-2 in nasopharyngeal exudate but positive in sputum. A chest radiography showed right lower lobe opacification and lingula consolidation; these findings were confirmed by a chest CT scan and linked to the infection (Figs. 1 and 2). More detailed analyses showed normal kidney, liver, and thyroid function; vitamin B12 and folate levels within normal ranges; and normal lipid profile, blood count, and coagulation profile. Autoimmune tests yielded negative results except for antinuclear antibodies (1:320, homogeneous pattern) and acetylcholine receptor antibodies (1.10nmol/L; positive: >0.20nmol/L). Serology tests were negative. Diplopia resolved the day after hospital admission. A head CT scan showed no space-occupying lesions, vascular alterations, or any other abnormal findings. The patient's general condition improved and he was discharged 2 days after admission; he was instructed to continue treatment with hydroxychloroquine and azithromycin. Our patient developed diplopia associated with acetylcholine receptor antibodies in the context of microbiologically confirmed SARS-CoV-2 infection; symptoms resolved completely within days. He had no cardiovascular risk factors and neuroimaging studies revealed no vascular or space-occupying lesions that may otherwise explain his symptoms. We suggest 2 possible explanations for our case. First, the patient had latent myasthenia gravis, which was precipitated by SARS-CoV-2 infection; and second, SARS-CoV-2 infection was the main cause of the patient's symptoms, triggering an autoimmune response, with tropism to the neuromuscular junction as a result of molecular mimicry.6 Clinical and serological follow-up of our patient is necessary to evaluate his progression and detect any changes. Patients with COVID-19 must be screened for symptoms of muscle fatigability. This information is essential to direct further testing, with a view to determining whether myasthenia gravis is a possible complication of SARS-CoV-2 infection. This may open new lines of research into COVID-19.
Please cite this article as: Pérez Álvarez ÁI, Suárez Cuervo C, Fernández Menéndez S. Infección por SARS-CoV-2 asociada a diplopía y anticuerpos antirreceptor de acetilcolina. Neurología. 2020;35:264–265.