In the last 15 years, considerable improvements have been made in acute stroke care in Guipuzkoa, including the implementation of a centralised care model at Hospital Universitario Donostia (HUD), improved coordination between professionals, early detection campaigns, new treatments, a stroke unit, and specific rehabilitation. The aim of this work is to describe the results of a reference hospital (HUD) in a centralised care model.
Material and methodsWe performed a retrospective observational study of a sample of patients discharged between August and December 2015 from the HUD with a diagnosis of acute stroke (ICD-9-CM codes 430-436, except 433.10). We review patients’ baseline characteristics, acute-phase care, and functional outcomes and mortality at discharge and at one year.
Results and discussionWe identified 536 patients, with a mean age of 73.6 years and a high comorbidity rate. Ischaemic stroke accounted for 64.8% of patients, followed by haemorrhagic stroke (20%) and transient ischaemic attack (14.8%). A total of 53% of patients were attended in < 6 hours, with code stroke being activated in 37.1%; 52.2% of patients were admitted to the stroke unit. Intravenous therapy was administered to 8.3% of patients with ischaemic stroke, and 9.5% underwent mechanical thrombectomy. Surgery was performed in 12.1% patients with haemorrhagic stroke. Rehabilitation was started at hospital in 56% of patients, and 39.6% continued with this treatment at discharge. Mortality was 13.8% at discharge and 25.9% at one year (ischaemic stroke, 25.3%; haemorrhagic stroke, 47.5%); these figures are lower than those previously reported in Guipuzkoa. At one year, 62.5% of patients had a Barthel Index score of 95-100, and 50% a modified Rankin Scale score of 0-2.
ConclusionsAfter the strategic changes implemented in acute stroke care in Guipuzkoa, including the centralisation of the acute stroke care model, mortality rates at discharge and at one year are lower in 2015 than the previously reported rates, with similar rates of independence. These results are consistent with those published by other Spanish and European centres.
En los últimos 15 años se han introducido importantes mejoras en la atención de la enfermedad cerebrovascular aguda (ECVA) en Guipúzcoa que incluyen la implementación de un modelo centralizado en el Hospital Universitario Donostia (HUD), una mejor coordinación entre profesionales, campañas para su detección precoz, nuevos tratamientos, Unidad de Ictus y una rehabilitación específica. El objetivo de este trabajo es describir los resultados de un hospital de referencia (HUD) en un modelo de atención centralizado.
Material y métodosEstudio observacional retrospectivo de una muestra de pacientes dados de alta en el periodo de agosto-diciembre del año 2015 del HUD con diagnóstico de ECVA (CIE-9-MC-430-436 excepto 43310). Revisión de las características basales, atención en fase aguda, y resultados funcionales y de mortalidad al alta y al año.
Resultados y DiscusiónSe incluyeron 536 pacientes cuya media de edad fue de 73,6 años y cuya comorbilidad era elevada. El ictus isquémico supuso el 64,8% de las altas, seguido de la ECVA hemorrágica (20%) y del accidente isquémico transitorio (AIT) (14,8%). Se atendió en < 6 h a un 53% de pacientes, activándose el “código ictus” en un 37,1%. Un 52,2% ingresaron en la Unidad de Ictus. Un 11,34% de los pacientes con ictus isquémico recibió terapia intravenosa y un 9,5% trombectomia mecánica. Un 12,1% de los pacientes con ECVA hemorrágica fue intervenido quirúrgicamente. El 56% inició rehabilitación en el hospital y un 39,6% la mantuvo al alta. La mortalidad al alta fue de un 13,8% y al año de un 25,9% (ictus isquémico: 25,3% y ECVA hemorrágica: 47,5%), menor a la descrita previamente en Guipúzcoa. Al año un 62,5% de pacientes tenían un Índice de Barthel (IB) 95-100, y un 50% una puntuación en escala de Rankin modificada (mRS) 0-2.
ConclusionesTras las modificaciones estratégicas introducidas en la atención a la ECVA en Guipúzcoa, incluyendo la centralización del modelo de atención, la mortalidad al alta y anual en 2015 es menor a la descrita previamente, con tasas de autonomía similares. Estos resultados se encuentran en línea con los resultados publicados por parte de otros centros españoles y europeos.
According to the World Health Organization, acute stroke (AS) is the second leading cause of death and the first cause of disability in the adult population in Western countries.1 Furthermore, it is an important risk factor for disability in adults, as most patients are left with sequelae; 40% of patients are dependent for activities of daily living, resulting in an estimated cost of 45 billion euros in Europe.1,2 Moreover, its incidence is expected to increase by 34% by 2035, mainly due to population ageing.2 However, both the prevention and the acute rehabilitation treatment of this group of diseases have advanced considerably over the past 15 years, which has reduced sequelae and the rate of mortality due to AS.3
Specialised emergency neurological care provided by stroke units has been shown to improve the progression of patients with stroke.4,5 Treatment with intravenous alteplase (intravenous recombinant tissue plasminogen activator, rtPA) within the first 4.5 hours of symptom onset6 and endovascular treatment within the first 6-7 hours,7 with proven effectiveness and safety, have improved morbidity and mortality rates of AS, leading to significant changes in the organisation of stroke care. Admitting these patients to specialised neurorehabilitation units comprising multidisciplinary teams who exclusively treat brain damage has also reduced rates of mortality and sequelae, thus improving long-term functional prognosis.8
Considering the favourable geographical characteristics and population distribution in the province of Guipúzcoa, a centralised care model was established for AS at Hospital Universitario Donostia (HUD). Our hospital provides direct care to a population of 350 000 and is the tertiary referral centre for AS care for a population of 717 000 in the province of Guipúzcoa, receiving patients from 4 local hospitals: Bidasoa, Mendaro, Zumárraga, and Clínica de la Asunción in Tolosa. However, in 2015, 79.8% of patients discharged after ischaemic stroke and 87.8% after haemorrhagic stroke in the province are managed by different departments at HUD. In 2005, Arrazola et al.9 described the hospital care provided to patients with AS in Guipúzcoa. Their study identified a series of areas for improvement, including hospital arrival time of patients with AS and the consequent impact on the possibilities of acute treatment, and the limited amount of rehabilitation treatment received by patients during admission.9 Over the past 15 years, the neurology department at HUD, and specifically its stroke unit, has made significant changes both in the organisation and the care and treatment of patients with AS in the province of Guipúzcoa. Intravenous therapy was introduced at HUD in 2004; code stroke was implemented as a protocol 2 years later in the province of Guipúzcoa; and the stroke unit was inaugurated in 2009. In 2008, emergency multimodal CT had already been implemented, and intra-arterial treatment was introduced in 2011, with a neurointervention team available 24 hours per day, 7 days per week. Finally, a high-resolution clinic was established in 2013 for the outpatient management of low-risk transient ischaemic attack (TIA). During these years, close contact has been maintained between the different teams involved in the care of these patients, including the emergency, primary care, radiology, intensive care, neurosurgery, and rehabilitation departments.
After the implementation of this series of measures, which have improved the results of different patient groups, the present study aims to describe the care provided to patients with AS in the province of Guipúzcoa during the second half of 2015 (baseline clinical status, diagnosis and treatment, time to care, mortality, disability, dependence, and rehabilitation) in order to evaluate the results achieved as a consequence of all the measures implemented in the region over the past 15 years.
Material and methodsSelection criteriaWe conducted a retrospective, observational study of a sample of patients diagnosed with AS (ICD-9-CM codes 430-436, except for 43310) and discharged from any department of HUD in 2015. We included all patients discharged after an ischaemic stroke, haemorrhagic stroke, subarachnoid haemorrhage, cerebral venous thrombosis, subdural haematoma, or TIA. In order to obtain a similar sample size to that of Arrazola et al.9 in 2005 (of a sample of patients discharged in year 2000), we consecutively selected all patients discharged between August and December 2015 (n = 536).
Study variables and analysisWe included demographic variables (age; sex; history of arterial hypertension [AHT], diabetes mellitus [DM], or dyslipidaemia; drug habits; previous AS or heart disease; and relevant treatments including antiplatelet and anticoagulation therapy), time to hospital care and first neuroimaging study, diagnosis at discharge, treatment in the acute phase, complications during admission, functional status (modified Rankin Scale [mRS]), and mortality at discharge, as well as rehabilitation treatment (during admission and after discharge, and its different types: occupational therapy, physiotherapy, and speech therapy).
Subsequently, we analysed the overall mortality rate at one year, broken down by AS subtype. We also collected data on disability as measured by the Barthel index (BI) and the mRS. Data on the BI and mRS at 12 months were collected from the digital clinical history, when available, or by telephone.
Patient data were anonymised and extracted from the database of HUD’s stroke unit, in the case of patients admitted there, and from the digital clinical history, in the case of patients admitted to the general neurology ward or other departments at HUD (intensive care unit, neurosurgery, or internal medicine ward).
Statistical analysisDescriptive statistical analysis was conducted using version 21 of the SPSS software (IBM). Quantitative variables are expressed as mean and standard deviation, ordinal variables as median and interquartile range, and qualitative variables as the number of cases and percentage. We calculated means and standard deviations as well as percentages. We used a contingency table to break down the mortality rate by subgroup.
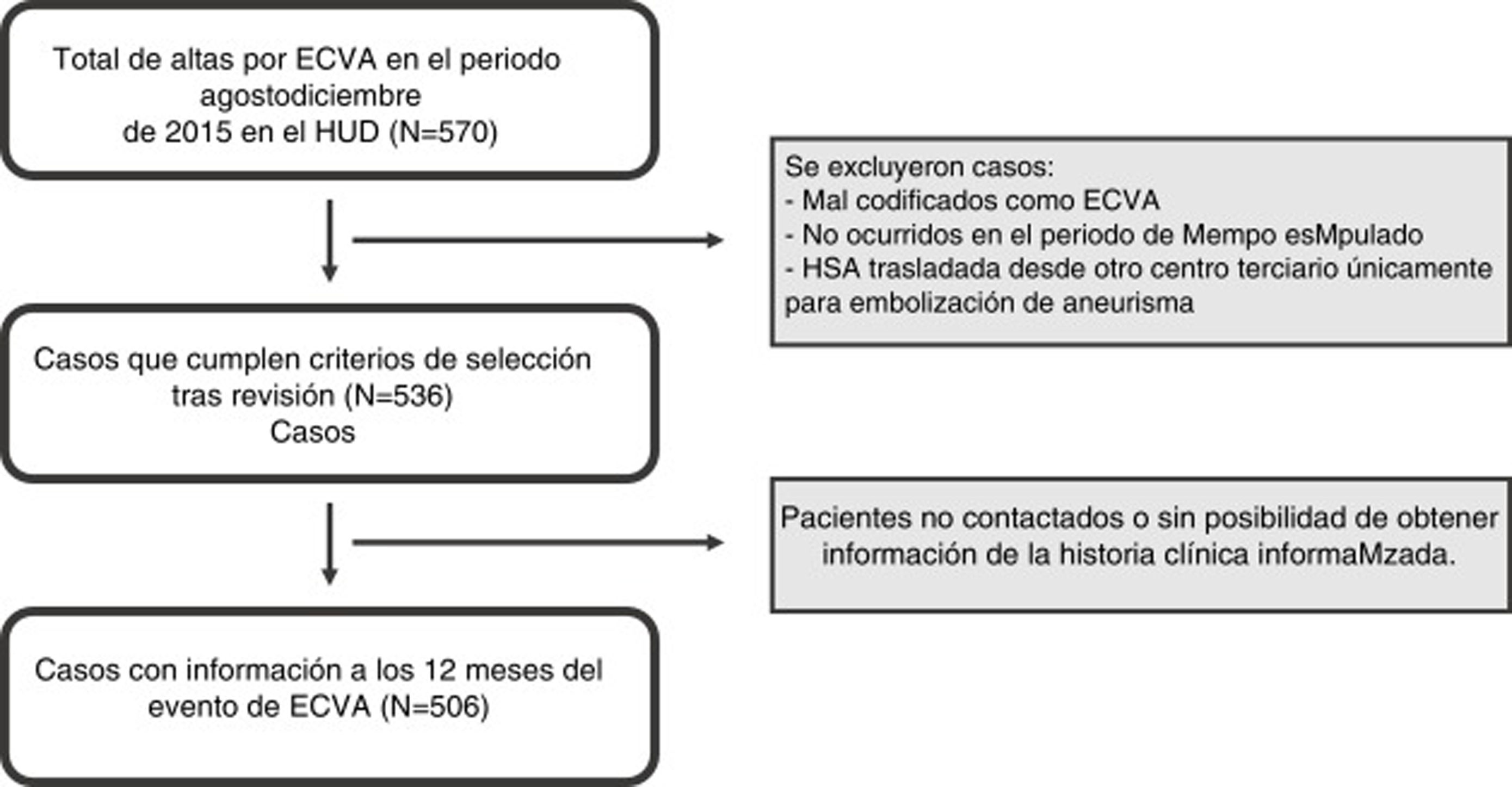
ResultsOf the 570 discharges identified at different HUD departments between August and December 2015, 536 met our inclusion criteria. Of these, 506 patients could be contacted or followed up at 12 months, as shown in Fig. 1. Given the characteristics of the centralised care model for AS in Guipúzcoa, of a total of 1294 discharges after ischaemic stroke in the whole province in 2015, 1023 (79.8%) were managed by HUD, including 929 at the neurology department (stroke unit or ward). Furthermore, of a total of 181 discharges after haemorrhagic stroke in Guipúzcoa, 159 were managed by HUD (87.8%).
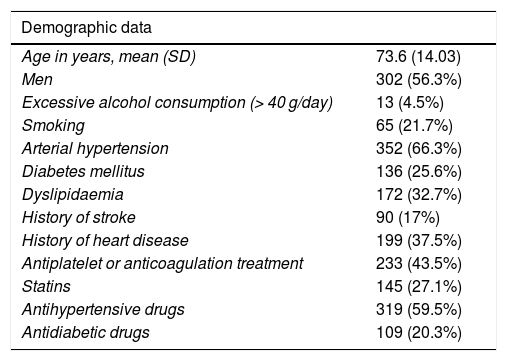
Mean age (standard deviation) was 73.6 (14.0) years; 56.3% (n = 302) of patients were men. Regarding medical history, 66.3% (n = 352) presented AHT and 25.6% (n = 136) DM. We also identified a large number of patients previously treated with antiplatelet or anticoagulation therapy (43.5%, n = 233), as shown in Table 1.
Demographic data, acute-phase treatment, complications, and rehabilitation treatment (n = 536).
| Demographic data | |
|---|---|
| Age in years, mean (SD) | 73.6 (14.03) |
| Men | 302 (56.3%) |
| Excessive alcohol consumption (> 40 g/day) | 13 (4.5%) |
| Smoking | 65 (21.7%) |
| Arterial hypertension | 352 (66.3%) |
| Diabetes mellitus | 136 (25.6%) |
| Dyslipidaemia | 172 (32.7%) |
| History of stroke | 90 (17%) |
| History of heart disease | 199 (37.5%) |
| Antiplatelet or anticoagulation treatment | 233 (43.5%) |
| Statins | 145 (27.1%) |
| Antihypertensive drugs | 319 (59.5%) |
| Antidiabetic drugs | 109 (20.3%) |
| Acute-phase treatment | |
|---|---|
| Pharmacologicala | 324 (60.4%) |
| Systemic thrombolysisb | 29 (8.3%) |
| Endovascular treatmentb | 38 (10.9%) |
| Direct | 27 |
| Secondary | 11 |
| Surgical | 15 (2.8%) |
| Haemorrhagic AS | 13 (12.1%) |
| No | 130 (24.3%) |
| Complications and rehabilitation | |
|---|---|
| Total complications | 23.9% |
| Rehabilitation | 59% |
The emergency department assessed 53% (n = 284) of patients with AS within 6 hours of symptom onset, and performed a neuroimaging study within the same timeframe in 49.8% (n = 267) (Appendix, supplementary Table 1). Code stroke was activated in 37.1% (n = 195) of cases. Two hundred and eighty (52.2%) patients with AS were admitted to the stroke unit, 54 (10.1%) to the intensive care unit, and 202 (37.7%) to a hospital ward (the neurology ward in 99% of cases).
Ischaemic stroke accounted for 64.9% (n = 347) of admissions, followed by haemorrhagic AS with 20% (n = 107) of cases. Discharges after TIA represented 14.8% (n = 79).
In our series, 8.3% (n = 39) of patients discharged after ischaemic stroke received intravenous treatment (fibrinolysis), whereas 10.9% (n = 38) received endovascular treatment (27 cases of direct mechanical thrombectomy and 11 cases of secondary mechanical thrombectomy following intravenous treatment). Of the total number of patients discharged after haemorrhagic AS, 12.1% underwent surgery. In-hospital complications were recorded in 23.9% (n = 128) of cases, and 59% (n = 300) received rehabilitation treatment during admission (Table 1). Fifty-six percent of patients started rehabilitation treatment during admission. At discharge, 30.5% of patients were transferred to a rehabilitation centre and 0.5% to an intensive rehabilitation centre, and 8% continued receiving rehabilitation in an outpatient basis. Seventy-one percent of patients received physiotherapy only, with 5% receiving speech therapy, 1% occupational therapy, and 22% a combination of rehabilitation techniques.
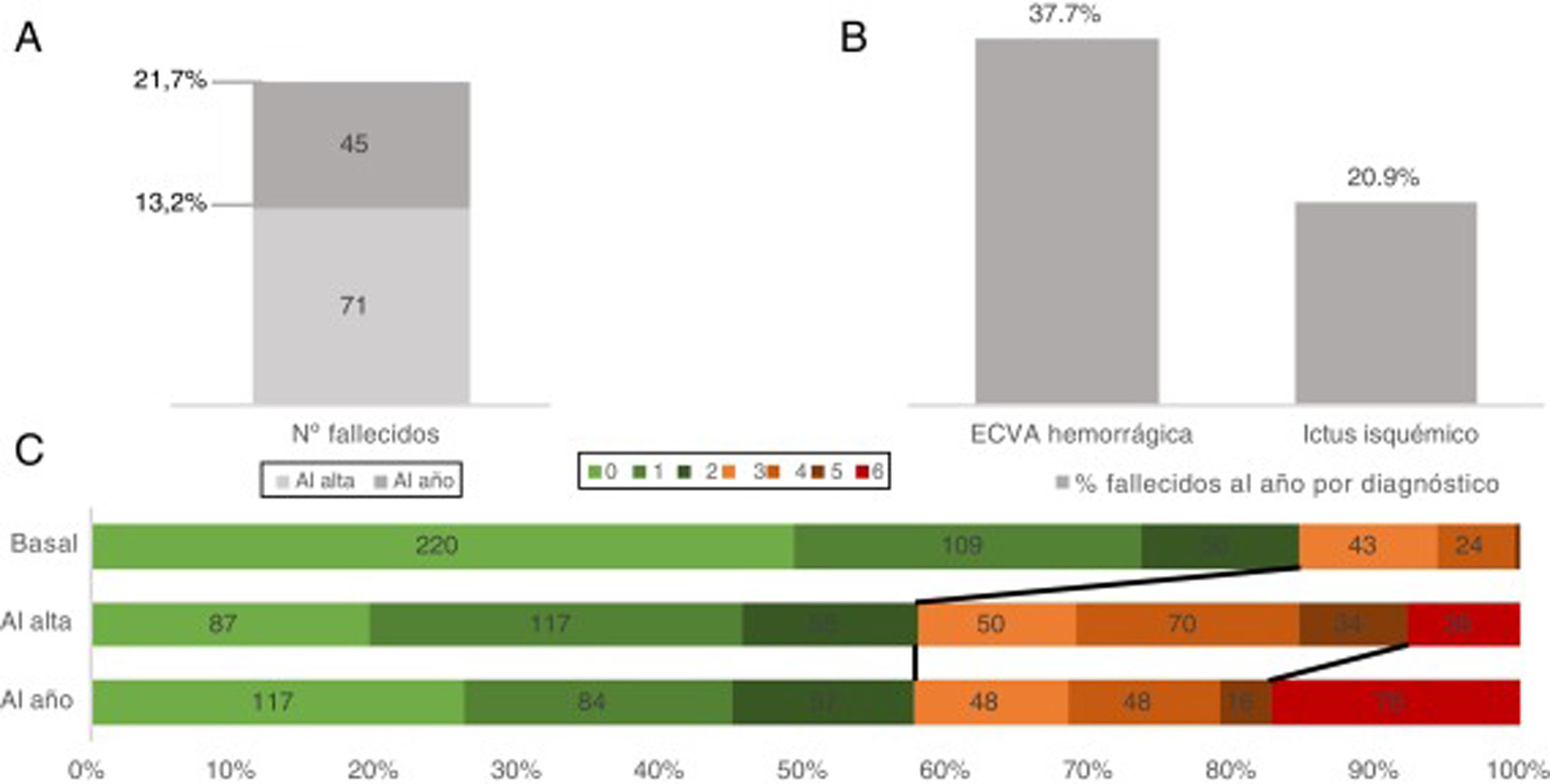
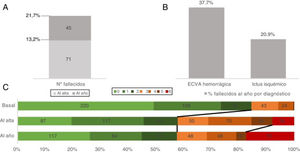
Finally, mortality at discharge was 13.2% (n = 71), with a 12-month mortality rate of 21.7% (n = 116). By AS subtype, 12-month mortality was lower for ischaemic stroke than for haemorrhagic AS (20.9% vs 37.7%, respectively) (Fig. 2). At 12 months, 62.5% (n = 335) of patients were independent or presented slight dependence (BI 95-100), 19.7% (n = 106) moderate independence (BI 60-90), and 17.7% (n = 95) severe dependence (BI 0-60) (Appendix, supplementary Fig. 1). According to the mRS, 50% (n = 268) of patients were independent (mRS 0-2), 23.1% (n = 124) showed some degree of disability (mRS 3-5), and 21.7% (n = 138) had died (mRS 6). Fig. 2 shows the progression of disability at admission, at discharge, and at 12 months.
A) Overall mortality due to acute stroke (absolute numbers) at discharge and at 12 months. B) Percentage of deceased patients by diagnosis. C) Disability (as measured by the modified Rankin Scale) at admission, at discharge, and at 12 months, only for patients for whom data were available for all 3 variables (n = 488).
Time to acute care was one of the main areas for improvement mentioned by Arrazola et al.9 in their 2005 study on hospital care for AS in a sample of patients discharged in the year 2000 in Guipúzcoa.9 In 2015, 53% of patients with AS were assessed by the emergency and neurology teams at HUD’s emergency department, within 6 hours of symptom onset, with a neuroimaging study performed within 6 hours of symptom onset in 49.8%. The implementation of code stroke has been shown to improve time to care for AS10,11; this effect has been observed in Guipúzcoa, if we compare the number of patients attended in the emergency department within 6 hours to the results published by Arrazola et al.9 Since code stroke was activated in less than half of cases (37.1%), it is likely that such other factors as better coordination and detection of cases by different emergency departments and local hospitals, as well as stroke awareness campaigns, may have helped to reduce time to care for AS, as is the case in other regions.12,13 Whereas in the year 2000, fibrinolysis would have been ruled out in an alarming number of patients (92.2%) simply due to the delay in arriving at the emergency department and undergoing a brain CT, 30.5% of patients with AS underwent a brain CT within 3 hours in 2015. In fact, 8.3% of patients with ischaemic stroke received intravenous treatment in Guipúzcoa in 2015, a similar percentage to that reported in other European countries including Germany and the United Kingdom (9.5% and 12.2%, respectively).2 Furthermore, 10.9% of patients with ischaemic stroke received endovascular treatment, which was direct in almost 70% (n = 27). The centralised model that the province of Guipúzcoa opted to implement at HUD may also have had an impact on the improvement of times to care and, therefore, on access to acute interventions. In 2015, Ramsay et al.14 reported a reduction in the time to care and improved access to acute interventions between 2008 and 2012, after the implementation of a centralised model in London and Manchester, as compared to urban areas in England where stroke care was not centralised.14
Also, the 2005 study underscored the low percentage of patients receiving rehabilitation treatment during hospitalisation (9.2%).9 The percentage of patients with AS receiving in-hospital rehabilitation treatment was 56% in 2015, with physiotherapy or a combination of different therapies being the most frequently adopted treatment for rehabilitation (93% in general). At discharge, 39% continued receiving rehabilitation treatment, frequently on an inpatient basis (Table 1).
Lastly, we observed that the overall mortality at discharge after AS in 2015 amounted to 13.2%, a figure similar to that mentioned in The Burden of Stroke in Europe report, which observed a mortality rate of 14% in patients admitted due to ischaemic stroke in the United Kingdom in 2015-2016, for instance.2 Mortality at 12 months was 21.7%, lower than that reported in previous studies15,16 (approximately 30% between 2000 and 2009).18 Mortality at 12 months was also lower than that reported in Guipúzcoa in 2000, both globally and for each AS subtype (2015 vs 2000: overall, 21.7% vs 25.9%; ischaemic stroke, 20.9% vs 25.3%, and haemorrhagic AS, 37.7% vs 47.5%).9 This seems not to be associated with increased morbidity, as the percentage of patients who were independent or presented slight dependence (BI 95-100) at 12 months remained similar (Appendix, supplementary Fig. 1). Furthermore, the baseline characteristics of our sample would be indicative of poorer prognosis and outcomes if no changes had been made to care for AS. Mean age (standard deviation) of the patients discharged after AS in 2015 was 73.6 (14) years, similar to that described in the same setting in 2000,9 as well as in population-based cohort studies that described ages between 69 and 72 years.17,18 However, the number of patients with previous comorbidities does seem to have increased when we compare data between samples from the years 2000 and 2015,9 despite patient selection having been practically identical in both studies. This is particularly relevant if we consider the importance of such factors as AHT and DM in AS risk and prognosis.18 Furthermore, whereas discharges after TIA represented 22.8% of the total in the sample of patients with AS in 2000,9 they amounted to 14.8% in 2015. This decrease is probably explained by the outpatient management of TIA in selected cases (according to the ABCD2 score and assessment of electrocardiogram rhythm),19 resulting in a higher proportion of patients discharged after ischaemic stroke and haemorrhagic AS in the 2015 sample.
Limitations of our study include the retrospective nature of data collection and the fact that some patients were lost to follow-up at 12 months. The patient sample is heterogeneous due to the non-restrictive selection criteria we used, aiming to select all patients attended due to AS at HUD. These selection criteria are also similar to those previously used in Guipúzcoa. Thus, despite these limitations, we are able to compare our results not only against current data from other centres, but also against data previously reported for this province.
ConclusionsAfter the implementation of strategic modifications to AS care in Guipúzcoa, including the centralised care model at HUD, rates of mortality at discharge and at 12 months are lower in 2015 than in previous years. Furthermore, more than half of patients are independent or present only mild disability or dependence at 12 months. These results are consistent with the objectives and results published by other Spanish and European centres.
Conflicts of interestThe authors have no conflicts of interest to declare. This study did not receive funding.
Please cite this article as: Fernández-Eulate G, Arocena P, Muñoz-Lopetegi A, Rodriguez-Antigüedad J, Campo-Caballero D, Equiza J, et al. Atención a la enfermedad cerebrovascular aguda en Guipúzcoa: descripción de los resultados de un hospital de referencia en un modelo de atención centralizado. Neurología. 2022;37:355–361.